Lipedema is a chronic condition that primarily affects women and is often misunderstood or misdiagnosed. It involves an abnormal buildup of fat cells in the legs and sometimes arms, resulting in a disproportionate, non-uniform shape. While there is no cure for lipedema, recognizing the symptoms early is crucial for proper management and improving quality of life. Here, we’ll explore the common symptoms of lipedema, ways to combat them at home, and when to consider lipedema reduction surgery.
Recognizing the Symptoms of Lipedema
Lipedema presents a range of symptoms that can vary from person to person. The following are common indicators, but it is important to note that while these symptoms are frequently associated with lipedema, a comprehensive evaluation by a healthcare professional is necessary for an accurate diagnosis.
- Disproportionate Fat Distribution: Disproportionate fat distribution in legs/arms with a “cuff” or “bracelet” appearance. A hallmark sign is the disproportionate fat accumulation in the lower body, particularly around the hips, thighs, and legs, while the upper body remains relatively unaffected.
- Swelling and Pain: Swelling and heaviness in the limbs are very common. Chronic swelling often persists even after resting or elevating the legs, accompanied by pain or sensitivity to touch. The pain may worsen after prolonged standing, physical activity, or in hot weather. Many have heavy, tired, and aching sensations in the legs and arms.
- Easy Bruising: The skin over the affected areas can bruise easily due to increased capillary fragility, even from minimal pressure.
