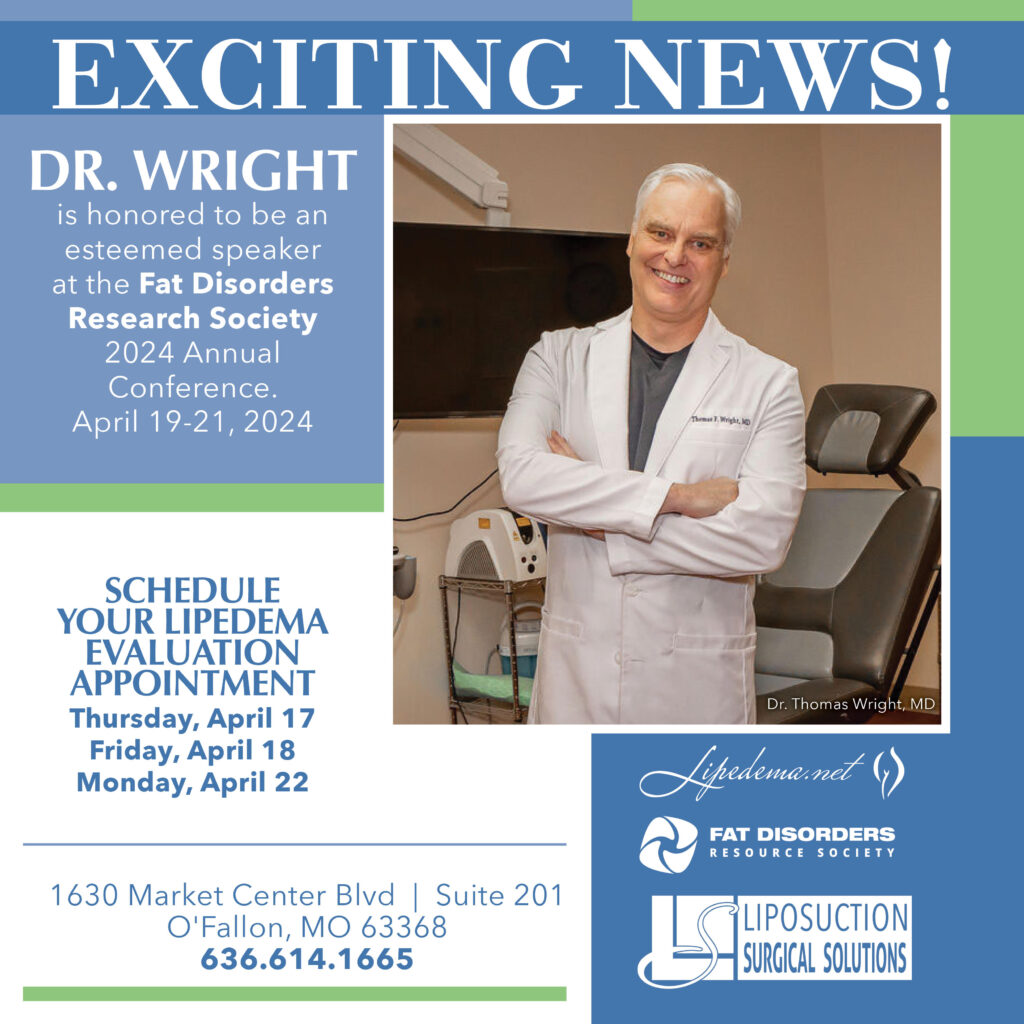
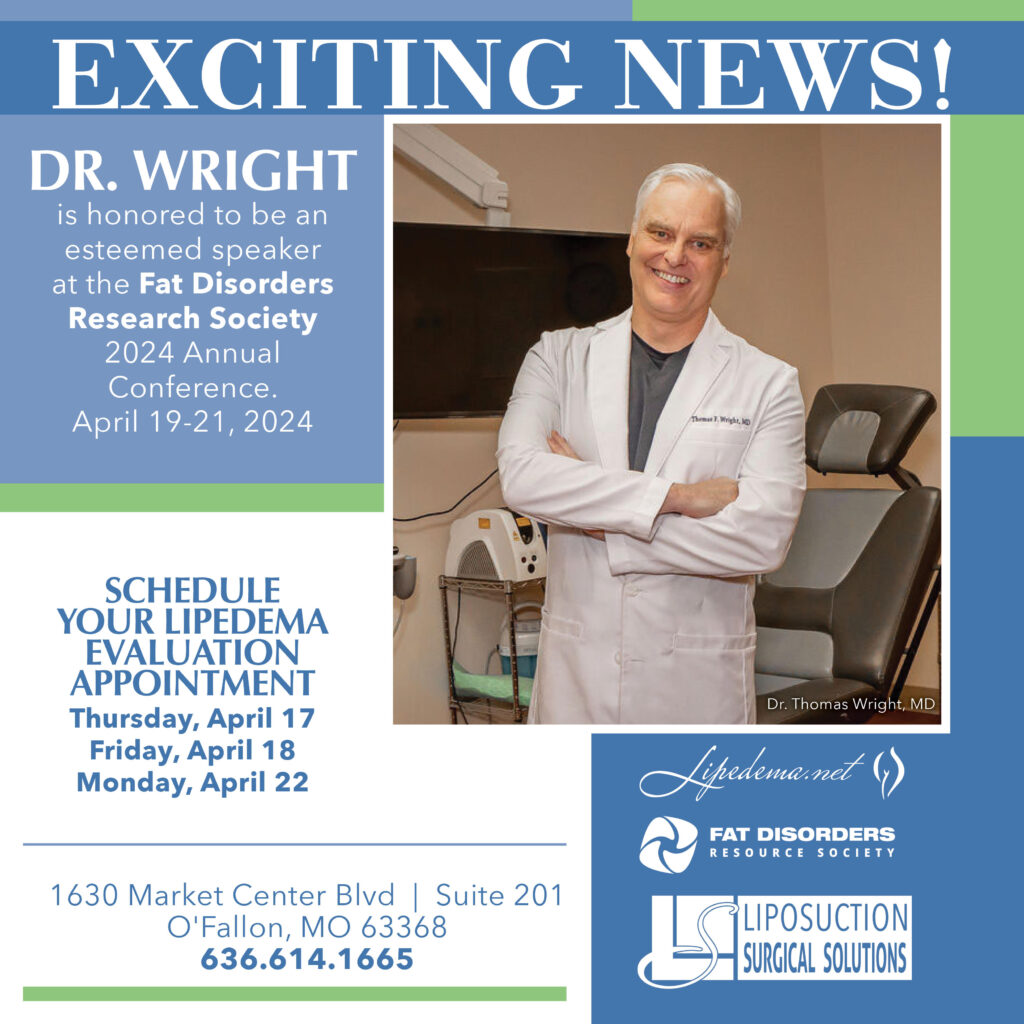
Lipedema, a chronic condition marked by the disproportionate accumulation of fat in the legs and arms, has perplexed and challenged the medical community for decades. Originating from the pioneering observations of Drs. Allen and Hines in 1940, the journey of lipedema treatment has evolved dramatically, from rudimentary recommendations of diet and compression stockings to groundbreaking surgical interventions. Dr. Wright’s upcoming talk with the Fat Disorders Resource Society (FDRS) from April 19-21 promises to shed light on this transformative journey and highlights the innovative strides in treating this often misunderstood disease.
Lipedema, characterized by pain, swelling, and an increased susceptibility to bruising, has long posed significant challenges in diagnosis and management. Traditional management strategies, while providing relief, often fell short of addressing the progressive nature of lipedema, leading many to live with unresolved pain and mobility issues. The condition’s overlap with lymphedema further complicated treatment approaches, necessitating a nuanced understanding of the lymphatic system’s involvement.
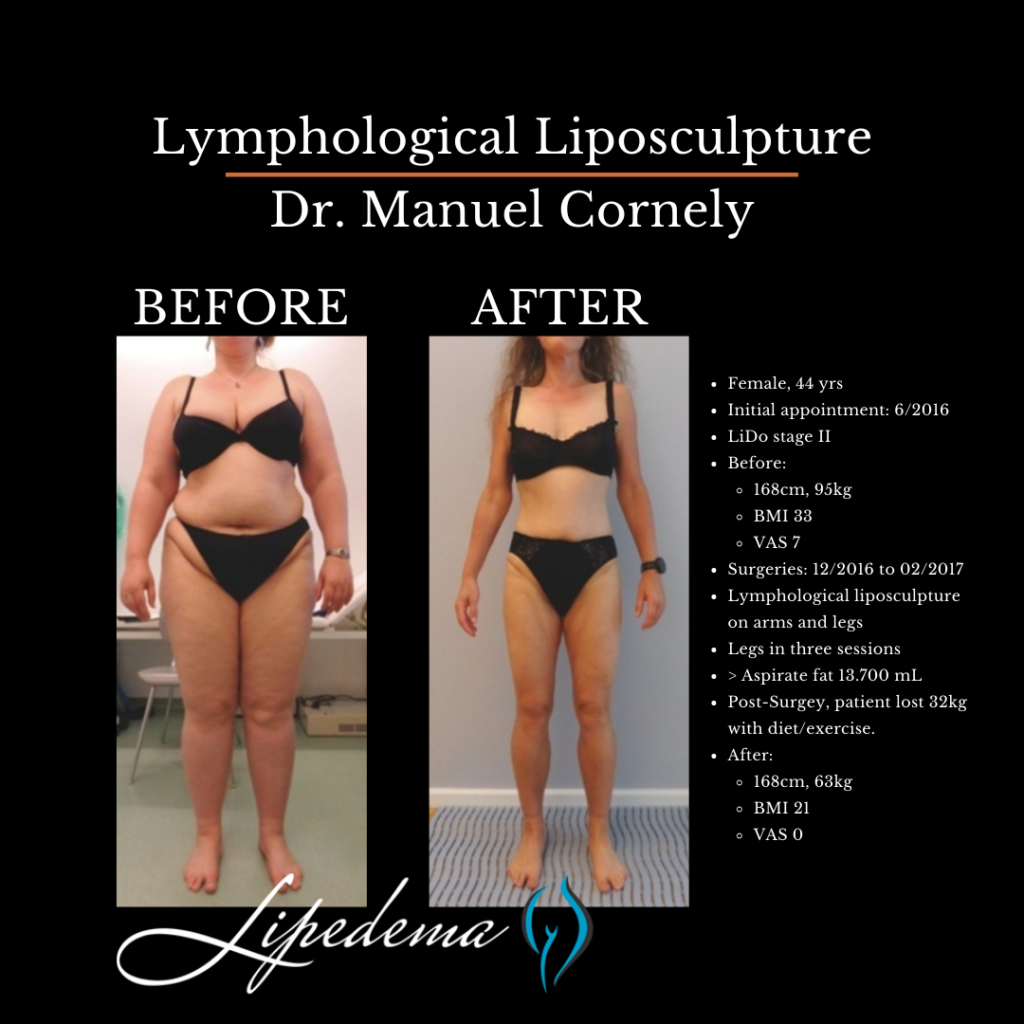
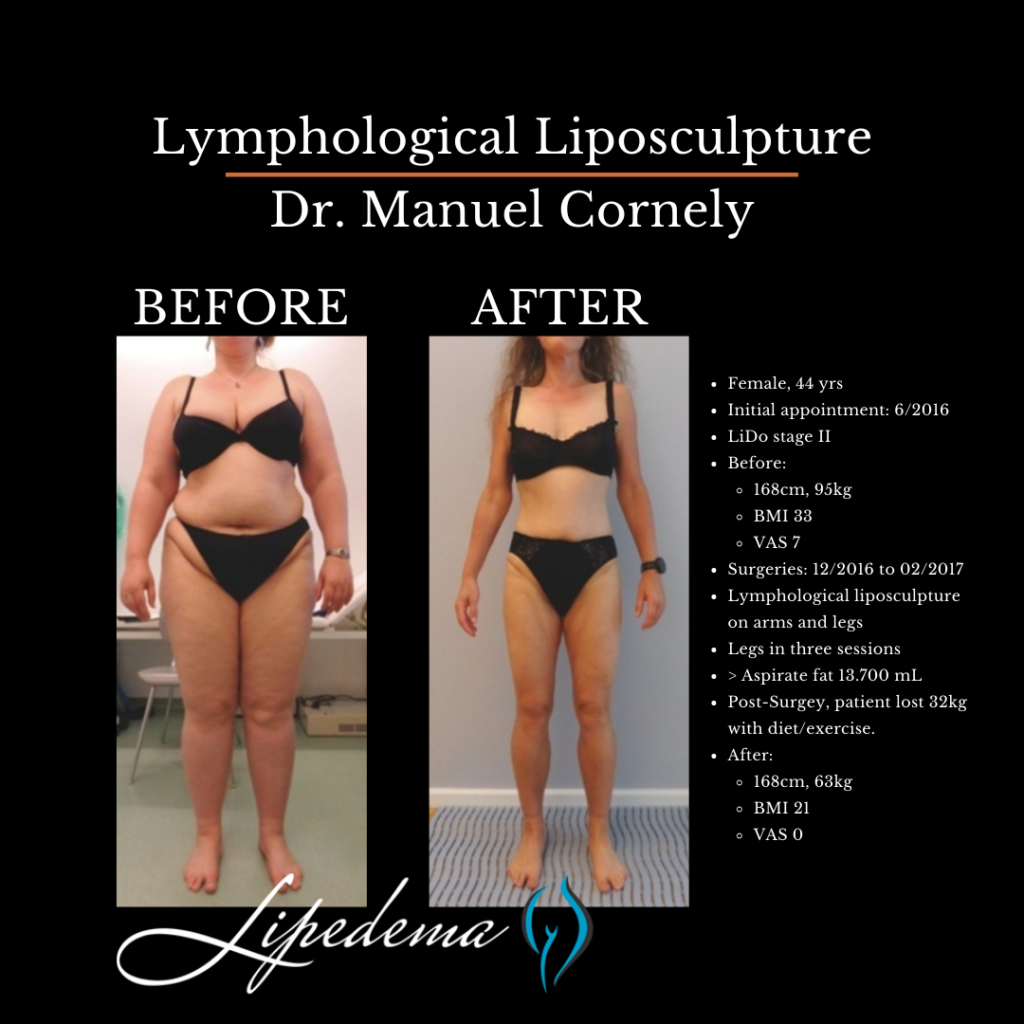
The 1990s marked a pivotal era in lipedema treatment. The introduction of the tumescent liposuction technique by Dr. Jeff Klein, which minimized blood loss and reduced surgical risks, set the stage for a new therapeutic approach. Dr Gerhard Sattler spent time with Dr Klein, bringing the new techniques to Germany. Dr. Gerhard Sattler’s pioneering efforts, alongside his colleagues, Drs. Stefan Rapprich and Manuel Cornely demonstrated the potential of liposuction in providing significant relief for lipedema patients. Despite early successes, concerns regarding potential lymphatic damage loomed, sparking heated debates within the medical community. The first abstract publication of the surgical reduction of lipedema was in 2002 from the Paris Dermatology Conference.
Lymphologists who focus on diagnosing and treating lymphedema were concerned with surgery for lipedema-causing lymphedema. Surgery, Trauma, and Radiation therapy can cause lymphedema. Lipedema women have an increased risk of developing lymphedema. The lymphologists who were treating lymphedema patients caused by liposuction and related surgeries were up in arms about the potential for lipedema surgery to cause more lymphedema. The controversy surrounding liposuction for lipedema underscored the need for meticulous technique and a deeper understanding of lymphatic anatomy. Studies conducted in the late 1990s and early 2000s meticulously examined the effects of liposuction on the lymphatic system, eventually paving the way for techniques that preserved lymphatic integrity while effectively reducing lipedema symptoms.
The Fat Disorders Resource Society (FDRS) has been instrumental in advancing the cause of individuals suffering from lipedema and related conditions. By fostering education, research, and advocacy, FDRS plays a critical role in raising awareness, improving patient outcomes, and supporting the development of effective treatments. Dr. Wright’s collaboration with FDRS underscores a shared commitment to enhancing the quality of life for those affected by fat disorders through education and innovative care.
The evolution of lipedema treatment through liposuction, particularly lymph-sparing techniques, represents a significant leap forward. Early adopters of these methods demonstrated remarkable improvements in symptoms, reduced need for ongoing conservative treatments, and a marked enhancement in patients’ quality of life. These findings, bolstered by subsequent studies, underscore liposuction’s role as a viable, long-term solution for managing lipedema.
Dr. Wright’s upcoming talk with FDRS is more than a historical overview of lipedema treatment; it’s a testament to the relentless pursuit of better outcomes for lipedema patients. By highlighting the journey from conservative management to surgical innovation, Dr. Wright emphasizes the importance of continued research, patient education, and multidisciplinary collaboration in tackling lipedema.
Through this dialogue, Dr. Wright and FDRS aim to empower patients and healthcare professionals alike, offering hope and direction in the ongoing battle against lipedema. The discussion will not only explore the milestones in lipedema treatment but also illuminate the path forward, emphasizing the necessity of accessibility to effective treatments and the ongoing need for advocacy and support.
As we anticipate Dr. Wright’s insightful presentation, it is crucial to recognize that the journey of lipedema care is far from complete. The collaboration between healthcare professionals and organizations like FDRS highlights the dynamic nature of lipedema research and treatment, underscoring the need for continued vigilance, innovation, and compassion in addressing this condition.
Armed with knowledge and support, Lipedema patients can navigate their treatment options with greater confidence, advocating for care that not only alleviates symptoms but also enhances their overall well-being. The dialogue between Dr. Wright and FDRS serves as a beacon of hope, driving home the message that significant strides in lipedema care are possible and within reach with perseverance and collaboration.
The history of treating lipedema is a narrative of challenge, innovation, and hope. Dr. Wright’s forthcoming talk with FDRS promises to be a profound exploration of this journey, shedding light on the milestones that have shaped lipedema care and the promising horizon of treatments. As we look forward to this event, let us rally behind the ongoing efforts to improve the lives of those affected by lipedema, inspired by the knowledge that together, we can make a difference. Through education, research, and advocacy, we can continue to push the boundaries of what is possible in lipedema treatment, ensuring that every individual has access to the care and support they deserve.
Navigating the healthcare system can be a daunting task, especially when seeking treatment for conditions like lipedema. Recognized for its complexity and often misdiagnosed, lipedema is a chronic condition characterized by an abnormal accumulation of fat cells in the legs and arms, leading to pain, swelling, and mobility issues. As we observe World Lymphedema Day in March, it’s an opportune time to shed light on the importance of understanding and managing lipedema, including the critical aspect of securing insurance coverage for its treatments.
Lipedema is often misunderstood and can be mistaken for obesity or lymphedema, but it’s a distinct condition requiring specific treatment approaches. Key treatments include conservative methods like manual lymphatic drainage, compression therapy, and carefully tailored exercise programs. In more advanced cases, liposuction and lymph-sparing procedures are recommended to remove the diseased fat cells and alleviate symptoms.
One of the most significant hurdles for patients with lipedema is getting insurance companies to cover the cost of surgeries. Many insurers classify lipedema surgery as cosmetic rather than medically necessary, leaving patients to bear the financial burden. However, with persistence, the right approach, and armed with evidence, it’s possible to secure coverage for these essential procedures.
Begin by thoroughly reviewing your insurance policy to understand what treatments and surgeries it covers. You will need to look at your insurance plan’s summary of plan benefits. You can obtain a copy of the plan summary through your insurance portal or your employer’s HR [ Human Resource ] representative. Look for exclusion for cosmetic surgeries as they often lump lipedema surgery in with cosmetic surgery. Look for any clauses related to chronic conditions, obesity-related treatments, and reconstructive surgeries. Also, look for exclusion for special services. Knowing the ins and outs of your policy will help you build a strong case for coverage.
If you have coverage, each insurance company has different medical necessity criteria that must be met for the company to even consider approving prior authorization. Often, these requirements include a certain BMI (or previous bariatric surgery with weight loss or medically supervised weight loss program) and trial of conservative measures, including the medial grade compression use, exercise, and manual lymph drainage. Some also include functional assessment of disability, intermittent pneumatic compression pumps, and secondary diagnosing physicians.
Getting a proper diagnosis is crucial. Several other diseases need to be excluded, including other lipomatosis [fat diseases such as Dercum’s and Madelung’s disease], lymphedema, and venous diseases such as pelvic venous compression. Several of the venous diseases that can look like lipedema should be excluded with a venous Doppler ultrasound and another test if indicated. Sometimes lipedema can coexist with obesity and/or lymphedema and/or venous disease. Each disease needs a different treatment. Failure to recognize the associated diseases can cause ineffective treatment and frustrated patients.
Consult with specialists, who are experienced and knowledgeable about lipedema. These professionals can provide detailed assessments, treatment plans, and supporting letters that emphasize the medical necessity of the surgery. Their expert opinions can be influential in convincing insurance companies of the need for coverage. Generally, these are vascular/venous and lymphatic specialists who focus on lipedema and lymphedema.
Detailed documentation of treatment is essential, including conservative treatments attempted, their outcomes, and the rationale for surgery. This plan should illustrate the comprehensive approach to managing your lipedema and why surgery is recommended.
