An estimated 17-million women in the U.S. and nearly 370 million women across the globe suffer from a condition known as Lipedema. What is regularly associated with rapid and uncontrollable weight gain in its initial stages can quickly spiral out of control if left undiagnosed. Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate in comparison to the rest of the body, and progression typically begins with puberty.
Lipedema is often misdiagnosed and dismissed by medical professionals as simple obesity, leaving affected women to deal with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses. Ultimately, effective treatment can require surgical reduction in order to alleviate the appearance and pain of symptoms. Lipedema reduction surgery is similar to liposuction and is performed on the affected limbs and is generally the most effective form of treatment. Removing fat deposits that are diseased not only helps reduce swelling of the limbs but alleviates the pain that holds patients back from everyday activities.
For one 41-year old woman with Stage 3 Lipedema progression, the misdiagnosis of Lipedema as obesity led to protein and calorie malnutrition and ultimately required hospitalization and parenteral nutrition. Through this time, despite high levels of malnutrition, her legs remained swollen and enlarged, which ultimately (and finally!) led to a correct lipedema diagnosis after decades of unsuccessful treatments focused on traditional obesity.
What Happened at Stage 3 Lipedema?
This 41-year-old woman noticed increased fat in her legs as early as 12 years old. Her weight and leg size increased through the age of 21, by which time she reached a maximum weight of 165 kg (363 lbs) and underwent a gastric bypass surgery.
Over the following 12 months, she lost 74.8 kg (165 lbs). The trunk of her body experienced significant weight loss, while her lower body and legs remained the same. Fifteen years later, during recovery from hysterectomy surgery, she became progressively weaker and swollen over her entire body. Laboratory test results showed hypoalbuminemia (2.0 g/dL), lymphopenia, and hypolipoproteinemia. Hypoalbuminemia and lymphopenia are not commonly seen in developed countries where famine is rare. In developed countries, hypoalbuminemia levels this low are often thought to be caused by liver failure, lymphopenia is a sign of some kind of severe disease or infection but in this case it was malnutrition. Similarly, hypolipoproteinemia refers to unusually low levels of fats (lipids) in the blood, which may be caused by rare genetic conditions or be a sign of another disorder such as overactive thyroid, anemia, cancer, chronic infection, or impaired absorption of foods from the digestive tract but again in this case was undernutrition.
