It’s not uncommon for women with Lipedema to either be misdiagnosed with severe obesity, or diagnosed with both Lipedema and obesity. In either scenario, it can be difficult to know what the next step should be. And if your doctor is recommending a serious surgery, such as bariatric surgery, to address obesity, it can be even more difficult to understand the relationship that has with lipedema, and how treatments should work so that both issues are addressed.
My Doctor Says Lipedema Isn’t Real – What Do I Do?
To make it more confusing for women with lipedema, there are contrasting opinions about the disease itself, as well as how to properly treat it. While some researchers assert that there is no edema (swelling) in lipedema and women reporting symptoms of this disease are imagining the pain and irreversible weight gain, this is not the case. Over and over, lipedema experts have found these assertions are based only on opinion and have no medical accuracy.
Studies not only found biomarkers leading back to this disease, but they’ve also determined that diet and weight loss do not affect lipedema tissue and that the only long-term solution is to extract these nodules via liposuction surgery. In a powerful study by Joanna Dudek et al, the research found that pain and the increase of this lipedema tissue is the precursor to mental health issues such as depression, rather than the other way around. Research continues to be done and the field of study is rapidly expanding as awareness grows. Insurance providers are beginning to recognize and cover liposuction as a form of treatment through the new Standard of Care guidelines, and more women than ever are beginning the treatment process that they desperately need.
How Do I Start The Treatment Process for Lipedema?
Typically, BMI plays a large role in the starting point for obesity diagnosis, even if patients are certain they have lipedema. But what many don’t realize is that both can be true! The longer your lipedema goes untreated, the more it progresses. And the more lipedema progresses, the more likely it is that you develop obesity as a side effect.
- Lipedema fat accumulation can contribute and lead to a Body Mass Index (BMI) of up to 35.
- Obesity in addition to lipedema can lead to higher BMIs, ranging from 45 to 50+.
- In these cases, it’s imperative to first address and treat obesity prior to putting together a treatment option for lipedema.
- The most successful obesity treatment is Bariatric surgery.
At a glance: Bariatric Surgery + Lipedema Treatment
Step 1: Speak with a Lipedema specialist before committing to Bariatric Surgery.
Step 2: Assuming your lipedema medical provider agrees, undergo this procedure.
Step 3: Give yourself time to heal, adopt an active lifestyle, healthy eating habits.
Step 4: Get an official Lipedema diagnosis, if not obtained in Step 1. Adopt non-surgical lipedema treatments at home.
Step 5: Follow your lipedema provider’s plan for working with insurance and schedule the appropriate surgeries!
What Does BMI have to do with Lipedema?
Body Mass Index (BMI) = weight in pounds (or kilograms) divided by height in feet squared (or meters squared).
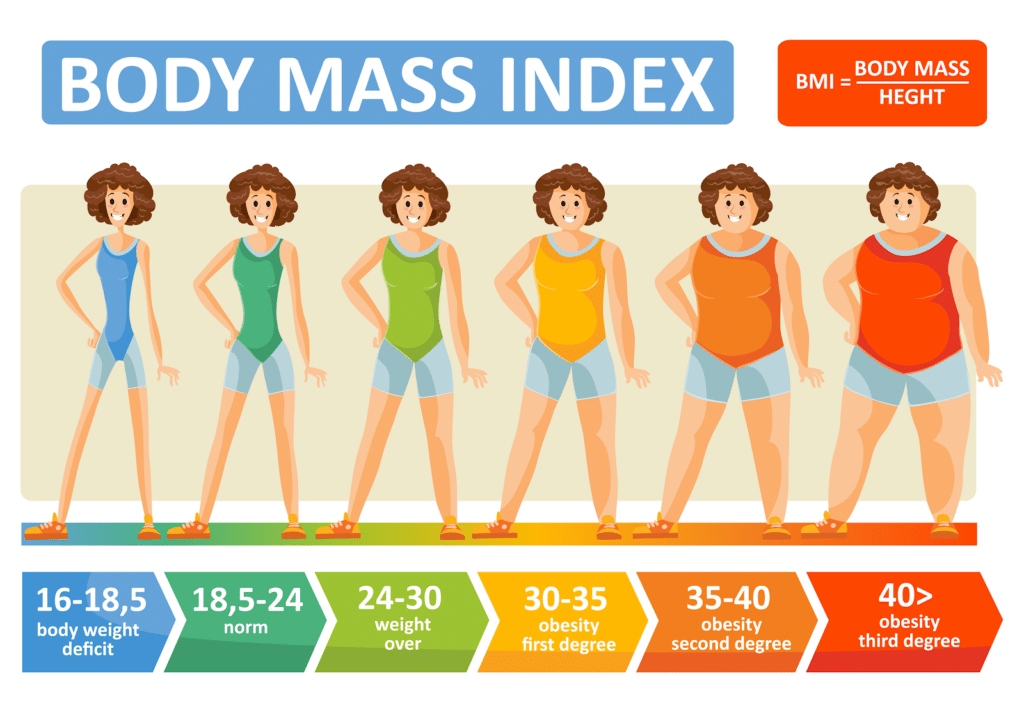
Body Mass Index (BMI) is simply an overall numerical score (like height and weight) which is not a biological representation of a person’s overall health. While the World Health Organization (WHO) defines a BMI over 25 as overweight and over 30 as obese, this is actually an inaccurate and incomplete assessment. Overall, obesity is a condition where fat mass affects patients metabolically, chemically, and mechanically (for example, in your joints).