Work with your healthcare provider to gather medical records, diagnostic tests, and letters of necessity. These documents clearly state that the surgery is essential for your health and not merely for cosmetic purposes.
If you are planning to use insurance, your surgeon should submit all of your documentation to your health insurance for “ prior authorization” ahead of your surgery.
If your initial claim is denied, don’t lose hope. Many patients succeed upon appeal. Carefully review the insurance company’s reason for denial and address these points in your appeal letter. Include additional documentation and expert opinions if necessary. Persistence is key, as several rounds of appeals may be required. Your surgeon can appeal the ruling.
You may consider using an additional resource such as an ERISA attorney, insurance advocate or a patient advocate. If you decide to use a patient advocate – be careful!
In the United States, there is an unregulated space where people describe themselves as patient advocates.
While some of these self-appointed patient advocates are helpful and ethical, other self-appointed advocates are duplicitous and attack patients and providers who do not recommend or refer for their costly services.
Reach Out For Help Today!
Securing insurance coverage for lipedema surgery is a challenging but not insurmountable task. It requires patience, thorough preparation, and a proactive approach. As we recognize World Lymphedema Day, let’s also acknowledge the importance of advocating for comprehensive care and support for those living with lipedema. By following the steps outlined above and leveraging available resources, you can increase your chances of getting insurance to cover your lipedema surgeries, paving the way for a healthier and more comfortable life.
Remember, your health is worth fighting for. With the right strategy, persistence, and support, you can navigate the complexities of insurance coverage for lipedema treatment and take a significant step toward managing your condition effectively.
In the ongoing battle against lipedema, a condition that affects millions of women worldwide, patients and specialists alike are in constant search for effective treatments. Lipedema, characterized by the abnormal accumulation of fat cells in the legs, arms, and other body parts, can lead to pain, swelling, and mobility issues. Dr. Wright, a leading lipedema surgeon based in St. Louis, is at the forefront of exploring innovative treatments to help those suffering from this challenging condition. One such promising treatment is Ozempic, a medication primarily known for its benefits in weight management. While not specifically studied for lipedema, emerging evidence and patient reports suggest it might relieve some individuals struggling with this condition.
Ozempic, a brand name for the drug semaglutide, is an injectable medication originally approved for the treatment of type 2 diabetes. It works by mimicking a hormone that regulates blood sugar, satiety, and the slowing down of gastric emptying. In recent years, its weight loss benefits have gained significant attention, leading to its use in managing obesity and related conditions.
Lipedema is a complex condition; effective management often requires a multifaceted approach. The condition is not just about excess fat but also inflammation and pain. Here’s where Ozempic steps into the picture. While primarily used for weight loss, Ozempic also has properties that reduce adipose inflammation. These two effects – weight management and the reduction of inflammation – are crucial in lipedema.
Many individuals with lipedema struggle with weight control despite maintaining a healthy lifestyle. The stubborn fat associated with lipedema does not respond well to conventional weight loss methods, including diet and exercise. Ozempic’s ability to aid in weight loss presents a glimmer of hope for those who have found little success with traditional methods. By reducing the volume of lipedema fat, Ozempic could alleviate some of the pressure and discomfort in the affected limbs.
Lipedema is not just a cosmetic issue; it’s a painful condition often accompanied by significant inflammation. This inflammation can exacerbate the pain and swelling associated with lipedema. Ozempic’s anti-inflammatory properties might help reduce this condition, relieving many sufferers.
Dr. Wright, a renowned lipedema surgeon in St. Louis, has observed the potential benefits of Ozempic in managing lipedema. According to Dr. Wright, while Ozempic has not been studied explicitly for lipedema, there are encouraging reports from patients who have experienced improvements in their symptoms. These improvements include weight reduction in lipedema areas, decreased inflammation, reduced pain, and better mobility.
Most of the prescriptions for Ozempic in lipedema come from primary care physicians, not directly from lipedema specialists. Patients have reported a decrease in the size of lipedema fat deposits and improvements in related habits such as smoking, drinking, and nail-biting. This suggests that Ozempic’s benefits extend beyond the direct treatment of lipedema, potentially improving overall health and well-being.
As with any medication, Ozempic comes with potential side effects. Some patients may experience nausea, muscle loss, constipation, and other discomforts. It’s crucial for individuals considering Ozempic for lipedema to consult with a healthcare provider, preferably one familiar with lipedema, to weigh the benefits against the possible risks. Dr. Wright emphasizes the importance of a tailored approach, taking into account each patient’s specific circumstances and health profile.
The exploration of Ozempic as a treatment for lipedema is still in its early stages. More research and clinical studies are needed to understand its efficacy and safety fully. However, the anecdotal evidence and preliminary observations by specialists like Dr. Wright offer a hopeful outlook for many who have struggled to find relief from lipedema’s debilitating effects.
Dr. Wright advocates for a comprehensive approach to managing lipedema, incorporating lifestyle modifications, specialized treatments, and, when appropriate, medications like Ozempic. The goal is to address the physical symptoms of lipedema and the psychological and emotional challenges that often accompany the condition.
For women suffering from lipedema, the journey to finding effective treatment can be long and fraught with frustration. The potential of Ozempic to aid in weight management and reduce inflammation presents a promising avenue for research and treatment. Dr. Wright, a leading figure in St. Louis lipedema treatment, continues to monitor and evaluate the benefits of Ozempic and other emerging treatments for lipedema. While Ozempic may not be a cure-all, it could be a valuable component of a comprehensive treatment plan for some individuals with lipedema. As with any medical treatment, it’s essential to consult with a healthcare provider to determine the best course of action for your specific needs.
In the quest to improve the quality of life for those with lipedema, Ozempic represents a potential tool in the arsenal against this challenging condition. With ongoing research and patient feedback, we hope treatments like Ozempic will bring us one step closer to effective management and relief for those affected by lipedema.
Lipedema is a chronic condition predominantly affecting women, characterized by abnormal fat accumulation in the legs and arms. It can be a confusing and often misdiagnosed condition, leading many to feel lost in their search for information and support. However, the internet has become a haven for resources, offering extensive information and a sense of community for those affected by lipedema. This blog will explore the wealth of resources available to women with lipedema, including the website lipedema.net, Dr. Wright’s YouTube channel, Facebook group, Instagram, and Pinterest pages, each offering unique insights and support for this condition.
Lipedema.net is an excellent starting point for anyone seeking comprehensive information about lipedema. This website is an extensive resource, providing detailed insights into the nature of the disease, symptoms, diagnosis, and treatment options. It offers:
For those who prefer video content, Dr. Wright’s YouTube channel, Lipedema Info, is a treasure trove of information. The channel features:
The Lipedema Group – Lipedema.net on Facebook is a vibrant community where members can find support and share experiences. This group offers:
Dr. Wright’s Instagram page, @lipedemasurgicalsolutions, is a visually engaging platform providing insights into the treatment and management of lipedema. Here, you can find:
Lastly, Dr. Wright’s Pinterest page, Laser Lipo Vein, is an excellent resource for educational material and inspiration. This platform offers:
Living with lipedema can be challenging, but with the right resources and support, managing the condition becomes significantly easier. From comprehensive information hubs like lipedema.net to engaging social media platforms like YouTube and Instagram, numerous avenues exist to explore for education, support, and community. Dr. Wright’s dedication to providing a wealth of resources across these platforms highlights the growing awareness and support for those battling lipedema. By leveraging these resources, women with lipedema can empower themselves with knowledge, find comfort in shared experiences, and remain updated on the latest in lipedema care and research.
Remember, while online resources are invaluable, they should complement, not replace, professional medical advice. Always consult with healthcare professionals for personalized medical guidance and treatment plans.
