
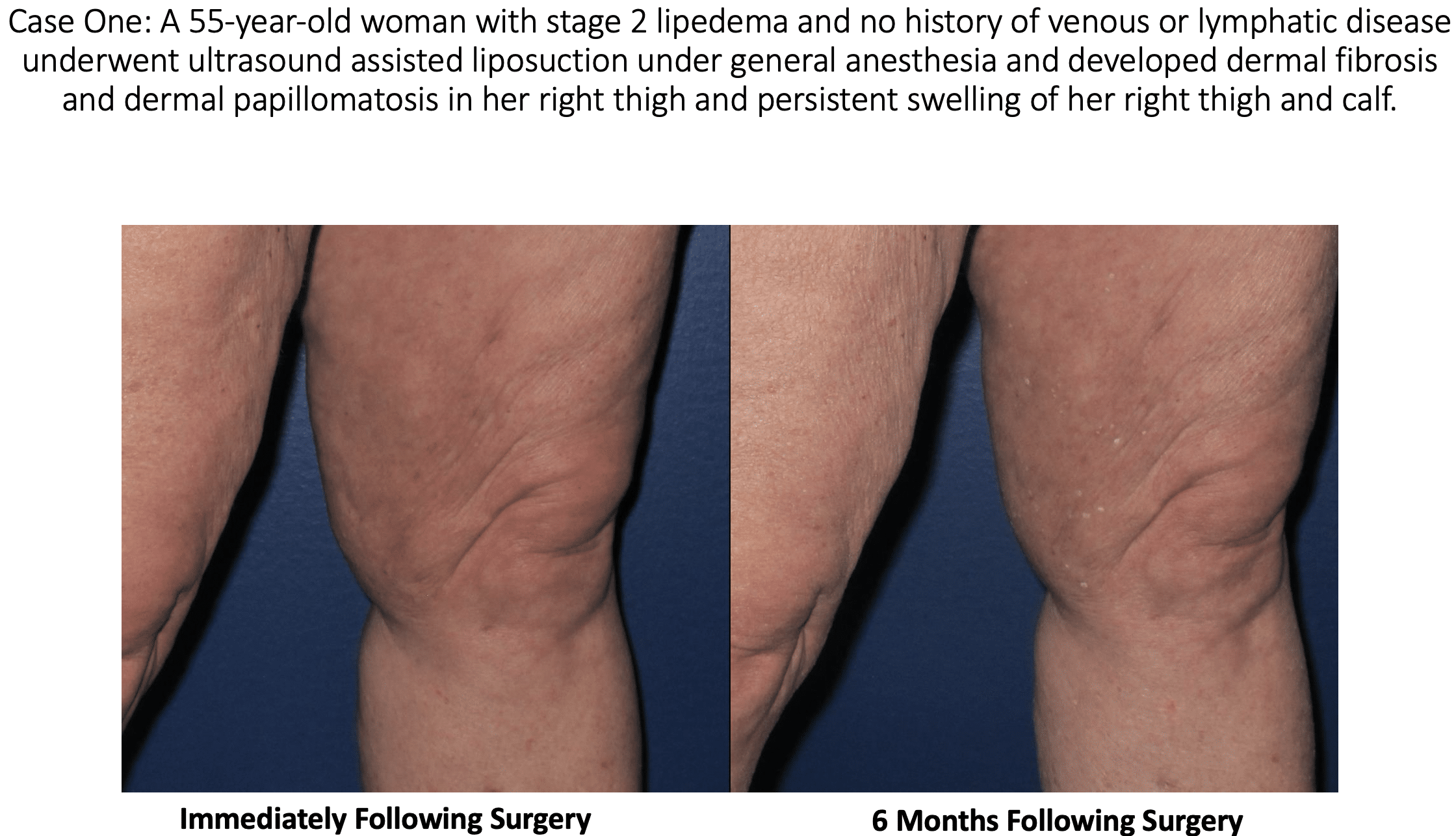
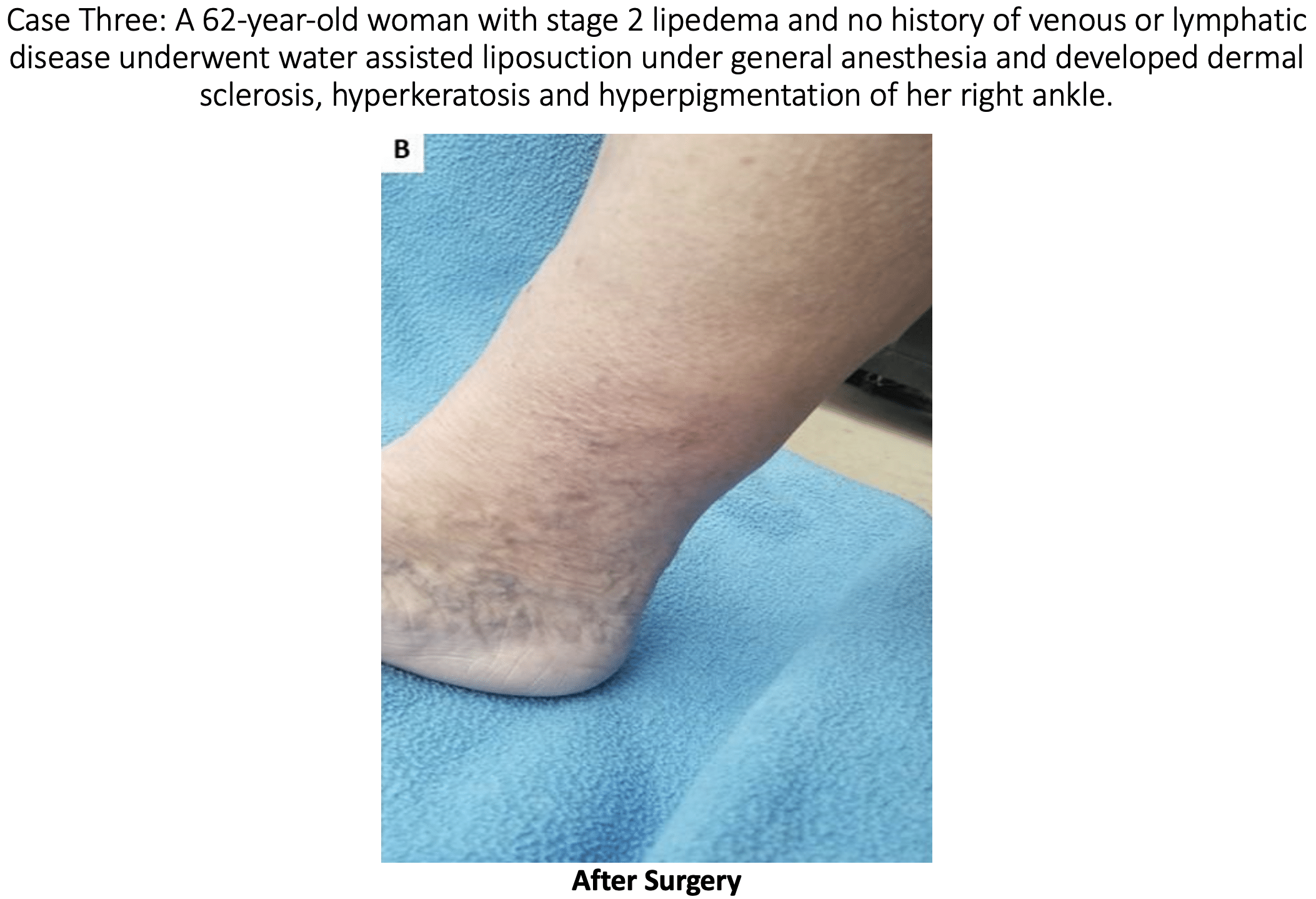
At this year’s annual congress of the American Vein and Lymphatic Society (AVLS), Dr. Wright presented an abstract on lymphatic injury after suction lipectomy in patients with lipedema. The abstract consisted of three cases of patients who had been diagnosed with lipedema and underwent suction lipectomy with ultrasound, power, or water assistance. Immediately after lipo, the patients appeared to recover normally; however, over a 3 to 6-month period, they developed skin changes and symptoms consistent with the lymphatic injury after liposuction. Specifically, the patients developed skin lymphostatic fibrosis, papillomatosis, dermal sclerosis, and leg swelling. Find greater detail from Dr. Wright’s AVLS 2021 lymphatic injury liposuction presentation, and follow along to see prior year’s information below.
Possible Side Effects from Lymphatic Injury after Liposuction
Skin Lymphostatic Fibrosis:
This is a widespread side effect in patients with lymphedema, where the skin hardens over time. In the early stages of lymphedema, swelling is soft to the touch. However, over time, the swelling hardens the skin due to the development of connective tissue fibers underneath the skin of the affected areas.
Papillomatosis:
The growth of numerous papillomas, more commonly referred to as warts.
Dermal Sclerosis:
Hardening and tightening of the skin and connective tissues.
Leg Swelling:
Ironically, leg swelling is one of the most common symptoms of lipedema and prompts patients to seek treatment. Post-lymph-sparing liposuction for lipedema, lymphatic injury after liposuction can lead back to leg swelling.
At this time, most experts believe that suction lipectomy with ultrasound, power, or water assistance techniques, in the proper hands, are safe and effective treatments for lipedema, as long as the surgeon performing the liposuction has skill and experience to perform a lymph sparing technique. When suction lipectomy is performed properly, it improves symptoms, lymphatic flow, and skin health. Studies have shown that lipedema is often associated with lymphatic impairment. Studies have also shown that lymphatic function is not changed or improved with careful liposuction that uses surgical techniques and technologies that protect or minimize lymphatic injury after liposuction. We do know that traditional liposuction, without special care of the lymphatics or proper tumescent technique, can cause lymphatic damage and possibly worsen lipedema symptoms.
