Getting an initial Lipedema diagnosis is a challenge for many women suffering from it. In fact, an overwhelming majority of patients seeking treatment are well into their forties, fifties, sixties, or later in age, simply because they had never heard of lipedema or been diagnosed with it. After decades of being diagnosed with a high Body Mass Index (BMI) followed by a general obesity diagnosis or misdiagnosed as lymphedema, some of these women with other diseases sought alternate explanations for their pain, discomfort, and unsuccessful weight loss, despite regular diet, exercise, and, in some advanced cases, even after undergoing bariatric surgery. Learn more about lipedema diagnosis below.
Lipedema: friend and foe: http://orcid.org/0000-0002-9079-9754. Department of Biological Sciences, University of Texas at El Paso, El Paso, TX, USA.
Fat tissue (also referred to as adipose tissue) provides the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, and in many cases, excessive clustering of fat cells is noticed in the arms as well.
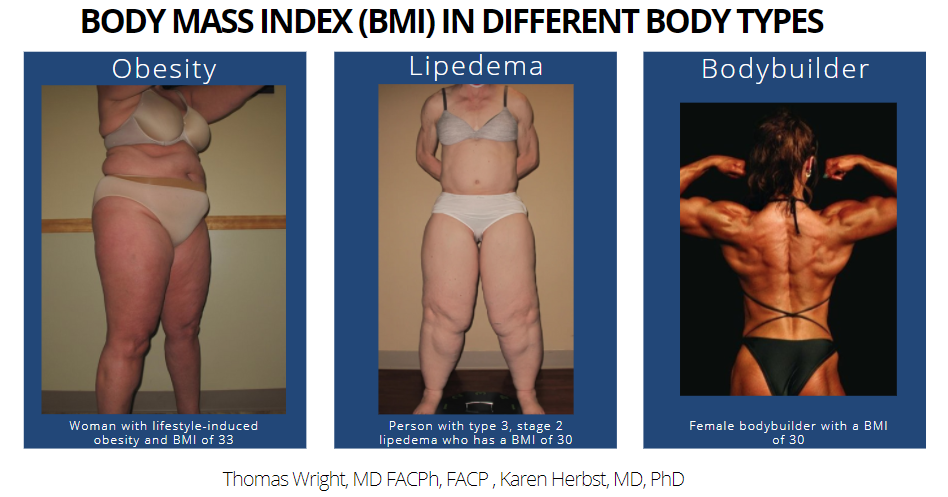
Lipedema vs. Obesity Using BMI
Body Mass Index (BMI) is a calculation that illustrates the relationship between a person’s weight and height, and equips healthcare providers with one tool in evaluating a patient’s overall health. Specifically, these ranges are used to categorize whether a person is underweight, in a normal weight range, overweight, or obese. While BMI does not provide the full picture of a patient’s health or the full body composition breakdown, it is a commonly used factor in diagnosing numerous diseases. Dr. Wright and fellow Lipedema expert Dr. Karen Herbst discuss this in greater detail with Vein Magazine here.