If you or someone you know is dealing with lipedema, we encourage you to explore these resources. Visit lipedema.net, subscribe to Dr. Wright’s YouTube channel, join the Facebook group, follow the Instagram page, and check out the Pinterest boards. Each platform offers unique perspectives and support, providing a comprehensive toolkit to understand and manage lipedema effectively. Join this growing community today and take a step forward in your journey toward wellness and empowerment.
Lipedema is a chronic and progressive disease that primarily affects women. It is often misdiagnosed as obesity or primary lymphedema, leading to a lack of understanding and appropriate treatment options. Lipedema’s physical and psychological consequences significantly impact the quality of life of those who suffer from it. This comprehensive guide will delve into women’s experiences with lipedema, highlighting their challenges and the importance of providing adequate care and support.
Lipedema is characterized by the abnormal deposition of subcutaneous adipose tissue, primarily in the lower body parts, such as the buttocks and legs. This adipose disease is of unknown etiology and tends to manifest during or after puberty, although it can also occur in connection with pregnancy or menopause. The accumulation of fat and fibrous tissue leads to bilateral swelling and enlargement, causing discomfort, bruising, severe pain, and limited mobility. Unfortunately, the progression of lipedema varies greatly, making it challenging to predict and control.
Conservative therapy, which focuses on patient education, weight control, manual lymphatic drainage therapy, and compression therapy, is commonly used to manage lipedema. Surgical interventions, such as liposuction, may be necessary in some cases. However, there are no easy solutions for treating lipedema, and further research is needed to develop more effective interventions.
Living with lipedema has a profound effect on the quality of life of women. The physical symptoms, including pain, fatigue, and limited mobility, significantly hinder their daily activities and overall well-being. Women with lipedema often describe their bodies as burdensome, feeling controlled and hindered by the swelling and pain they experience. The constant pain and discomfort can lead to exhaustion and a sense of helplessness.
Furthermore, the psychological impact of lipedema should not be overlooked. Women with lipedema often face fat-shaming and negative judgments from others, which affects their self-esteem and body image. They may feel unattractive and struggle with intimacy and sexual activity. The changes in their bodies, such as the appearance of loose and bumpy skin, pose additional challenges regarding hygiene and self-care. The lack of understanding and support from healthcare professionals further exacerbates their emotional distress.
Women with lipedema frequently seek medical help to address the changes in their bodies and the increasing pain they experience. However, obtaining an accurate diagnosis can be a lengthy and frustrating process. Many women have encountered healthcare professionals who lack knowledge about lipedema, leading to misdiagnosis or dismissive attitudes. Instead of receiving appropriate care, they are often advised to engage in weight loss exercises or visit physiotherapists and dietitians without addressing the underlying lipedema.
Women with lipedema often take matters into their own hands, researching and gathering information to understand their condition better. Some find the diagnosis themselves and present it to their doctors, only to face skepticism and hurtful comments. The lack of awareness and understanding among healthcare professionals contributes to feelings of isolation and a lack of support for women with lipedema.
Receiving a diagnosis of lipedema should be a turning point towards appropriate care and treatment. However, many women find themselves at a dead end. Despite having a confirmed diagnosis, they struggle to access the care they need. The limited knowledge about lipedema among healthcare professionals hinders the development of effective treatment strategies. Women with lipedema often have to fight for liposuction surgery, which can be crucial in managing the disease. They may also seek treatment abroad, incurring additional financial burdens.
The lack of guidance and support in medical decision-making further compounds the challenges faced by women with lipedema. They often feel alone, left to navigate their treatment options without sufficient professional advice. Some women have found supportive doctors who listen to their concerns and collaborate with them to develop appropriate treatment plans. However, these rare instances highlight the urgent need for increased awareness and knowledge among healthcare professionals.
Pain and fatigue are two significant symptoms that women with lipedema experience daily. The pain associated with lipedema is often described as aching, heavy, and unpredictable. It can worsen with movement and become stabbing in nature. Women with lipedema express feelings of exhaustion and describe the constant pain as debilitating. The invisible nature of their symptoms makes it challenging for others to understand and empathize with their experiences.
Fatigue, another common symptom of lipedema, further adds to the physical and emotional burden. Women with lipedema describe feeling constantly tired, which affects their ability to engage in daily activities. The lack of understanding and validation of their pain and fatigue by others, including healthcare professionals, leads to feelings of neglect and frustration.
Encounters with healthcare professionals play a crucial role in the lives of women with lipedema. Unfortunately, many women feel that their experiences are not taken seriously, resulting in a lack of dignity and respect. Healthcare professionals’ skepticism and dismissive attitudes toward their pain and symptoms contribute to feelings of violation and humiliation. Women with lipedema emphasize the need for healthcare professionals to listen, understand, and acknowledge their experiences.
Creating a supportive healthcare environment requires healthcare professionals to educate themselves about lipedema and its impact on patients’ lives. By validating women’s experiences and providing appropriate care, healthcare professionals can alleviate the emotional distress associated with lipedema. Collaborative decision-making and the involvement of specialists can also contribute to better treatment outcomes and improved quality of life.
Living with lipedema often leads to negative body image and decreased self-esteem. Women with lipedema may feel unattractive and struggle with self-acceptance. The changes in their bodies, such as the irregular distribution of fat and the appearance of cellulite, contribute to dissatisfaction and insecurity. The societal pressure to conform to narrow beauty standards exacerbates these negative feelings.
However, some women find solace in supportive relationships, particularly with their partners. Feeling desired and loved by their partners is essential for their overall well-being. The challenges of intimacy and sexual activity due to lipedema can strain relationships, but open communication and understanding can help foster intimacy and emotional connection.
Education and support play a vital role in empowering women with lipedema. Access to accurate information about the condition, treatment options, and self-care strategies can help women make informed decisions about their health. Support networks, both online and offline, provide a sense of community and understanding. Connecting with other women with similar experiences can offer emotional support and practical advice.
Additionally, psychological support is crucial for women with lipedema. Counseling or therapy can help address body image concerns, manage emotional distress, and enhance overall well-being. By addressing lipedema’s physical and emotional aspects, women can regain control over their lives and improve their quality of life.
The experiences of women with lipedema highlight the urgent need for change in healthcare systems and increased research on the condition. Healthcare professionals must be educated about lipedema to provide appropriate care and support. Developing evidence-based treatment guidelines and exploring novel interventions are essential to improve outcomes for women with lipedema.
In conclusion, lipedema has a significant impact on the quality of life of women who live with this chronic and progressive disease. Their physical and psychological burdens require healthcare professionals to approach lipedema with empathy, understanding, and respect. By providing adequate care and support, we can empower women with lipedema to navigate their journey towards better health and well-being.
Dr. Wright presented at the first World Congress on Lipedema, held in October 2023 in Potsdam, Germany. The common goal of this gathering was to share knowledge, experiences, and ideas related to the understanding and treatment of Lipedema and to benefit from first-hand, high-class education, network, and learn from world-renowned experts about the latest science and best practices in the management of lipedema.
The Lipedema World Congress is designed to bring together a broad spectrum of healthcare professionals, including lymphologists, plastic surgeons, angiologists, phlebologists, nutritionists, dermatologists, physical therapists, bariatric and Metabo specialists, and radiologists, as well as representatives of patient associates from around the world to share experiences and expertise on an international high-class level and to reflect on how to best incorporate these insights into education and clinical practice.
Dr. Wright gathered with peers from across the globe to learn the latest science and best practices in treating lipedema and shared his techniques and experiences treating patients. His presentation at the Lipedema World Congress was on how Lipedema Reduction Surgery Improves Mobility, Physical Function, and Multiple Measures of Quality of Life in Women with Lipedema.