- Tissue Texture Changes: Skin changes include dimpling, bumpiness, or thickening. As lipedema progresses, the fatty tissues may develop a nodular or lumpy texture.
- Cold Extremities: Affected limbs often feel cold to the touch, indicating circulatory disturbances. The skin and tissues may feel soft, flexible, and colder in the affected areas.
- Impaired mobility: As lipedema progresses, it becomes more difficult to combat the pain and swelling, often leading to secondary obesity and making mobility and staying active more difficult.
- Vein issues: Spider or varicose veins may be present in the affected regions.
- Psychological effects: Anxiety, depression, and low self-esteem are commonly reported by women with lipedema, resulting from low quality of life and feeling helpless in their health journey.
Disproportionate Fat Distribution in Lipedema
Research indicates that lipedema develops through three distinct stages, each characterized by noticeable skin and lipedema tissue changes. Most women don’t experience significant fat accumulation around the face, neck, feet, or hands. Instead, fat buildup commonly occurs below the shoulder line and on the front of the chest.
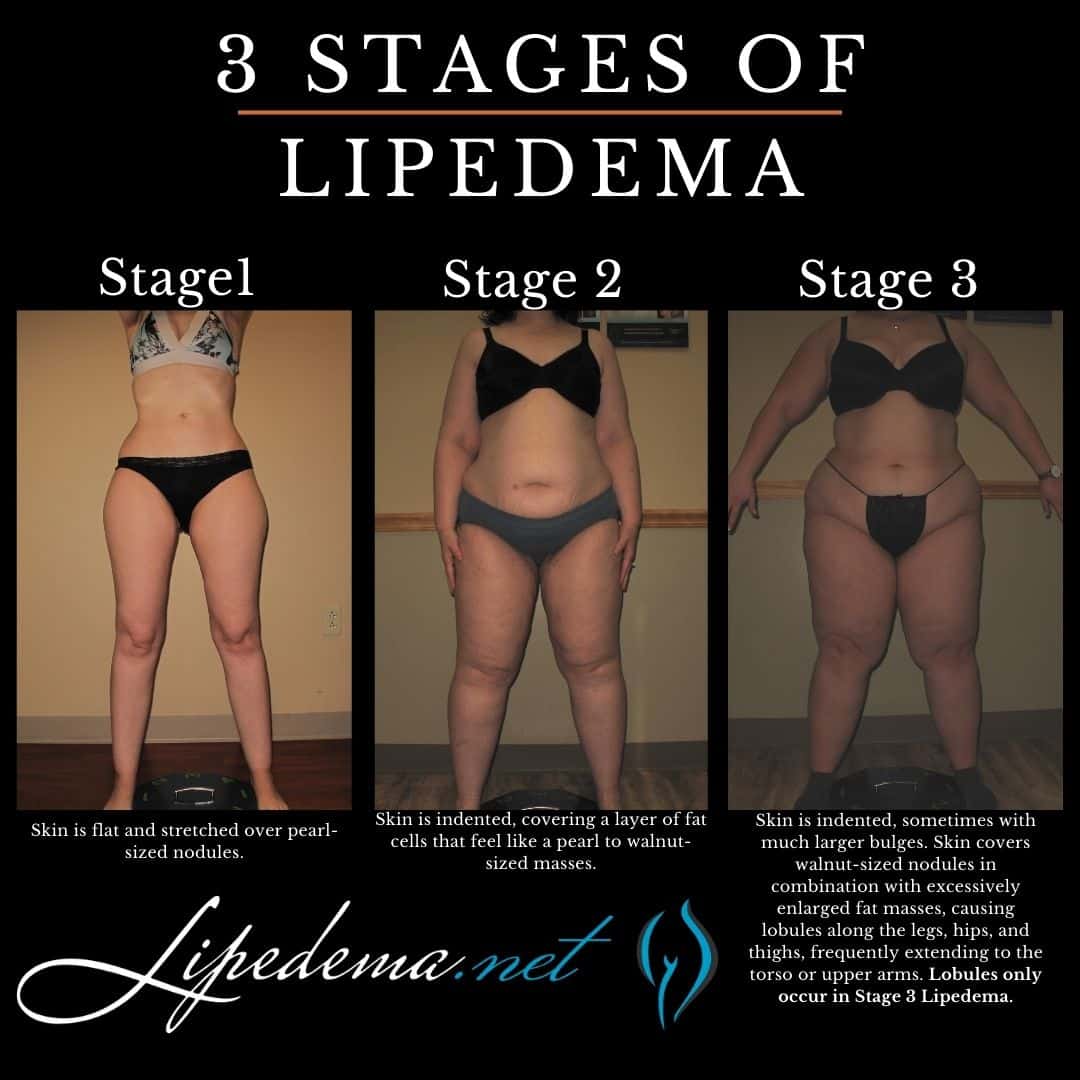
The upper body, including the torso, abdomen, and arms, generally accumulates less fat. However, over 90% of women with lipedema will have fat buildup around the inner elbow, forearm, and upper arm. The lower body, particularly the thighs and buttocks, tends to be the primary site of fat accumulation. Women also often notice significant fat deposits around the inner knee and the back of the legs in these regions. Learn more about the stages and types of lipedema here.
