June is Lipedema Awareness month, one in which the Lipedema community focuses (even more than usual) on how to reach women who have lived with this painful and distressing disease. While we’ve seen great strides in awareness, insurance coverage, and slightly greater recognition of this disease in the medical community, we continue to fight an uphill battle as women are underdiagnosed or completely dismissed when discussing their struggles and side effects with their providers. As a result, our team has put together some of the most important and most impactful information for all of you! Read it, re-read it, and share it with the women in your life. Some of the pain we’ve lived with for decades may actually have a life-changing solution!


What is Lipedema?
Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.


Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper Lipedema diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
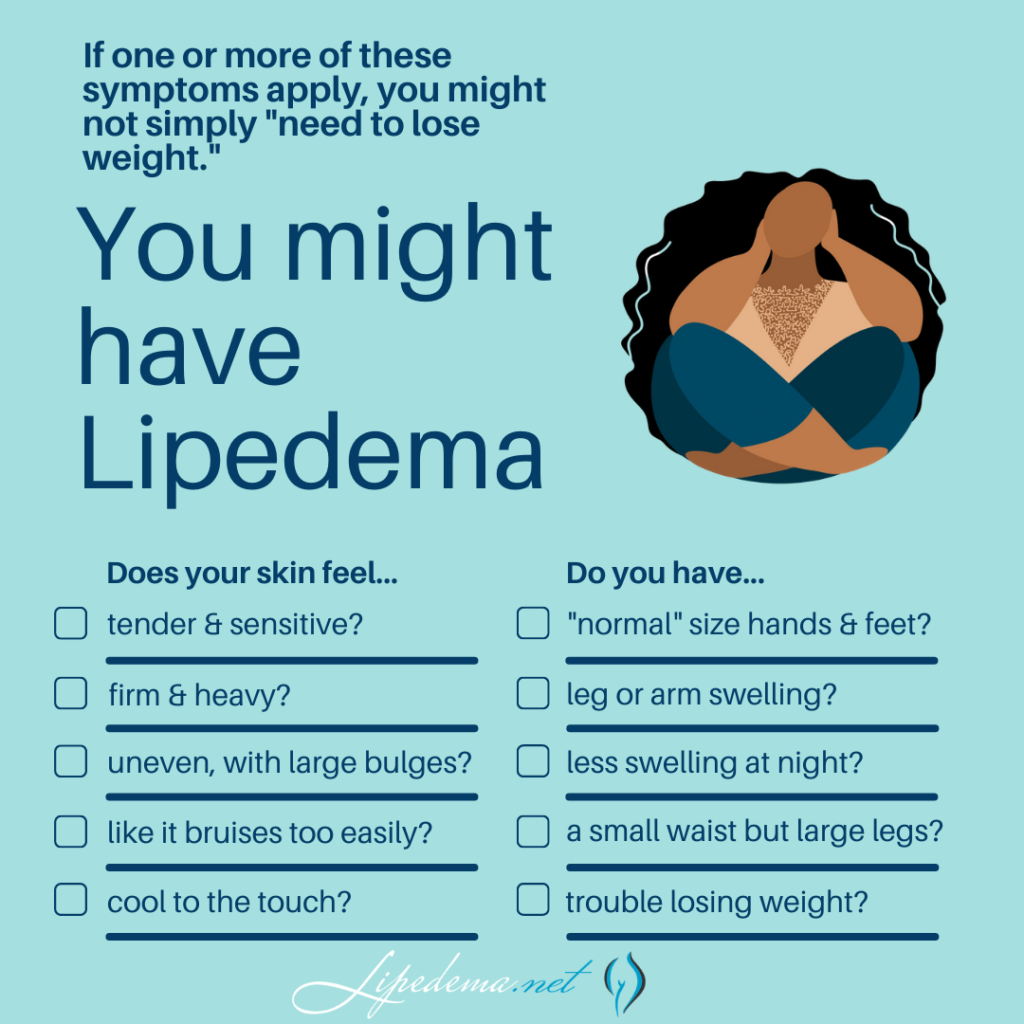
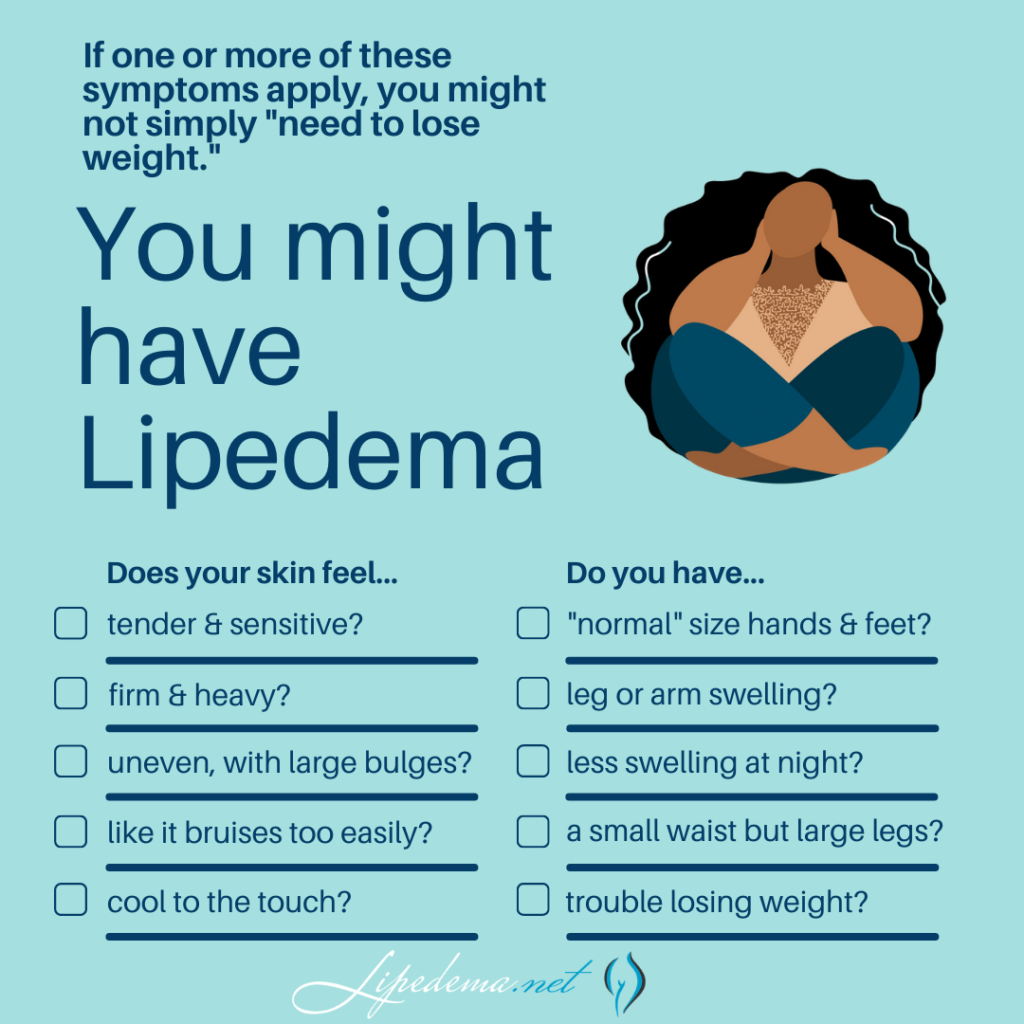
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
Lipedema Symptoms Checklist:
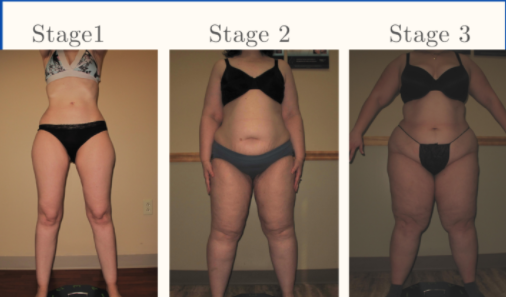
3 Stages of Lipedema
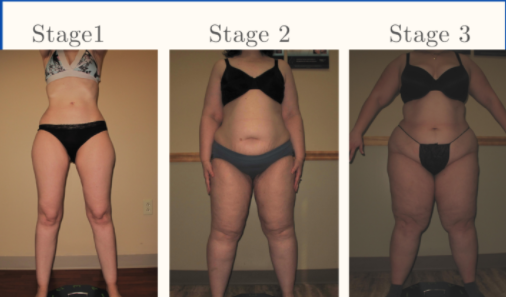
Overall, Lipedema appears in a series of three stages. Do any of these sounds like you?