World Congress on Lipedema, Potsdam, Germany, 4-7 October, 2023.
This is the first time Lipedema has had its own designated Congress, in which leading experts from over 35 countries gathered to discuss and learn about the disease. More than 500 participants testified that interest in the subject is constantly growing and is bringing important news to the international scientific community. The US-based Lipedema Foundation had a large presence at the Congress, bringing along their staff to share knowledge with the large group of attendees. The Lipedema Foundation alone funds around 10% of the research projects on the disease.
Many colleagues from overseas also participated with great interest, and numerous representatives of patient associations from various countries joined the professionals. Attendees heard from Sharie Fetzer and Kate Forster of Lipedema UK, Valeria Giordano and Marcella Oggiano of LIO Lipedema Italia, representatives from American Fat Disorders, and leading experts representing Danish, Australian, Dutch, Swedish, Finnish, and Canadian foundations and practices.


World Congress on Lipedema, Potsdam, Germany, 4-7 October, 2023.
Sessions began with live commentaries of surgical procedures on patients; those present could talk, discuss, and ask questions to the surgeons who illustrated their techniques. Dr. Fabio Kamamoto of Brazil began by illustrating the technique of laser ligation with simultaneous endovenous laser ablation (also referred to as EVLA). This was followed by Dr. Mojtaba Ghods and his Potsdam, Germany-based team demonstrating the Lymph-sparing Hybrid Technique: MicroAire PAL Large-Volume Liposuction and Manual Extraction in General Anaesthesia for Advanced Stages Lipedema.