Tissue Texture Changes: Lipedema Lobules & Nodules
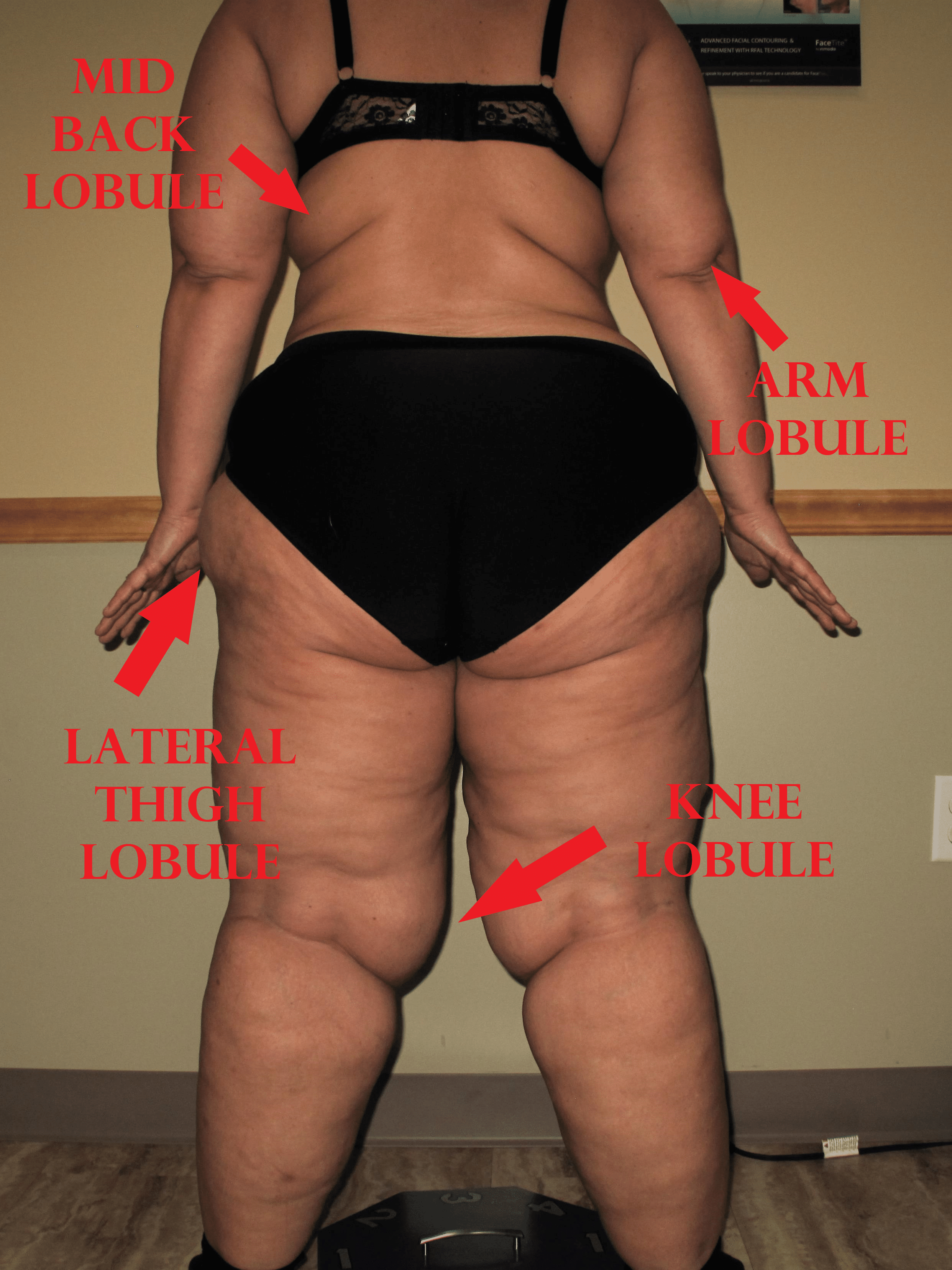
In the later stages of lipedema, lobules develop in the skin. The presence of a lobule is one of the most important physical changes to occur in the skin, and it differentiates between stage 2 and stage 3 lipedema. Dr. Schmeller described a lobule as a “hanging flap of skin,” also called an “extrusion of skin that protrudes or sticks out from the expected smooth contour of the skin.” Lobules can be seen from a distance.
The lobules can occur in many areas of the body in lipedema patients. Still, the classic areas are just below the knees, or subpatellar lobules, lobules that hang over the knees, inner thigh lobules, lateral thigh lobules, and upper arm lobules. Some lipedema experts think these lobules are diagnostic of lipedema.
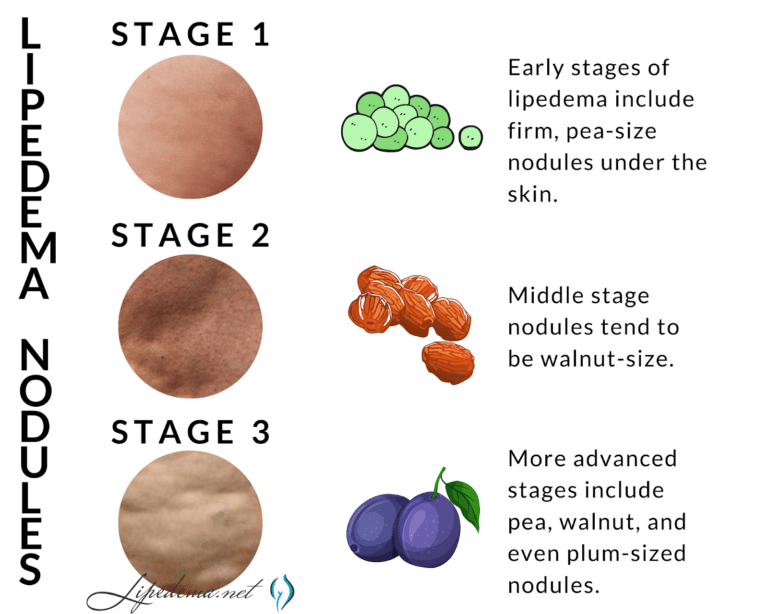
Lipedema nodules, on the other hand, are felt and not usually seen. In lipedema, the skin surface is soft, but the nodules can be felt as harder areas just below the surface. Early-stage Lipedema (Stage 1) has small nodules the size of small seeds or peas, which often appear pearl-size. Middle-stage Lipedema (Stage 2) has larger nodules that feel the size of walnuts or gumballs. The presence of lobules characterizes the later stage, Lipedema (Stage 3). The nodules in Stage 3 may be the same size as those in Stage 2 or larger up to the size of a plum.