In many cases, BMI is actually a very flawed number that leads doctors to misdiagnose women with Lipedema with obesity instead. The Body Mass Index (BMI) calculation is an unfortunate oversimplification of a person’s health and ignores extremely important factors that are imperative for accurate diagnosis and treatment plans. Family history and genetics, general lifestyle and activity levels, age, gender, and body composition (muscle mass, water content, bone mass) are all essential parts of our health profile, all of which are ignored by the BMI calculation. Despite all of this, it continues to be used worldwide to aid in diagnosing (or misdiagnosing and oversimplifying) patient health profiles.
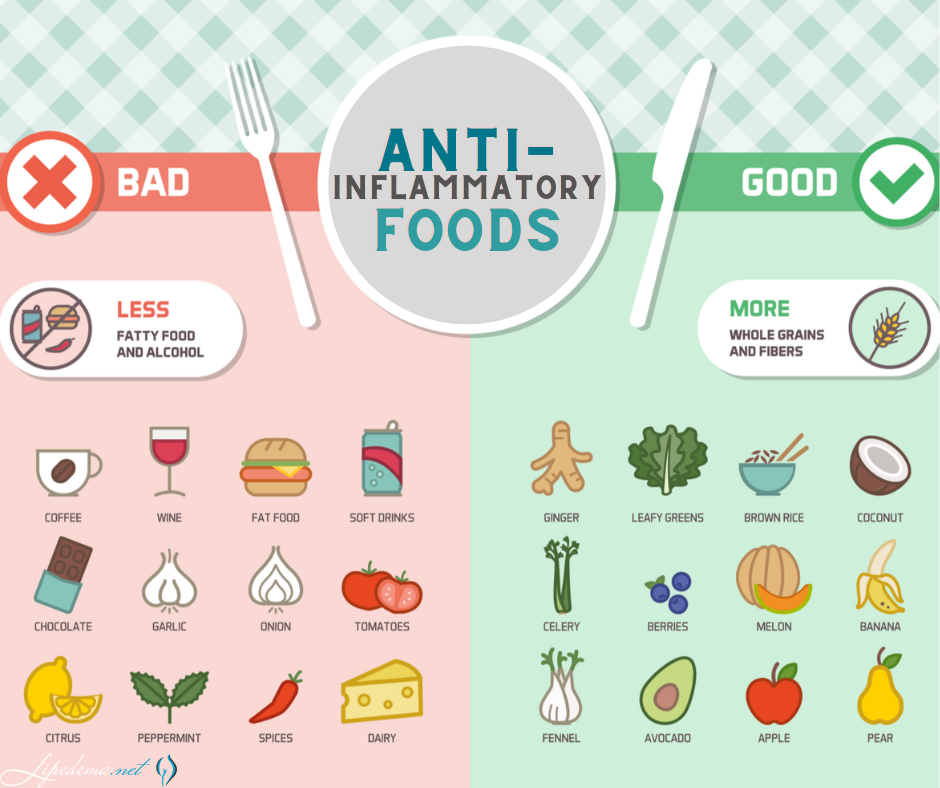
As mentioned above, lipedema can lead to a BMI of 35 simply due to the disproportionate fat it creates. At this point, it’s unlikely that patients have metabolic fat accumulations because lipedema fat is somewhat cardiac protective. At this point, patients can likely manage it well enough with an anti-inflammatory diet and regular exercise.
This helps treat lipedema and is associated with weight loss because low inflammation means patients also have low insulin excretion, which, in itself, helps patients feel better, improve health, and manage their lipedema.