Dr. Fabio Kamamoto illustrates the technique of Laser Liposuction with simultaneous endovenous laser ablation.
Dr. Ziah Taufig of Cologne, Germany, demonstrated the Human Med body-jet technique WAL Liposuction in General Anesthesia, followed by Dr. Barbara Herstant of Paris, France, who described with a video presentation the technique of VASER Liposuction + Renuvion J Plasma in General Anesthesia.


Dr. Ziah Taufig demonstrated the Human Med body-jet technique WAL Liposuction in General Anesthesia.
Finally, the first morning ended with a talk in the presence of our very own Dr. Thomas Wright, who illustrated his MicroAire PAL Liposuction in tumescent local anesthesia technique by video. The images alternating throughout the morning demonstrated how, with the application of effective techniques, the volumetric increase in the areas affected by Lipedema can be consistently reduced, with consequent benefits both functionally and on the symptoms related to the clinical picture.


Dr. Thomas Wright illustrated his MicroAire PAL Liposuction in tumescent local anesthesia technique at the World Lipedema Congress.
The afternoon session began with a presentation by Christine Moffat on the current state of care for patients with lipedema, which highlighted the serious deficiencies that exist in most public and private care systems worldwide. Several presentations on home self-management of the condition followed this. At the end of the first session, the co-chairs of the Congress reminded the audience that the disease was only a little over a year ago, finally recognized by the World Health Organization with its own code (EF.02.2) in the eleventh edition of the International Classification of Diseases, welcomed all those present to a packed and attentive hall.


Dr. M. Ghods Co-Chair


Dr. K. Herbst Co-Chair


Dr. S. Michelini Co-Chair
The second session on the conservative treatment of lipedema followed this. Several authors (Ure Christian, Michelini, Serena, and others) presented their experience, emphasizing the essential symptomatic aspect (although long-lasting and important in terms of symptom regression) of the treatments themselves.
In the third session, papers were presented on the status of genetic studies (still much to be investigated, even though the disease has clearly been revealed as hereditary), on biochemical studies, and on anatomical studies that are bringing us closer to a better understanding of the pathogenesis of the disease. Several authors took turns, including the Australian Rami Shayar and the Italian Saverio Cinti.
The fourth session, with presentations by José Luis Simarro, was devoted to the pathogenic hypotheses of the disease and, in particular, some of its symptomatological aspects, first and foremost, pain.


Dr. Simarro
The fifth and final session of the day was devoted to surgical treatment, particularly the various liposuction techniques, with the complementary aspects of using the various methods. Presentations were given by, among others, Thomas Wright and David Christel.
Dr. Wright
On 6 October, the day began with the General Assembly of the Lipedema World Alliance. The first of its kind, the LWA is a new and innovative association set up in 2022, made up of healthcare professionals, patient associations, and scientific societies. The Association is supported, in part, by ‘founding donors’, including Juzo Italia, Juzo International, LeSearch, Medi International, and Tactile Medical. The LWA’s president, Sandro Michelini, shared the motivations and steps that led to the creation of the association, emphasizing their mission, operating methods, and organizational charter. He also announced the start of registering regular members alongside their founding members. Potential members can review and submit their information to join the LWA here. During the assembly, several proposals were made, including that of organizing, if possible, a ‘dedicated’ international congress every two years in different locations.
The following session was devoted to the relationship between Lipedema and Obesity, which once again highlighted the fact that the association between the two pathologies is neither constant nor interdependent and that, in the case of obesity associated with Lipedema, bariatric surgery, which has a good effect on the classic sites of accumulation of adipose tissue, does not have such an effect in the anatomical sites affected by Lipedema itself.
The next session was followed by the presenter describing in more detail the aims of the Lipedema World Alliance. Johnatan Kartt described the activities of the Lipedema Foundation, which are mainly aimed at supporting scientific research. Dr. Karen Herbst and Dr. Gabriele Faerber then described the American and German Lipedema guidelines. Dr Faerber also compared the main consensus documents currently in place. During the lunch break, there was the opportunity to follow extra-congressional work with the description of other surgical experiences (WAL and other techniques) by several alternating specialists.
That afternoon, the resumption of proceedings was devoted to nutritional aspects; the presentations showed that the ketogenic diet (Giovanna Pitotti, Malgorzata Jeziorek, and other authors) and ‘low carb’ are the most effective dietary regimes in the disease. This was followed by the session on epidemiological and diagnostic aspects, with speakers touching on differential diagnosis aspects (Rachelle Crescenzi, Epameinondas Gousopoulos, and other speakers), including that between Lipedema, lipohypertrophy, and Secondary Lymphoedema. The last session highlighted the possible interactions between Lipedema and the lymphatic system. It featured other important and well-known speakers such as Stanley Rockson, Alberto Onorato, Jean-Paul Belgrado, and Hakan Brorson.


International experts possible interactions between Lipedema and the lymphatic system.
The evening ended with the Gala Dinner, during which the Lipedema Foundation honored Ghods for his scientific and care commitment. There were also some truly uplifting moments of fellowship and fun, during which it was possible to deepen mutual understanding between the various participants, as well as on some of the topics discussed after the presentations.


The Founder’s Dinner for the Founders of Lipedema World Alliance.
Saturday morning began with a plenary discussion on the results of the first two steps of the Delphi study, which was so well attended that it lasted for much of the coffee break time. The lively and substantive discussion led to the final draft [ of the contents of the paper that will be published in the coming weeks.
Dr. Kruppa prepared 100 statements about lipedema to review by the participants, and prior to the meeting, the statement had been modified and winnowed to 69 statements. The open session was chaired by Dr. Michelini, Dr. Kruppa, and Dr. Cresscenzi. During this time, Dr. Wright and nearly 100 experts worldwide discussed and debated the consensus statements.
The goal of this important project is to define what is agreed to be understood in the field of lipedema research and treatment. Also, to point out areas where more research and coordination are needed. The results of this work are hoped to produce a position paper focusing on lipedema coordinated by the Lipedema World Alliance. This document aims to comprehensively cover various aspects of lipedema, including its nature, epidemiology, pathophysiology, diagnosis, and treatment approaches. The intention is to create a resource that assists healthcare professionals, researchers, funders, and individuals impacted by lipedema in understanding the current opinions of experts and gaps in knowledge and management of the condition.


Left to Right: Dr. Crescenzi, Dr. Kruppa, and Dr. Michelini preside over the Delphi consensus discussions.
This position paper is the basis and starting point for further areas to be explored as they relate to lipedema. Given the evolving nature of lipedema research and the varying degrees of evidence available, reaching a unanimous consensus in certain areas might prove challenging. Acknowledging this, the project will employ a multi-step Delphi method to facilitate expert collaboration. This method will enable the group to iteratively evaluate and refine statements related to lipedema based on the current literature and collective expertise.
The last conference sessions followed this, the first of which was dedicated to basic science, histology, and molecular analysis. Among the various papers presented, the one by Cannataro, who, with the coordination of the writer, carried out on tissue samples selected and taken by the Plastic Surgeon Nicola Vaia in Rome, together with his wife Erika Cione (biochemist at the University of Cosenza), showed the data of a preliminary study that highlighted the presence of an ‘up-regulator’ micro-RNA as a possible ‘marker’ of the disease, arousing lively interest in those present (at the moment, the diagnosis of the disease is essentially clinical).