The Lipedema nodules felt on the skin are important criteria for diagnosing Lipedema. Nodular or bumpy subcutaneous fat occurs with other conditions or diseases such as cellulite, obesity, and other fat disorders. However, subcutaneous nodules must be present to diagnose lipedema. These nodules represent excess and slightly disorganized fibrosis of the subcutaneous tissue. Inflammation of the adipose tissue in lipedema is likely the cause of this fibrosis.
Managing Lipedema Symptoms at Home
While medical intervention is vital, certain home-care practices can alleviate discomfort and help manage symptoms:
- Compression Therapy: Wearing compression stockings or wraps can help reduce swelling and improve blood flow.
- Exercise: Low-impact exercises like swimming or cycling can enhance lymphatic circulation and support muscle tone.
- Healthy Diet: A balanced diet low in processed foods and high in anti-inflammatory nutrients may reduce symptoms. Aim for a diet rich in omega-3s, antioxidants, and fiber.
- Lymphatic Drainage Massage: Manual lymphatic drainage (MLD) or self-massage can gently encourage lymph flow and reduce swelling.
- Hydration: Staying hydrated is crucial for maintaining lymphatic function.
Compression Garments for Lipedema
Compression garments are generally prescribed to lipedema sufferers following decongestive therapy to help maintain the reduction of swelling. Compression therapy also helps encourage the flow of lymphatic fluids out of the affected limb. Compression garments assist lymph circulation by increasing the pressure in the tissue and propelling lymph fluid through the body.
In most people with lipedema, swelling and activities such as standing for long periods worsen the pain and tenderness. Compression garments can help reduce limb pain and heaviness by decreasing swelling. Also, compression potentially reduces the rate at which the fat cells grow and helps prevent fat disorders from progressing to more serious stages.
Compression garments are to be worn 24 hours a day, every day. Because of this, patients must be fitted correctly and use the best type of compression garment for their cases. An inaccurate fit or a poor-quality garment can cause additional pain and discomfort. Patients should discuss which type of compression garment is appropriate with a lipedema specialist and ensure they are properly fitted with medical-grade compression garments. Read more about compression garments for lipedema here.
Exercise for Lipedema
Exercise for lipedema can help activate the lymphatic drainage system in a patient’s limbs through the foot and calf muscle pump. Workouts that aren’t too strenuous help move the excess fluids out of affected limbs and reduce additional fat buildup.
The lymphatic system differs from the arterial circulatory system in that it does not have a muscle “pump” to move fluids into the lymphatic system. The venous system and lymphatic system rely on the passive motion of muscle contractions to aid in the propulsion of their fluids. Additionally, the larger vessels’ lymphatic system has lymphangions that further aid in lymphatic flow. Because lymphatic flow depends on muscle and body movement, exercise is critical to optimal lymphatic flow. This is especially true if the lymphatic system is compromised.
The best lipedema exercises to help treat lipedema are low-impact exercises that aren’t too strenuous, as strain can increase fatigue and pain. Low-impact exercises also help protect joints and are less likely to increase lactic acid build-up. Individuals suffering from lipedema can greatly benefit from yoga, water aerobics, diaphragmatic breathing exercises, and strength training. Exercising in water has a special benefit for women with lipedema because, in addition to muscle contraction, the water pressure acts as a naturally graduated compression.