However, once a BMI over 35 is reached, patients are considered to have both lipedema and obesity. At this point, weight loss is CRITICAL. You must address that first, because the increased weight puts additional pressure on your lymphatics, further aggravates the existing lipedema, and continues to negatively affect the venous return. All of this leads to more serious medical issues.
The metabolic issues that develop from obesity are extremely serious, especially high blood sugar and increased levels of triglycerides which can aggravate and increase BMI even more. Ultimately, patients find themselves in a disastrous cycle, starting with increased BMI and fat accumulation, leading to metabolic issues, and then to further increases in obesity and lipedema.
The best part about addressing obesity with Bariatric Surgery? It increases the odds of significant and long-term weight loss.
One study showed that 95% of people who lose 20+ lbs (without surgery) ultimately regain it, and only 5% keep it off. Patients who undergo Bariatric surgery, on the other hand, experience a weight loss of 65-70 lbs on average, and are 10X more likely to keep it off in comparison to traditional weight-loss diets. In fact, over 60% of patients who undergo this surgery are able to keep this off for 15+ years, and they lose, on average, 70% of their excess weight. Meanwhile, only 3.4% of patients regained the weight within 10 years post-surgery!
Obesity in lipedema patients should be addressed prior to liposuction for lipedema because about 10% of patients regain their fat in the treated areas – especially those who have a higher BMI. Lipedema and obesity experts are finding that post-surgical growth of lipedema tissue can affect a staggering 30% of patients, so ultimately patients are more likely to have a recurrence of lipedema fat if treated prior to addressing their obesity. And Bariatric surgery is the most successful treatment for obesity in these patients by far.
I’ve recovered from bariatric surgery. Now what?
After fully recovering from your bariatric surgery, it’s important to do two things. First, maintain a healthy diet and exercise routine, following the anti-inflammation-based diet mentioned below, and exercising daily for about 30 minutes a day. Below is an example of what a daily meal plan should look like.
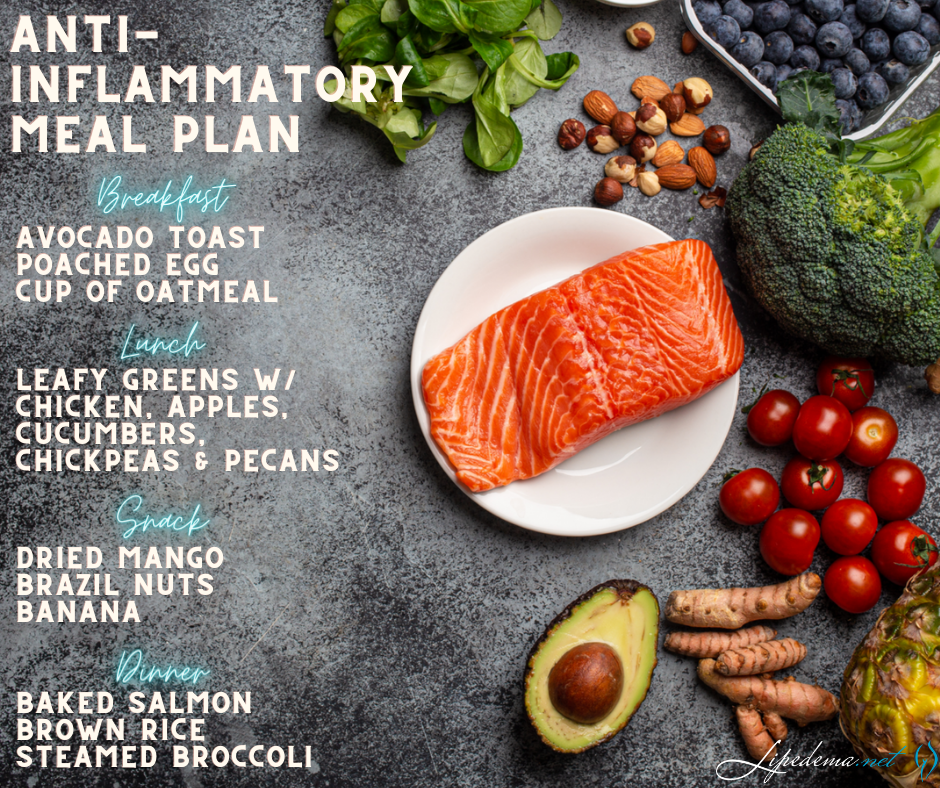
While continuing this practice, you should also start working towards your official lipedema diagnosis, if you don’t already have one. As you continue your post-bariatric surgery lifestyle, you’ll want to start working towards a lipedema treatment plan. Bariatric surgery will help with your underlying lipedema, but most of the time it is not enough in treating it. Now that you’ve freed your body of the obesity-related fat, it means you’ll have greater success in ridding your body of the painful, swollen, stubborn lipedema fat.