Dr. Cannataro explains data from a preliminary study that highlights the presence of an ‘up-regulator’ micro-RNA as a possible ‘marker’ of Lipedema.
The last session was again dedicated to various liposuction procedures. Various speakers took turns (including Agostino Bruno, Enriquez Burgos, Uwe Wollina, Corrado Cesare Campisi, Thomas Su, and others), highlighting some aspects relating to the effectiveness of the techniques and the sparing of other anatomical structures (first and foremost, the loco-regional lymphatic system).
As already mentioned, one of the novelties of the Congress was the role of the patients’ associations, which was much appreciated. This participation was precisely in the spirit advocated also by the WHO, of sharing the experiences of healthcare professionals with patients’ associations and, above all, finalizing the collaboration itself to the drafting of consensus documents useful in clinical practice and functional for recognition at the level of individual country governments.
The first World Congress on Lipedema upheld its promise to be an unparalleled gathering of experts and stakeholders in the field. Dr. Wright was honored to contribute his knowledge, learn from renowned experts, and collaborate with peers worldwide. Together, they’re paving the way for advancements in the understanding and management of lipedema.
Dr. Thomas Wright is a leading expert in venous and lymphatic medicine, with 15+ years of experience dedicated to advancing lipedema treatment. As the medical director of Laser, Lipo, and Vein Center, he’s among the first 200 US surgeons to attain diplomat status with the American Board of Venous and Lymphatic Medicine. He is a Fellow of the American Venous and Lymphatic Society. His research contributions include peer-reviewed papers on lipedema and co-authoring the US Lipedema Standard of Care Guidelines. Dr. Wright’s expertise covers lipedema reduction surgery, fat transfer, and minimally invasive skin tightening. Trained by Dr. Jeffrey Klein, he has performed thousands of tumescent liposuction procedures for cosmetic and lipedema patients, collaborating with institutions like Washington University and the University of Arizona to deepen our understanding of lipedema.
We are pleased to announce that Dr. Wright accepts patients for Lipedema Reduction Surgery in-network with United Healthcare. We are delighted that United Healthcare is working with us to provide the lipedema patient community with in-network lipedema treatment options. Please be aware that United Healthcare’s medical necessity criteria must be met to their satisfaction before approval. This includes six months of conservative therapy (diet, exercise, compression), photo documentation showing disproportionate tissue of the extremities, and documentation of functional impairment. We also highly recommend that patients document their personal journey to share with their provider and UHC to prove their need for further treatment.
We aim to help the lipedema community obtain affordable in-network treatment and care. We will continue to work with other payers to achieve fair compensation for the expertise and outstanding patient care and outcomes we provide to our patients.
Lipedema is a chronic condition affecting many women, causing disproportional fat distribution and significant physical discomfort. Fortunately, UnitedHealthcare (UHC) Insurance offers lipedema treatment insurance coverage, but it’s essential to understand their strict criteria and the steps required to get the coverage you need. We’re here to guide you through obtaining lipedema insurance coverage through UHC while shedding light on Dr. Wright’s success in securing coverage for his patients.


United Healthcare recognizes individuals’ challenges with lipedema and has developed a policy for treating this condition. However, it’s important to note that they have stringent criteria that must be met to qualify for lipedema covered by insurance. Below is the general outline of what criteria UHC is looking for. At the end of this article, we summarize the entire process that includes this criterion.
To be eligible for treatment for lipedema covered by insurance through UHC, you must meet the following criteria:
Diagnostic Criteria: You must meet all diagnostic criteria for lipedema. This includes having photographs showing disproportional fat distribution consistent with the diagnosis. Additionally, you must have documented evidence of the failure of disproportional fat to respond to medically supervised weight loss or bariatric surgery if your BMI is in class 2 or above (BMI +35).
Conservative Therapy: You should have completed medically supervised conservative therapy for lipedema for at least six months. This therapy includes compression garments, manual lymphatic drainage (MLD), and a low-carb diet. Documenting your efforts is crucial. You must document if symptoms persist despite diet adherence and compression use.
Medical Evaluation: In addition to diagnosing lipedema, you’ll need another diagnosis from your primary care physician (PCP) or a specialist who is not providing surgery for lipedema. This diagnosis should support the need for surgical intervention to treat lipedema.
Functional Impairment: To further substantiate your coverage case, you must provide documentation of functional impairment. This could include how lipedema affects mobility, physical activity, and daily life. Be sure to detail the limitations you experience due to lipedema, as this will strengthen your case.


One positive aspect to highlight is that Dr. Wright has had significant success in helping his patients secure lipedema insurance coverage treatment through United Healthcare. This speaks to the importance of having a knowledgeable and experienced medical professional on your side when navigating the insurance process. His patients have seen great success with lipedema surgeries and long-term quality-of-life changes. Below he and one of his patients were featured on FOX 2 St. Louis!
Now that you understand the criteria for UHC’s lipedema coverage policy, let’s outline the steps to help you secure the coverage you need:
United Healthcare does offer coverage for lipedema treatment, but they have strict criteria that must be met. By following the steps outlined in this article and enlisting the expertise of a knowledgeable specialist like Dr. Wright, you can increase your chances of obtaining the coverage you need to manage and treat your lipedema effectively. Remember that your health and well-being are worth the effort required to navigate the insurance process successfully.
Read more about the UHC Policy here.
We will make every effort to get patients approved for Lipedema Reduction Surgery; however, final approval for medical necessity and prior authorization is determined by United Healthcare and at the discretion of a Medical Director at United Healthcare. We cannot guarantee patients will be approved for surgical procedures.
The general rule of thumb for Lipedema Insurance Coverage claims reimbursements is that any given claim must be deemed “medically necessary”. Lymph Sparing Liposuction is nearly always considered a cosmetic surgical procedure in nature or experimental, meaning this is an elective procedure and not a medical necessity. Of course, as explained above, this is not the case for women with Lipedema, as lymph-sparing liposuction is the only treatment option for dealing with this disease that can reverse progression. However, the combination of the surgery being deemed cosmetic and election plus the general under-education and lack of awareness in the medical community has led to the battle patients and Lipedema surgeons are fighting. We must educate and advocate for these surgeries to be covered.
The liposuction CPT codes 15877-79 are cosmetic codes that were never intended to be used by commercial insurers to cover reconstructive or medically necessary procedures to improve function and technically should not be used for reconstructive treatment. Because they are cosmetic codes and are not covered by Medicare, they have never had a value or RVU (Relative Value Units) assigned to them. Some medical insurers like Blue Cross Blue Shield exploit the lack of an assigned value for the codes they insist on using. If an insurance company assigns little or no value to the surgery, even when it is a covered benefit, they can pay less for the 5-hour surgery than for a 15-minute follow-up office visit. This means that because they use cosmetic codes 15877-79, which can have little or no value assigned by commercial payers like Blue Cross Blue Shield, they can pay so little that they are, for practical purposes, technically “covering” treatment. But in practice, they’re not covering liposuction to treat lipedema. The good news, at least for now, is that UHC is covering Lipedema Surgery with a reasonable assigned value.
Despite the challenges and lack of coverage, some physicians, like Dr. Wright in St. Louis, do everything they can to work with patients to get insurance coverage. They are familiar with the ins and outs of different insurance providers, and their teams work extremely hard to get patient coverage. ERISA experts and attorneys can help you work on lipedema treatment coverage, and physicians can help you connect with them if you aren’t sure where to start.
You might also come across individuals who are self-described as “patient advocates”. These individuals will present themselves as experts in getting coverage for you. Still, they’re not licensed individuals and are unlikely to be bound by patient privacy laws that you’ll get with physicians and attorneys. We are aware of players in this field who are bad actors and ultimately hurt the cases of patient coverage. Be sure to check the BBB listings, names, and addresses of anyone wanting to work with you, along with Google Reviews and website listings.
Please reach out to our office, and Dr. Wright’s team would be happy to refer you to experts depending on where you are in your Lipedema diagnosis and treatment journey. We’re here to help, and happy to get you started!
Dr. Wright’s innovative lipedema surgery techniques are transforming lives by improving mobility and enhancing the quality of life for patients. He will be conducting a video demonstration of his surgical techniques in a Master Class for Lipedema treatment at this year’s 1st Annual Lipedema World Congress. 

