Lipedema is a loose connective tissue disease that causes disproportionate subcutaneous fat accumulation on the extremities. As a result of the increased subcutaneous tissue accumulation, lipedema is often confused with obesity by both physicians and patients. Poor awareness and limited diagnosis of lipedema contribute to the confusion of lipedema with obesity and can lead to decreased body image acceptance. Patients with lipedema may have anorexia nervosa, an eating disorder characterized by a distortion of body image, incorrect self-identification of being overweight, restricted eating behavior, and a relentless pursuit of weight loss. Read on to learn how lipedema and anorexia are linked with each other.
How are Lipedema & Anorexia Linked?
In a case report published in the American Journal of Case Reports, a young woman with disproportionate fat accumulation on the lower half of her body self-identified as having obesity. Her self-identification is not uncommon, given that even medical professionals often misdiagnose women with Lipedema as having obesity, and provide treatment plans assuming as much. The women in this study developed restrictive eating behavior and became obsessed with weight loss, ultimately undereating, becoming malnourished, then resulting in anorexia nervosa. To add insult to injury, the woman’s lower body remained swollen and did not experience weight loss because abnormal Lipedema fat is resistant to diet and exercise, even at extreme levels that cause anorexia, and in this case anorexic lipedema.
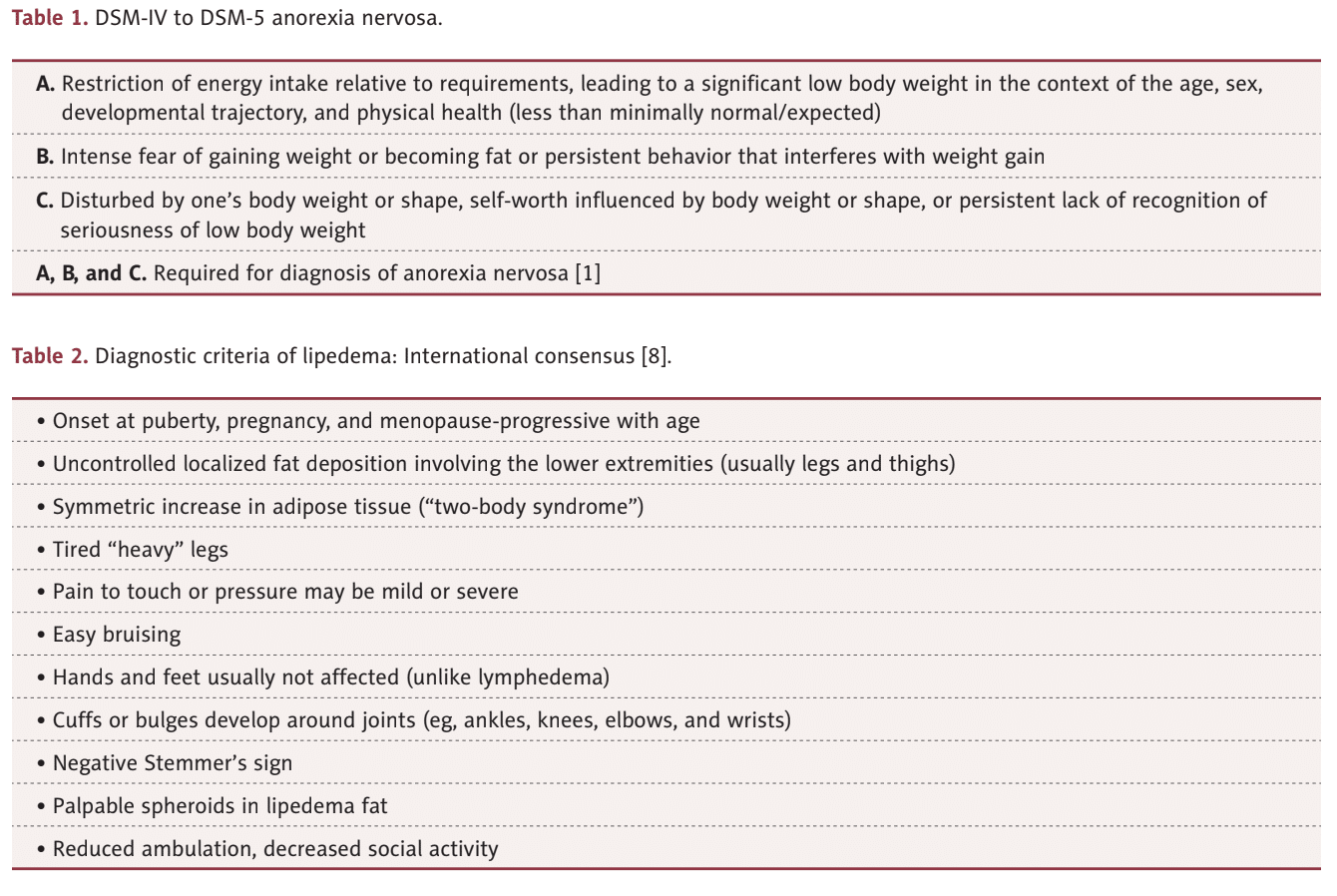
The lack of recognition of lipedema by medical professionals and the public as a weight loss-resistant disease can affect body image acceptance. Lipedema was mistaken for obesity by the young woman in this case and likely played a role in her development of an eating disorder. Eating disorders, such as anorexia nervosa, are not rare and may be more common in women with lipedema, which is called anorexic lipedema.
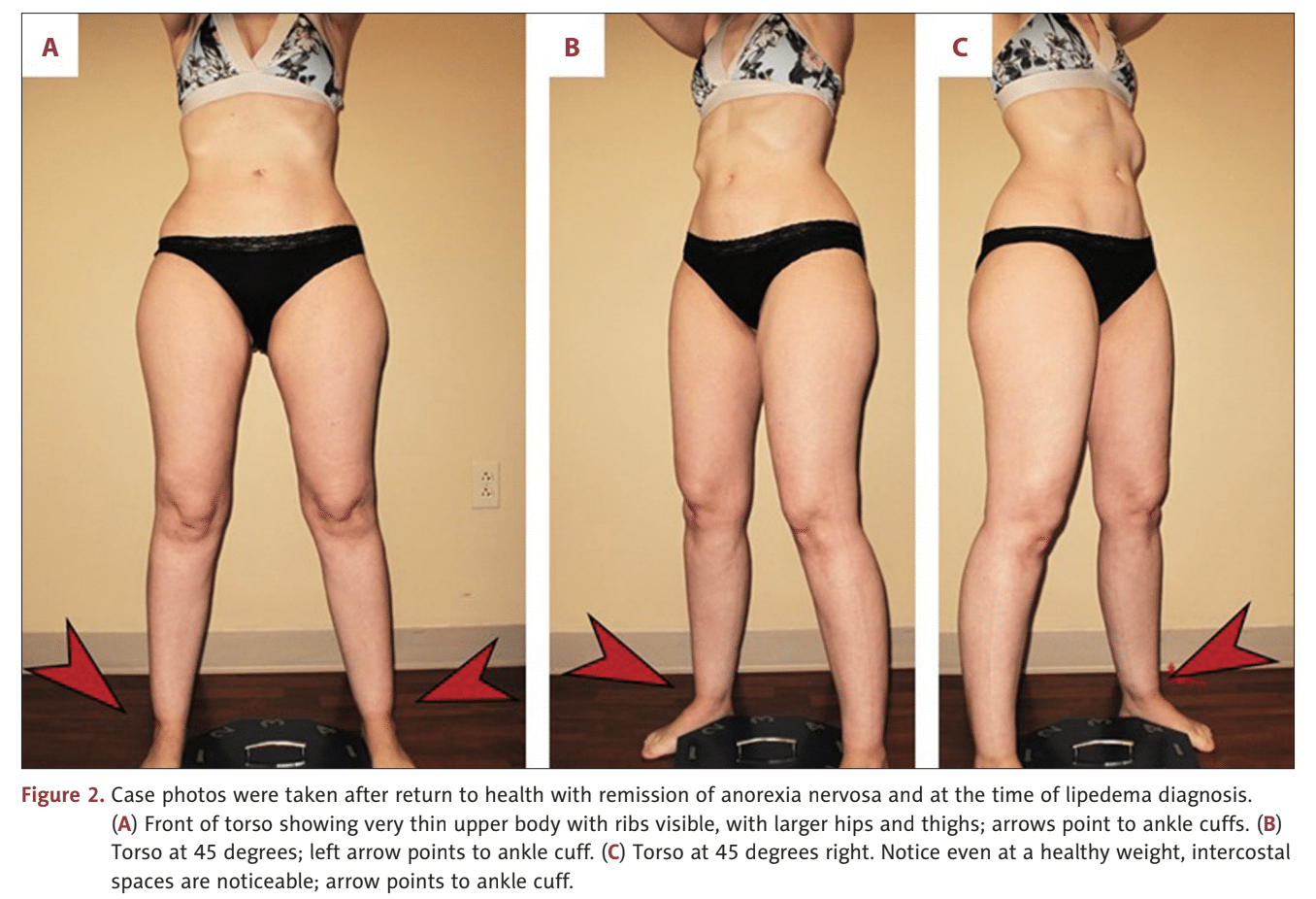
Her disproportionate subcutaneous tissue persisted despite losing weight to reach a BMI of 15 kg/m2 . After a decade-long struggle, her eating disorder resolved, and she maintained a healthy weight and BMI of 21.5 kg/m2 but disproportionate fat remained in her lower body. She experienced increasing leg tenderness, pain, and easy bruising and was diagnosed with lipedema.