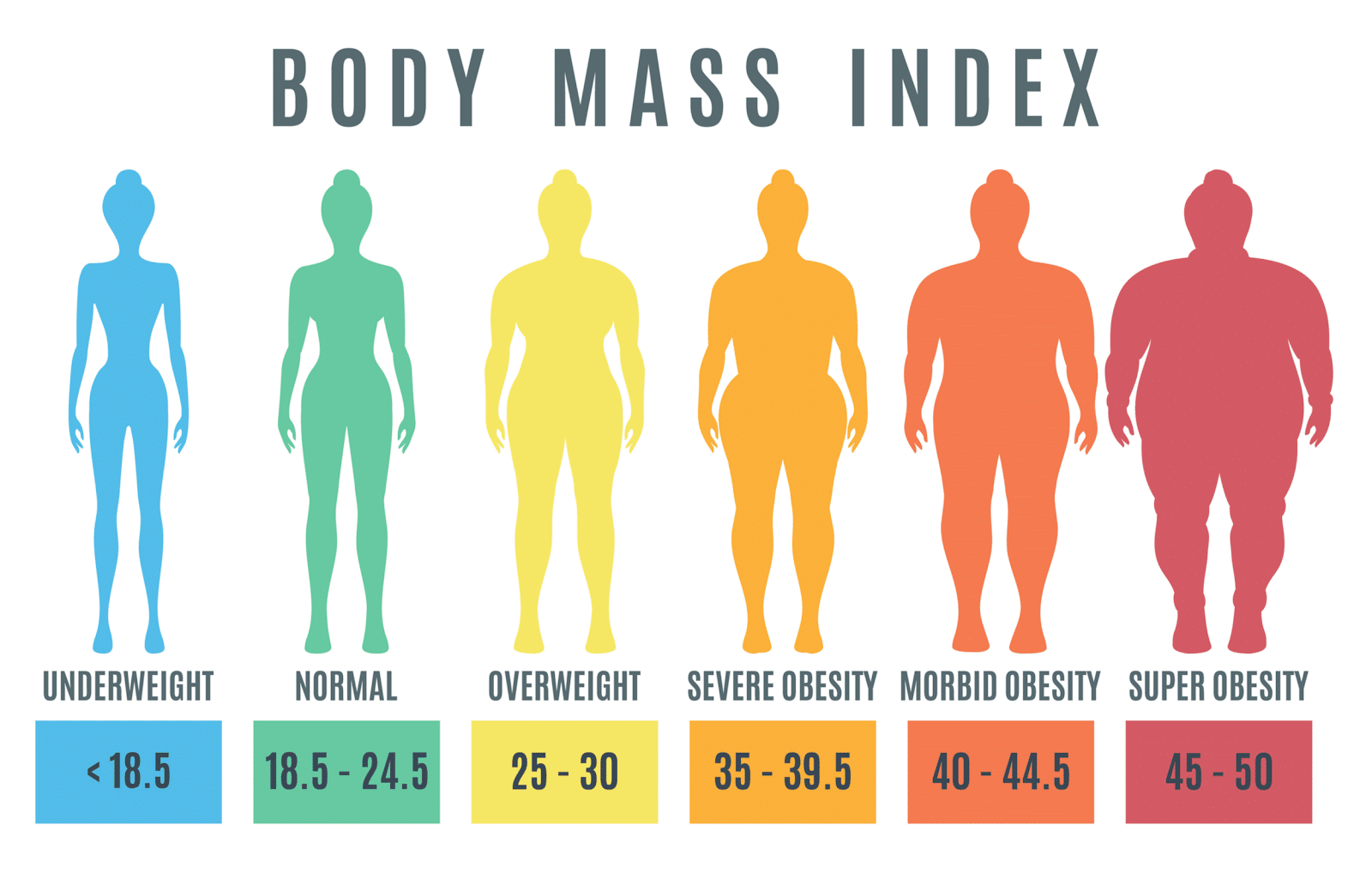
Body Mass Index (BMI) is simply an overall numerical score (like height and weight) which is not a biological representation of a person’s overall health. While the World Health Organization (WHO) defines a BMI over 25 as overweight and over 30 as obese, this is actually an inaccurate and incomplete assessment. Overall, obesity is a condition where fat mass affects patients metabolically, chemically, and mechanically (for example, in your joints).
However, Lipedema causes fat in a different proportion on the body and has different metabolic, chemical, and mechanical effects. Both obesity and Lipedema have increased BMIs, but they are not one and the same. When we use BMI as a blanket diagnosis, it’s an unfair and incomplete assessment.
As seen below, a female bodybuilder may have a higher BMI, but looking at their BMI number alone and diagnosing them as obese would be inaccurate. Similarly, while Lipedema will affect the BMI number, this BMI measure will not accurately pinpoint the cause of the higher measurement.
Lipedema is metabolically the opposite of obesity – both are associated with excess fat accumulation, however, obesity presents with fat accumulated in the central area of the body, primarily in the abdomen, and is associated with diseases such as diabetes, high blood pressure, high cholesterol, and cardiovascular disease. However, lipedema presents with peripheral fat in the extremities, while the abdomen and/or waist are typically unaffected. But because both diseases increase a patient’s BMI, misdiagnoses are common and destructive. This illustrates one reason why BMI is not a biologically valid way to diagnose obesity or lipedema.