As a founding member of Lipedema World Alliance (LWA) and with expertise in this procedure, Dr. Wright will present the Tumescent Local Anesthesia (TLA) approach using power-assisted liposuction. In this course, he will describe his approach and techniques to give the best surgical outcomes and the greatest impact on mobility and quality of life long-term. His video demonstration and Master Class will be conducted on October 4, 2023, in Potsdam, Germany, with international participants from Spain, Italy, Austria, Germany, Norway, Lithuania, Sweden, Australia, India, Argentina, Brazil, USA, Iceland, Denmark, and Turkey. Below, we outline the topics and steps Dr. Wright will discuss.
Patients must first implement an anti-inflammatory diet and compression therapy. Their diets should emphasize low-refined carbs and avoiding processed foods, and medical-grade compression optimizes lymphatic function and tissue inflammation. These combined measures can decrease limb size, decrease pain, and lead to softening of the lipedema tissue ahead of surgery.
Before lipedema surgery, using high-frequency Ultrasound, the greater and smaller saphenous veins are mapped, and adjacent principal lymphatic collecting ducts are located. The watershed area around the principal superficial lymphatics in the legs is approached with extra care during surgery.
Tumescent fluid helps protect vascular and lymph vessels from injury, so the surgical area must be completely tumescent. Dr. Wright was trained in the Tumescent Technique by its inventor, Dr. Jeffery Klien. He follows The Klein Method and Dosing. General anesthesia adds the risk of general anesthetic medication. It can also lead to areas of inadequate tumescence because the general anesthesia blocks the ability to find areas that were incompletely tumescent.
Dr. Wright uses small (3mm) blunt cannulas to remove as much lipedema-affected adipose tissue as possible. This process works to debulk the area using longitudinal techniques.
The cannula is directed in longitudinal strokes, especially in the areas marked with lymphatic collectors, so it allows transecting of the lymphatic vessels. This requires frequent position changes, sometimes 8-12 different patient re-positions, to ensure he can remove the tissue using longitudinal cannula strokes.
After as much lipedema-affected tissue as possible has been removed with the suction cannula, he feels and massages the affected areas to check for any remaining fibrous lipedema nodules. If lipedema nodules are still present, then we manually loosen the nodules. If necessary, we manually extract them with an additional puncture of incision.
The patient is then placed in medical-grade compression to be worn for 24 hours a day for the first month.
Early-stage Lipedema (Stage 1) has small nodules the size of small seeds or peas, which often appear pearl-size. Middle-stage Lipedema (Stage 2) has larger nodules that feel the size of walnuts or gumballs. The presence of lobules characterizes the later stage, Lipedema (Stage 3). The nodules in Stage may be the same size as those in Stage 2, or they may be larger up to the size of a plum.
In the earlier stages of Lipedema (Stage 1 and most patients in Stage 2), the subcutaneous nodules are removed with lipedema reduction surgery, which involves modification of cosmetic liposuction using tools and techniques that minimize harm to the lymphatics. In lipedema patients with larger or more adherent nodules, the nodules have to be manually extracted.
In these cases, a small incision is made over the nodules that resist removal with a suction cannula and are gently milked out of the skin. Surgeons don’t want to cause any more trauma than is absolutely necessary. However, there are instances where this method is the only way to get larger, more adherent nodules removed. Dr. Wright has several videos of the extraction process you can view here.
The procedure typically takes several hours to complete, depending on the extent of the lipedema.
Patients may experience some discomfort and swelling in the days following the procedure, but this can be managed with pain medication and other treatments.
Most patients can return to work and other activities within a week or two, although this may vary depending on the extent of the liposuction and individual healing rates.
By reducing the amount of subcutaneous fat tissue, you can reduce any pain associated with lipedema. Lipedema reduction surgery, sometimes called Lymph sparing liposuction, will help you increase mobility without having the pain you have been feeling with lipedema since it started. This is huge for women with lipedema, especially because the pain and bruising is the leading symptom of seeking treatment. Women report a significant improvement in their ability to move around more freely, exercise more regularly, and enjoy day-to-day activities that were previously off-limits. Bumping into a chair or a corner no longer causes large bruises, playing with the family dog doesn’t cause pain when they jump, and everyday activities are no longer considered out of reach.
Lipedema, also known as lipoedema, is a chronic condition that affects many women worldwide. It is characterized by an abnormal accumulation of painful adipose tissue, primarily in the legs. Unfortunately, lipedema is often misdiagnosed as simple obesity, leading to misunderstandings and challenges for women seeking proper healthcare. In this comprehensive guide, we will explore the causes, symptoms, and management of lipedema. We will also delve into St. Louis lipedema treatment options, highlighting the importance of early diagnosis and a multidisciplinary approach to care.
Lipedema is a complex condition with various factors contributing to its development. While the exact cause is unknown, there is a strong hereditary component, suggesting a genetic predisposition to the disorder. Hormonal imbalances and significant life events, such as puberty, pregnancy, or menopause, can trigger the onset of lipedema symptoms.
The classic presentation of lipedema is characterized by a disproportionate accumulation of fat in the lower body, while the upper body remains relatively unaffected. The legs may appear columnar or lumpy, with fat deposits often extending from the hips to the ankles. Importantly, the feet and ankles are not typically affected, distinguishing lipedema from regular weight gain.
In addition to the visible fat accumulation, individuals with lipedema experience pain and tenderness in the affected areas. The fat deposits can be sensitive to pressure and may bruise easily. Furthermore, the skin overlying the fat may feel different from other areas of the body, exhibiting reduced elasticity.
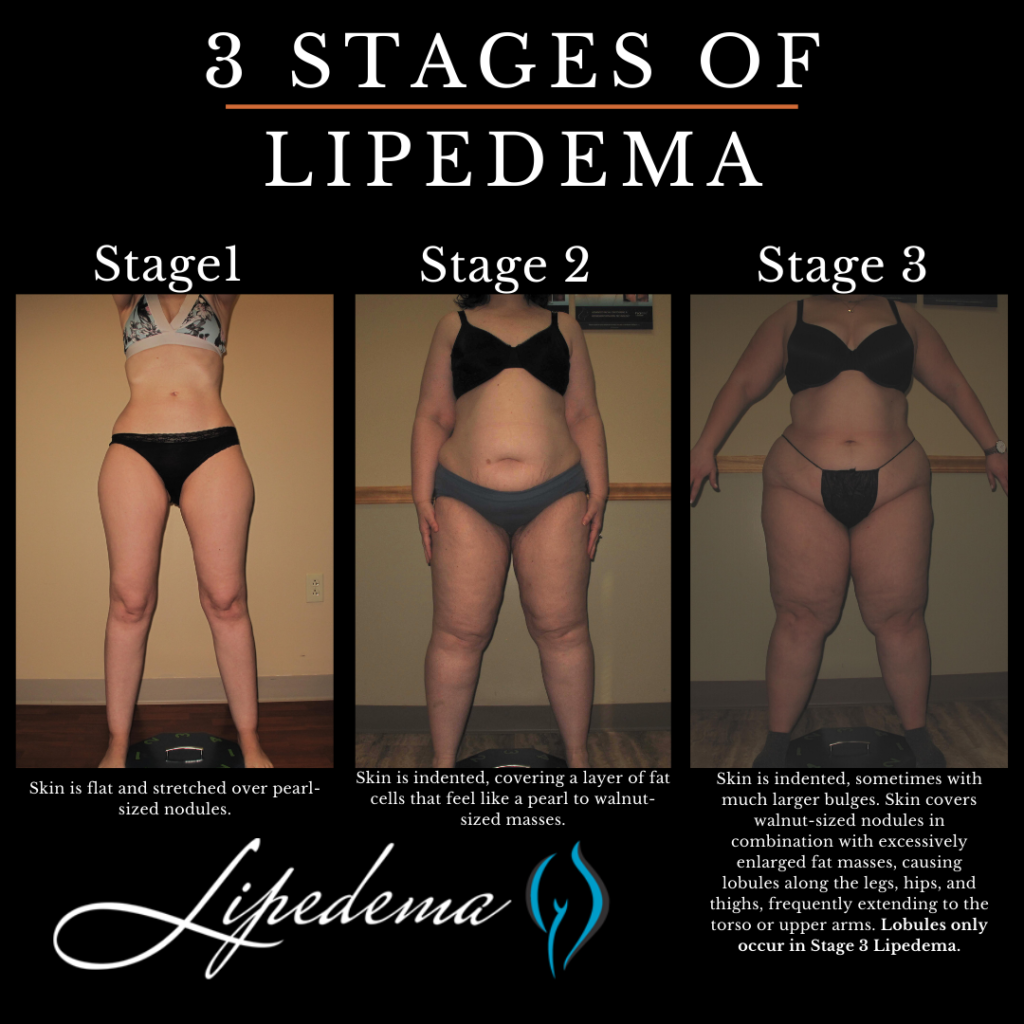
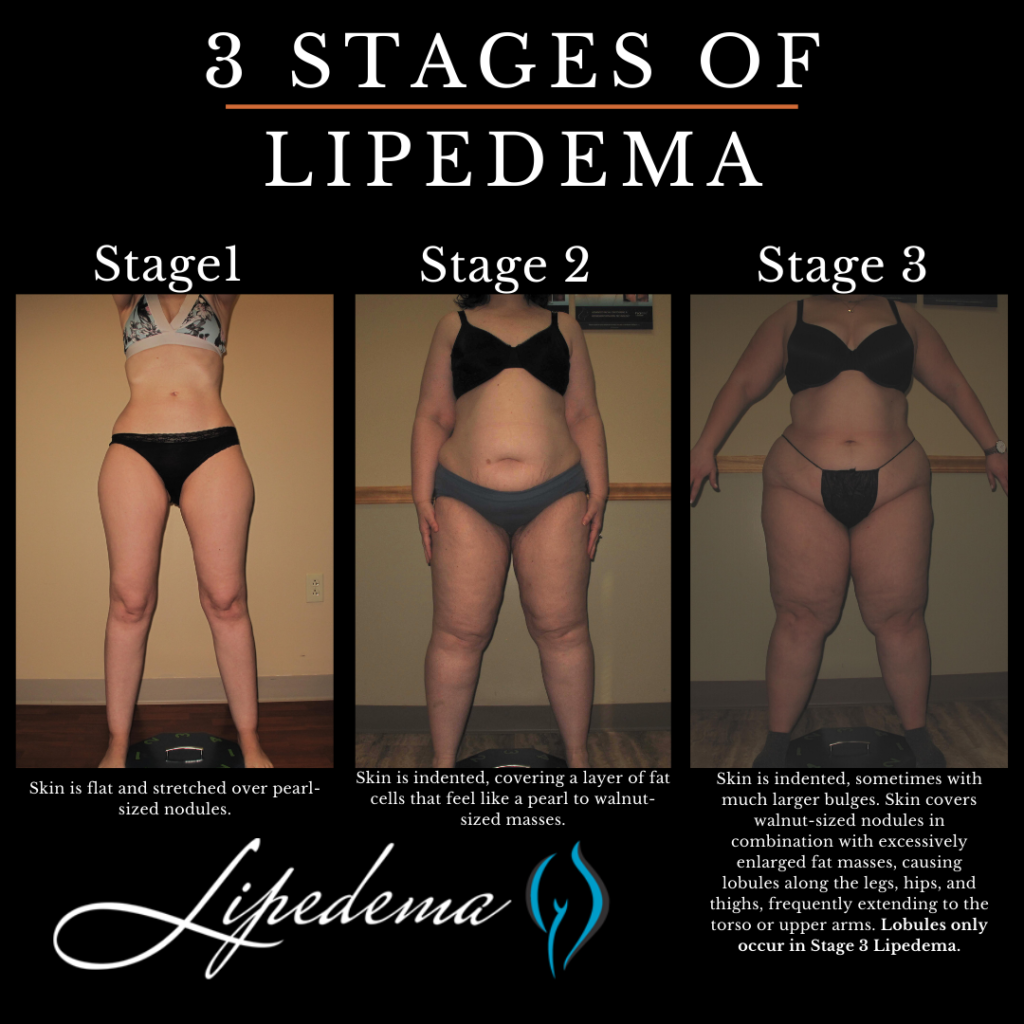
Lipedema is commonly described in three stages, although it is important to note that these stages of lipedema are not necessarily progressive. The stages reflect the severity of the condition and the presence of additional factors such as obesity and lymphedema.
At this stage, individuals primarily experience lipedema without significant obesity or lymphedema. The legs exhibit excess fat accumulation, and pressure on the fat deposits may cause pain. The skin remains healthy, and there is no visible swelling in the ankles or feet. While the symptoms may be bothersome, with proper management, Stage 1 lipedema can be effectively controlled.
In Stage 2 lipedema, the fat accumulation becomes more pronounced, and the pain and discomfort intensify. The affected areas may exhibit increased sensitivity, making daily activities challenging. At this stage, individuals may also begin to notice swelling in the ankles and feet, indicating the potential onset of lymphedema. It is crucial to seek appropriate treatment and lifestyle management strategies to prevent further progression.
Stage 3 lipedema represents the most severe form of the condition, often accompanied by significant obesity and lymphedema. The excess fat deposits are more extensive, causing considerable pain and impairing mobility. Swelling in the lower extremities becomes more apparent, requiring specialized treatment approaches to manage the combined effects of lipedema, obesity, and lymphedema.
In St. Louis, there are various treatment options available for individuals living with lipedema. It is essential to consult with a healthcare professional experienced in managing this condition to develop a personalized treatment plan. A multidisciplinary approach is typically recommended, combining medical interventions, lifestyle modifications, and emotional support.
Medical interventions for lipedema focus on symptom management and improving overall well-being. The following treatments may be considered:
In addition to medical interventions, lifestyle modifications can greatly impact the management of lipedema. The following strategies may be beneficial:
Living with lipedema can be emotionally challenging, as individuals may face stigma, body image concerns, and difficulties in finding appropriate healthcare providers. Seeking emotional support and education can significantly improve coping mechanisms and overall mental health. Connecting with support groups, patient communities, and organizations dedicated to lipedema can provide valuable resources and a sense of belonging.
Lipedema is a chronic condition that requires a comprehensive approach to management. Understanding the causes, symptoms, and available treatment options is essential for individuals living with lipedema. In St. Louis, there are dedicated healthcare professionals experienced in diagnosing and treating lipedema. By implementing a combination of medical interventions, lifestyle modifications, and emotional support, individuals with lipedema can effectively manage their symptoms and improve their quality of life. Remember, early diagnosis and treatment are key to preventing further progression and maintaining optimal health. If you suspect you may have lipedema, consult with a healthcare professional experienced in managing this condition to develop a personalized treatment plan tailored to your specific needs.