Lipedema vs. Obesity Using BMI
Because Body Mass Index (BMI) is a calculation that illustrations the relationship between a person’s weight and height, it equips healthcare providers with one tool in evaluating a patient’s overall health. Specifically, these ranges are used to categorize whether a person is underweight, in a normal weight range, overweight, or obese. While BMI does not provide the full picture of a patient’s health or the full body composition breakdown, it is a commonly used factor in diagnosing numerous diseases.
Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, and in many cases, excessive clustering of fat cells is noticed in the arms as well.
However, Lipedema causes fat in a different proportion on the body and has a different metabolic, chemical, and mechanical effect. Both obesity and Lipedema have increased BMIs, but they are not one and the same. When we use BMI as a blanket for Lipedema diagnosis, it’s an unfair and incomplete assessment.
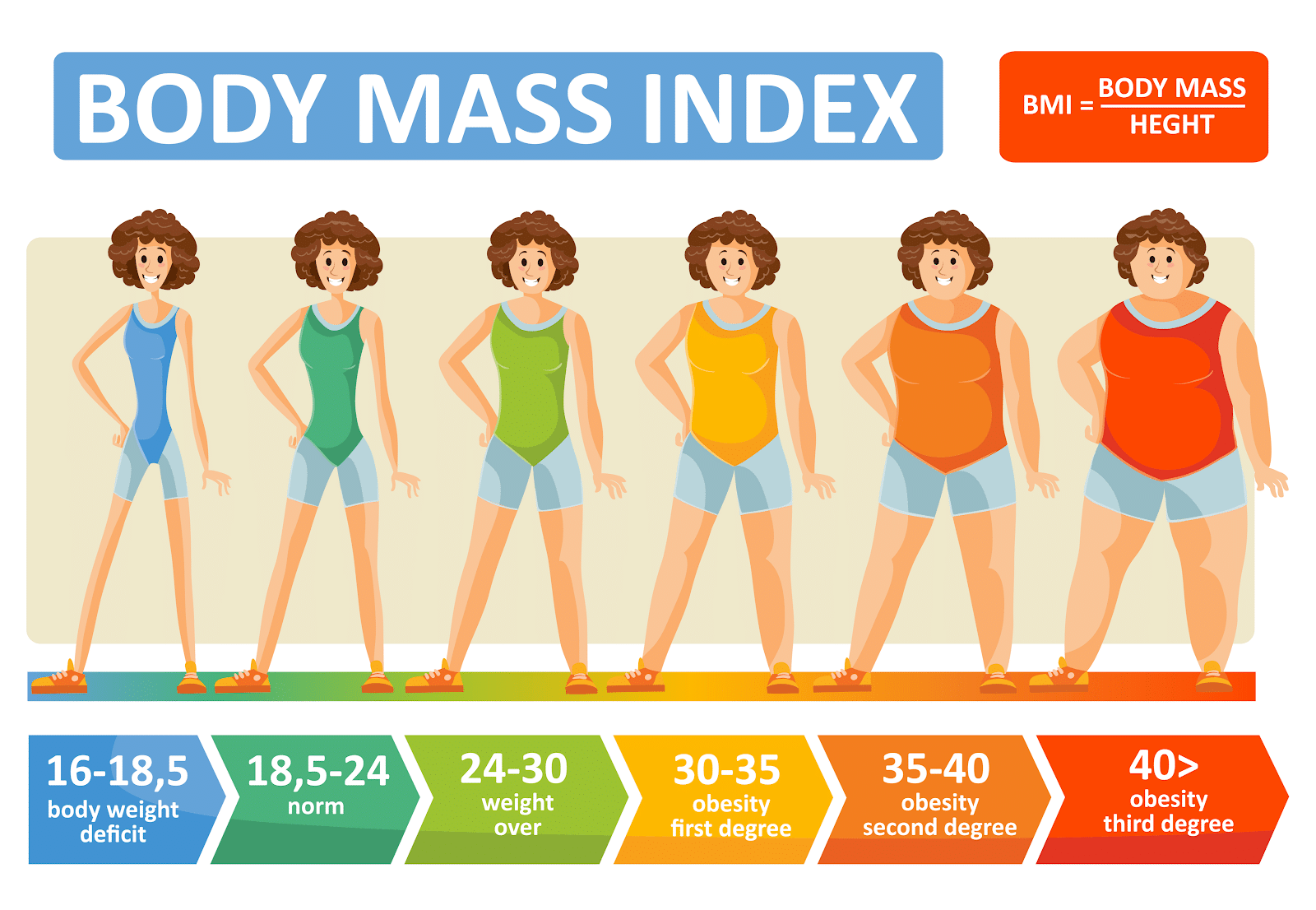