Getting a Lipedema Diagnosis: Symptoms Checklist
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
Lipedema Symptoms Checklist:
☑Tender skin that is sensitive to the touch, feels pressure when walking or climbing stairs, crossing your legs, or sitting for long periods of time.
☑Skin’s surface feels nodular and firm, like beans in a bean bag or rubber balls.
☑Skin’s surface is uneven, with large bulges and valleys up and down. Areas that were traditionally thought of as cellulite are much more dramatic and bulging.
☑Skin’s temperature is relatively cool.
☑Legs feel heavy and tired.
☑Swelling in the affected area (legs, arms), worsening during the day, and better at night after you’re able to elevate your limbs (such as laying in bed).
☑Easy bruising.
☑Visible veins.
☑Disproportionate fat accumulation, not affected by calorie restriction. Think extreme “pear-shaped” body.
☑Feet and hands are unaffected by weight gain or swelling. As a result, there’s often a “cuff” at the ankles or wrists.
Check out these resources for how to best address the next steps of diagnosis, non-surgical treatment options while you wait for lipedema surgery, and what to expect from lipedema surgery as well.
- Non-Surgical Lipedema Treatment
- Liposuction for Lipedema
- Life After Lipedema Surgery
- Before & After Lipedema Gallery
Contact Dr. Wright today if you have questions or would like to set up a consultation – his team is available to help guide you wherever they can!
Sources
- Bertsch T, Erbacher G. Lipoedema: a paradigm shift and consensus. Journal of Wound Care 2020;29:2-52.
- Cellina M, Gibelli D, Soresina M, et al. Non-contrast MR Lymphography of lipedema of the lower extremities. Magn Reson Imaging 2020;71:115-24. [published Online First: 2020/06/21 06:00]
- Crescenzi R, Donahue PMC, Weakley S, et al. Lipedema and Dercum’s Disease: A New Application of Bioimpedance. Lymphat Res Biol 2019;13(10)
- Guyton AC. Pressure-volume relationships in the interstitial spaces. Invest Ophthalmol 1965;4(6):1075-84.
- Herbst KL, Kahn LA, Iker E, et al. Standard of care for lipedema in the United States. Phlebology2021;28(2683555211015887):2683555211015887. [published Online First: 2021/05/30 06:00]
- Pessentheiner AR, Ducasa GM, Gordts PLSM. Proteoglycans in Obesity-Associated Metabolic Dysfunction and Meta-Inflammation. Frontiers in Immunology 2020;11(769) doi: 10.3389/fimmu.2020.00769
- Gould DJ, El-Sabawi B, Goel P, et al. Uncovering Lymphatic Transport Abnormalities in Patients with Primary Lipedema. J Reconstr Microsurg 2019;23(10):0039-1697904.
- Forner-Cordero I, Olivan-Sasot P, Ruiz-Llorca C, et al. Lymphoscintigraphic findings in patients with lipedema. Rev Esp Med Nucl Imagen Mol 2018;37(6):341-48. doi: 10.1016/j.remn.2018.06.008. Epub 18 Aug 28.
- Dudek JA-O, Białaszek W, Gabriel M. Quality of life, its factors, and sociodemographic characteristics of Polish women with lipedema. 2021(1472-6874 (Electronic))
- Herbst KL, Hansen EA, Cobos Salinas LM, et al. Survey Outcomes of Lipedema Reduction Surgery in the United States. PRS Global Open 2021;9:e3553 doi: 10.1097/GOX.0000000000003553
- Gensior MHL, Cornely M. Der Lipödemschmerz, seine Folgen auf die Lebensqualität betroffener Patientinnen – Ergebnisse einer Patientenbefragung mittels Schmerzfragebogen [Pain in lipoedema, fat in lipoedema and its consequences: results of a patient survey based on a pain questionnaire]. Handchir Mikrochir Plast Chir2019;51:249–54.
- Wold LE, Hines EA, Jr., Allen EV. Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann Intern Med 1951;34(5):1243-50.
- Di Renzo L, Cinelli G, Romano L, et al. Potential Effects of a Modified Mediterranean Diet on Body Composition in Lipoedema. Nutrients 2021;13(2) [published Online First: 2021/01/29 06:00]