Nutrition & Hydration for Lipedema
Nutrition plays a key factor in how and when your body experiences edema (swelling), and a large player in this experience is in response to diet & hydration. Read more about a lipedema diet, which you can follow here.
The Rare Adipose Disorder Diet (AKA RAD Diet)
Dr. Wright recommends following a Rare Adipose Disorder (RAD) diet, a modification to a standard Mediterranean diet that helps you maintain a low glycemic index to limit the number of occurrences and levels your blood sugar spikes through the day. To do this, it is recommended that you avoid any refined or processed starches and sugars. These are usually found in pasta, rice, bread, corn, and potatoes. Avoiding processed food – especially processed carbohydrates – will keep your insulin levels low and provide you the best chance of limiting inflammation.
It is also recommended that individuals with lipedema should reduce dietary inflammation triggers. The dietary triggers of inflammation vary from individual to individual and must be investigated through systematic trial and error. Many lipedema patients have gluten or dairy sensitivities. Gluten is typically found in wheat, rye, and barley. If you have gluten sensitivity, make sure your lipedema diet focuses on foods high in omega-3 fatty acids and are also high in fiber to assist your body in burning fat and fighting inflammation. Focus on colorful foods, like nuts, beans, fish, and whole grains.
Manual Lymph Drainage for Lipedema
Manual lymph drainage is just one component of complete decongestive therapy (CDC), which includes MLD, compression, exercise, and skincare. When performed together, these therapeutic components can ultimately lessen painful lipedema symptoms. This practice increases the capacity of the lymphatic system, which then lets it process more fluid than usual. It increases the flow through the lymph nodes, allowing the system to filter out waste, dead cells, excess proteins, and toxins. The production of lymphocytes will also increase to heighten the body’s ability to fight infections. Learn more about performing lymphatic drainage massages for lipedema here.
Seeking Medical Attention for Lipedema
For some with advanced lipedema, conservative management may not provide adequate relief. You may want to discuss surgical intervention with a qualified surgeon if:
- Symptoms significantly impact your mobility and quality of life
- At-home treatments provide little to no relief
- Skin conditions like deep folds, leakage, or infections develop
- Excessive weight and pain make performing daily tasks difficult
In these cases, lipedema reduction surgery, such as lymph-sparing liposuction procedures, could be an option to remove excess fat build-up. However, surgery does not cure the root cause, and lifestyle changes are necessary for long-term management.
While lifestyle adjustments are beneficial, there are times when consulting a healthcare professional is essential:
- Increased Pain or Swelling: If pain or swelling intensifies despite home care, it may indicate worsening lipedema or complications.
- Restricted Mobility: When mobility becomes limited due to swelling, stiffness, or pain, it may warrant further assessment.
- Infection Signs: Fever, redness, or warmth over the affected areas may indicate an infection requiring prompt medical attention.
- Mental Health Impact: Lipedema can significantly affect self-esteem and mental health. Support groups and counseling can provide emotional assistance.
Considering Lipedema Reduction Surgery
Lipedema reduction surgery, also called lymph-sparing liposuction, can effectively reduce the excess fatty tissue. Finding a surgeon experienced in lipedema treatment is crucial, as improper techniques could worsen the condition. You can find more information about finding the best lipedema surgeon here.
The decision to have surgery is highly personal, and one should consider the potential risks, recovery process, cost, and likelihood of symptom improvement.
If you notice any potential lipedema symptoms, don’t hesitate to consult a lipedema specialist. Early intervention provides the best chance of effectively managing this condition. You can take steps toward improving your comfort and mobility through a combination of self-care strategies and working closely with your care team.
- Confirm Diagnosis: Ensure a certified specialist diagnoses lipedema to rule out other conditions that can look like lipedema.
- Evaluate Health: Have a thorough health evaluation to identify any underlying issues that could affect the surgery.
- Understand Risks and Benefits: Discuss the potential risks, expected outcomes, and long-term results with your surgeon.
Final Thoughts
Managing lipedema requires a comprehensive approach that combines lifestyle adjustments with medical expertise. Early identification, proper home care, and timely medical intervention can alleviate symptoms and improve the quality of life for those with this condition. Stay informed, reach out for support, and seek guidance from healthcare professionals to develop a personalized care plan that best suits your needs.