In today’s society, body image and weight management are often hot topics of discussion. Many individuals strive to achieve their desired physique through diet and exercise. However, for some, the struggle to lose weight in certain areas, particularly the legs, can be frustrating and confusing. This leads us to a common question: Is it lipedema or obesity? In this comprehensive guide, we will explore the key differences between lipedema and weight gain, helping you understand your body better and make informed decisions about your health and well-being.
Lipedema is a chronic and progressive medical condition characterized by the abnormal accumulation of fat cells, primarily in the lower body. It predominantly affects women, with an estimated prevalence of 7-11% in Western countries. Lipedema causes a disproportionate increase in fat deposits in the legs, hips, and buttocks while sparing the hands and feet. Individuals with lipedema often have a smaller waist and upper body, creating a distinct pear-shaped appearance.
One of the primary distinctions between lipedema and weight gain is that lipedema fat is resistant to traditional weight loss methods such as diet and exercise. Despite leading a healthy lifestyle, individuals with lipedema find it challenging to reduce fat in the affected areas. Lipedema fat can also exhibit unique characteristics, such as a gelatinous texture and the presence of small nodules beneath the skin.
Lipedema is thought to have a genetic component, with hormonal changes during puberty, pregnancy, and menopause potentially triggering its onset or exacerbation. It is crucial to understand that lipedema is not caused by obesity. While many individuals with lipedema may also be overweight or obese, the condition itself is independent of weight status.


It is important to distinguish between lipedema and weight gain to ensure accurate diagnosis and appropriate treatment. While both conditions involve the accumulation of excess fat, they have distinct characteristics and underlying causes.
Lipedema presents with specific symptoms that differentiate it from general weight gain. Individuals with lipedema often experience:
In contrast, weight gain typically occurs more evenly throughout the body and is not associated with pain or other physical symptoms commonly seen in lipedema.
One of the key distinctions between lipedema and weight gain is the response to lifestyle changes. Individuals with lipedema often find that diet and exercise alone do not significantly impact the fat accumulation in the affected areas. Despite their best efforts, weight loss may be minimal or not occur at all in these specific regions. On the other hand, individuals experiencing general weight gain will typically see changes in their body composition through proper nutrition and physical activity.
Lipedema fat distribution differs from general weight gain. Lipedema fat primarily affects the lower body, including the legs, hips, and buttocks, while sparing the hands and feet. This leads to a distinct shape and disproportion between the upper and lower body. In contrast, weight gain is typically more evenly distributed throughout the body, without the characteristic pear-shaped appearance.
Lipedema not only affects physical health but can also have a significant psychological and emotional impact. Many individuals with lipedema experience depression, low self-esteem, and social isolation due to the perceived body image differences and the challenges associated with finding appropriately fitting clothing. Weight gain, on the other hand, may have similar psychological effects but is not specifically linked to the unique challenges faced by individuals with lipedema.


Accurate diagnosis is essential to establish appropriate treatment strategies for individuals with lipedema. If you suspect that you may have lipedema, it is crucial to consult with a healthcare professional experienced in the diagnosis and management of this condition. They will evaluate your symptoms, medical history, and perform a physical examination to assess fat distribution and other associated features.
Currently, there is no cure for lipedema, but various treatment options can help manage symptoms and improve quality of life. Treatment for lipedema may include:
It is important to note that liposuction is not a cure for lipedema but can offer significant improvements in symptoms and overall quality of life for select patients.


Understanding the difference between lipedema and weight gain is crucial for accurate diagnosis and appropriate treatment. Lipedema is a chronic condition characterized by the abnormal accumulation of fat in the lower body, while weight gain is a general increase in body weight. Lipedema fat is resistant to traditional weight loss methods, and individuals with lipedema often experience specific symptoms, such as pain, tenderness, and easy bruising.
If you suspect you may have lipedema, consulting with a healthcare professional or an experienced lipedema specialist is essential to develop an individualized treatment plan that addresses specific needs and goals. Dr. Wright and his team of experts are here for you whenever you’re ready to start your treatment journey!
Remember, your health and well-being are important, regardless of your body shape or size. By seeking appropriate care and support, you can live a fulfilling life and embrace your unique beauty.