Lipedema is metabolically the opposite of obesity – both are associated with excess fat accumulation, however, obesity presents with fat accumulated in the central area of the body, primarily in the abdomen, and is associated with diseases such as diabetes, high blood pressure, high cholesterol, and cardiovascular disease. However, lipedema presents with peripheral fat in the extremities, while the abdomen and/or waist are typically unaffected. But because both diseases increase a patient’s BMI, misdiagnoses are common and destructive. This illustrates one reason why BMI is not a biologically valid way to diagnose obesity or lipedema.
This clinical case shows how poor understanding and recognition of lipedema can play a role in the self-identification of being overweight or obese. Lipedema is often associated with higher body weights and BMI, but this case shows lipedema can be present in underweight women too! You can read the full case study here. Be sure to contact us today!
References
Wright TF, Herbst KL. A Young Woman with Excessive Fat in Lower Extremities Develops Disordered Eating and Is Subsequently Diagnosed with Anorexia Nervosa, Lipedema, and Hypermobile Ehlers-Danlos Syndrome. Am J Case Rep. 2021 Jun 14;22:e930840. doi: 10.12659/AJCR.930840. PMID: 34121088.
https://pubmed.ncbi.nlm.nih.gov/34121088/
https://www.amjcaserep.com/download/index/idArt/930840