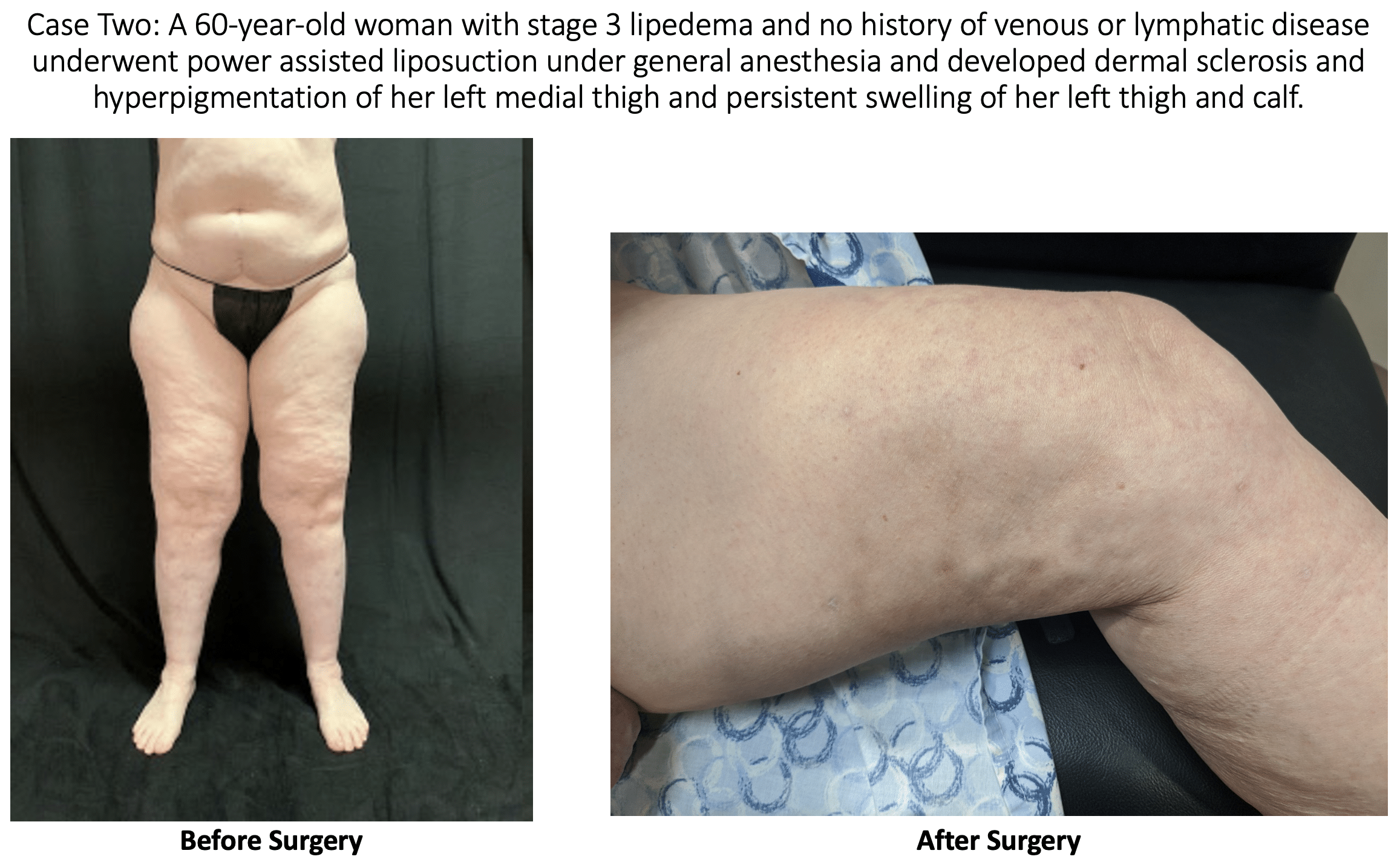
The skin changes experienced by the above patients were not present prior to the surgery. The changes seen in these patients are consistent with stage 2 or stage 3 lymphedema. We are left to conclude that the lymphedema changes in the skin were most likely the result of surgical trauma during suction lipectomy. Doctors A. Frick, C.C. Campisi, and others have shown that there are surgical techniques that can limit the risk of lymphatic injury after liposuction. [1,2] These case reports show the importance of choosing a surgeon that will take every precaution to not injure lymphatics
Why Does Lipedema Occur?
The cause of Lipedema is unfortunately unknown, but it almost entirely occurs in women after puberty or some kind of hormonal change. It mostly affects overweight or obese people, and sometimes normal-weight individuals. You can learn more about Lipedema causes here.
1 Frick A, Hoffmann JN, Baumeister RG, Putz R. Liposuction technique, and lymphatic lesions in lower legs: anatomic study to reduce risks. Plast Reconstr Surg. 1999 Jun;103(7):1868-73; discussion 1874-5. doi: 10.1097/00006534-199906000-00009. PMID: 10359247.
2 Campisi CC, Ryan M, Boccardo F, Campisi C. Fibro-Lipo-Lymph-Aspiration With a Lymph Vessel Sparing Procedure to Treat Advanced Lymphedema After Multiple Lymphatic-Venous Anastomoses: The Complete Treatment Protocol. Ann Plast Surg. 2017 Feb;78(2):184-190. doi: 10.1097/SAP.0000000000000853. PMID: 27404468