At this time, she was diagnosed with protein and calorie malnutrition with marked gut edema (swelling), requiring prolonged parenteral nutrition as she was unable to consume her meals orally on her own. After restoration of normal protein and nutrition, her health returned and her pitting edema resolved, but her extremities remained enlarged. She was subsequently diagnosed with lipedema and was able to seek proper treatment.
Why is Misdiagnosis so Common?
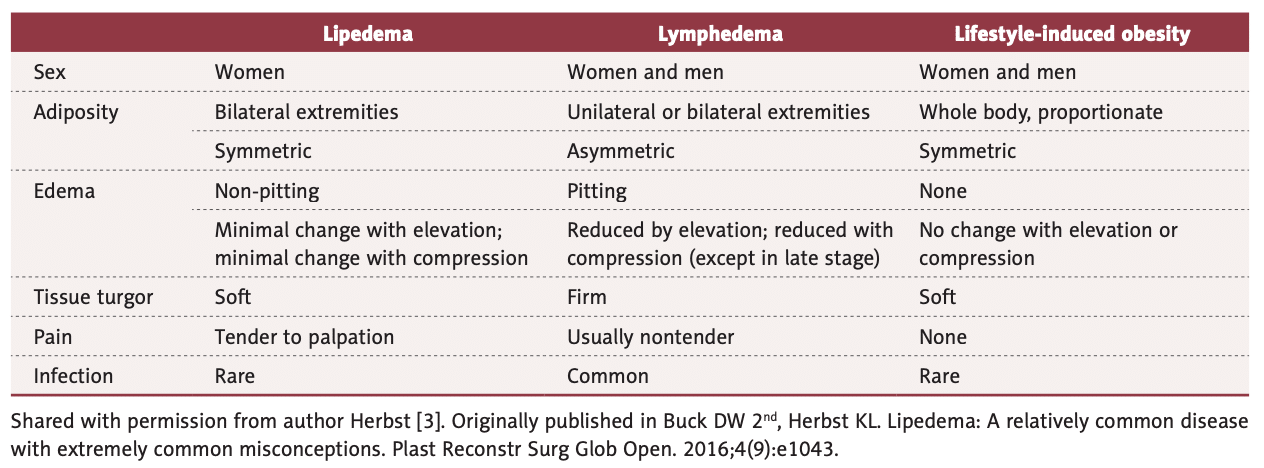
Getting an initial Lipedema diagnosis is a challenge for many women suffering from it. In fact, an overwhelming majority of patients seeking treatment – like the woman in this case – are well into their forties, fifties, sixties, or later in age, simply because they had never heard of lipedema or been diagnosed with it. After decades of being diagnosed with a high Body Mass Index (BMI) followed by a general obesity diagnosis or misdiagnosed as lymphedema, some of these women with lipedema sought alternate explanations for their pain, discomfort, and unsuccessful weight loss, despite regular diet, exercise, and, in some advanced cases, even after undergoing bariatric surgery.
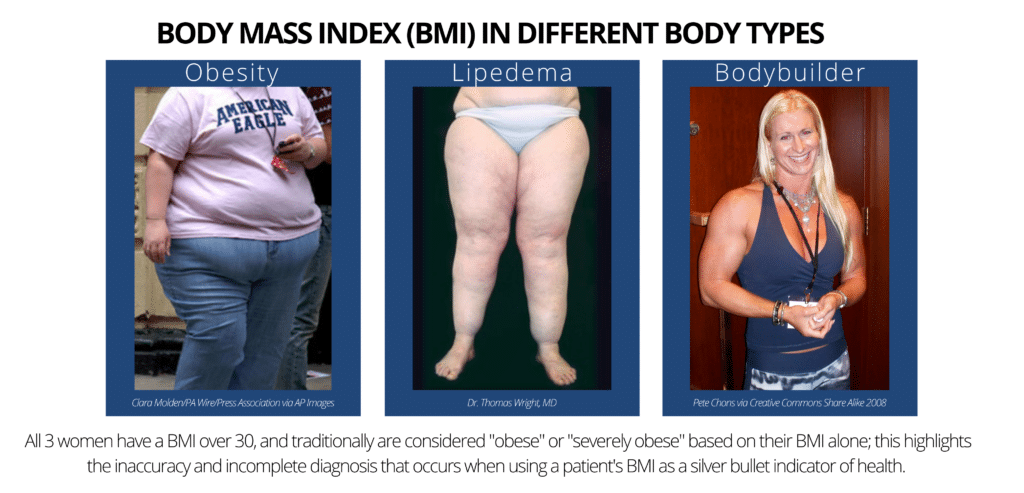
The Body Mass Index (BMI) calculation is an unfortunate oversimplification of a person’s health, and ignores extremely important factors that are imperative for accurate diagnosis and treatment plans. Family history and genetics, general lifestyle and activity levels, age, gender, and body composition (muscle mass, water content, bone mass) are all essential parts of our health profile, all of which are ignored by the BMI calculation.
Despite all of this, it continues to be used worldwide to aid in diagnosing (or misdiagnosing and oversimplifying) patient health profiles. As we see here, this misdiagnosis has the opportunity to become dangerous and life threatening in some instances, and at best leaves patients with Lipedema in pain and a poor quality of life. To read more about the woman in this case study you can find her story here. Be sure to contact us today!
References
Wright TF, Herbst KL. A 41-Year-Old Woman with Excessive Fat of the Lower Body Since Puberty with Progression to Swollen Ankles and Feet Despite Caloric Restriction, Due to Lipedema and Protein-Calorie Malnutrition: A Case of Stage 3 Lipedema. Am J Case Rep. 2021;22:e930306. Published 2021 May 7. doi:10.12659/AJCR.930306