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like a pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them. If you’re diagnosed with one of these conditions but you feel strongly that the diagnosis is incorrect, these summaries can help highlight why.
Lymphedema
While Lipedema typically does not have to swell in the patient’s feet and hands, Lymphedema will always have swelling in these areas. Lipedema symmetrically affects both legs equally, but Lymphedema usually affects one leg or arm and leaves the other leg or arm unaffected. There may be overlap in these two diseases and treatments can be similar, but some patients only experience Lymphedema after their Lipedema progresses into later stages.
Obesity
Obesity is much more common than Lipedema, and the most common misdiagnosis for it. While obesity is the accumulation of excess fat, stored centrally inside the abdomen or belly, Lipedema is the excess accumulation of fat out of proportion on the extremities, and typically not in the abdomen or belly. There may be overlap in these two conditions, too. In fact, sometimes obesity develops as a secondary condition due to the mobility problems caused by the Lipedema. So, not only is lipedema often misidentified as just obesity, but obesity can also complicate Lipedema, and be a symptom of it.
Venous Insufficiency and Veno-Lipo-Lymphedema
The symptoms of Lipedema and venous insufficiency are similar. They both cause heaviness, tenderness, fatigue, and swelling. They often both have discoloration in the shins, easy bruising, and prominent veins. In more advanced cases of venous insufficiency, not only does venous lymphedema develop, but a secondary Veno- Lipo- Lymphedema develops. With the overwhelmed lymph circulation, the ability to clear fatty acids from the affected tissue is compromised and a secondary fat accumulation occurs. In many cases, the best way to differentiate between lipedema and venous insufficiency and veno- lipo-lymphedema is to have a specialized standing venous Doppler ultrasound to check for venous reflux.
Getting a Lipedema Diagnosis & Next Steps
Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time to find a Lipedema specialist and get tested! Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
Note: There is no single test to diagnose Lipedema. Tests, however, are important to rule out a related disorder.
Stemmer’s Sign Test
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
Venous Doppler Ultrasound
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema. Lipedema has many similarities to venous insufficiency (as explained above), so this can help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. Unfortunately, most hospital vascular labs complete Venous Doppler Ultrasounds with the patient lying down, While this is the typical way to find Deep Vein Thrombosis (DVT), it is definitely not a successful method to detect venous insufficiency. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
Lymphoscintigraphy
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
Life After Lipedema Diagnosis
First – congratulations! We know the road to diagnosis is emotionally draining, physically painful, and it can feel lonely and discouraging. The time and research it takes to make it to this point are huge, and you should be proud of yourself and the courage it takes to be your own advocate. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.


After going through the diagnosis process and receiving a positive Lipedema diagnosis, most patients are relieved, overjoyed, and validated by their endless search. After years of living with the private struggle and knowledge that “something just isn’t right” in their body, putting a name to the issues is a huge win. And after an official diagnosis, there are many different treatment paths available to you! A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, it can give you an idea of what options may be available to you. Good luck!