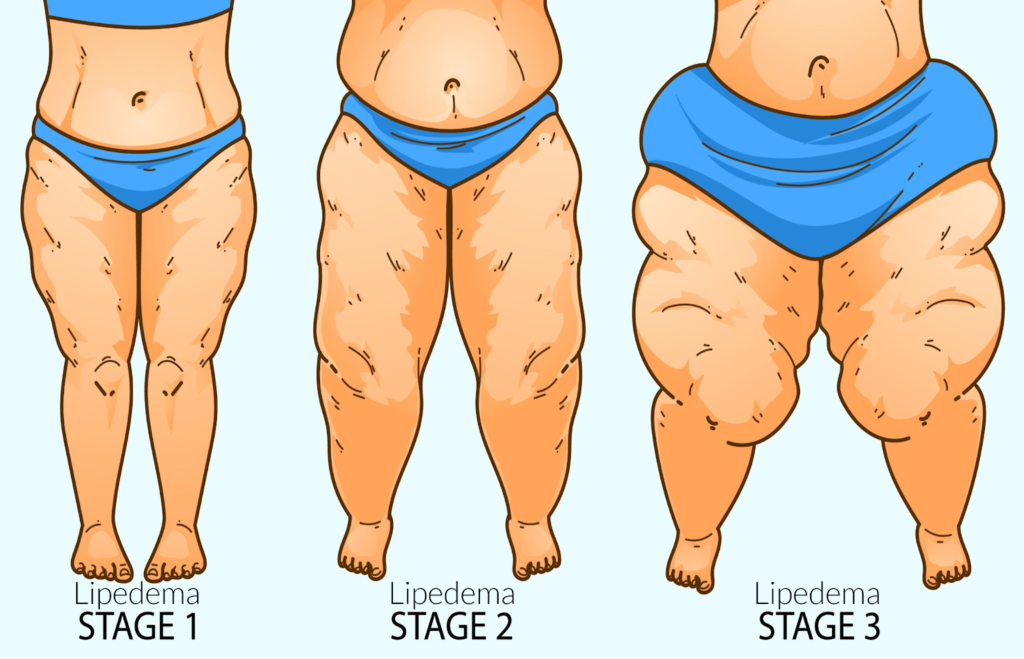
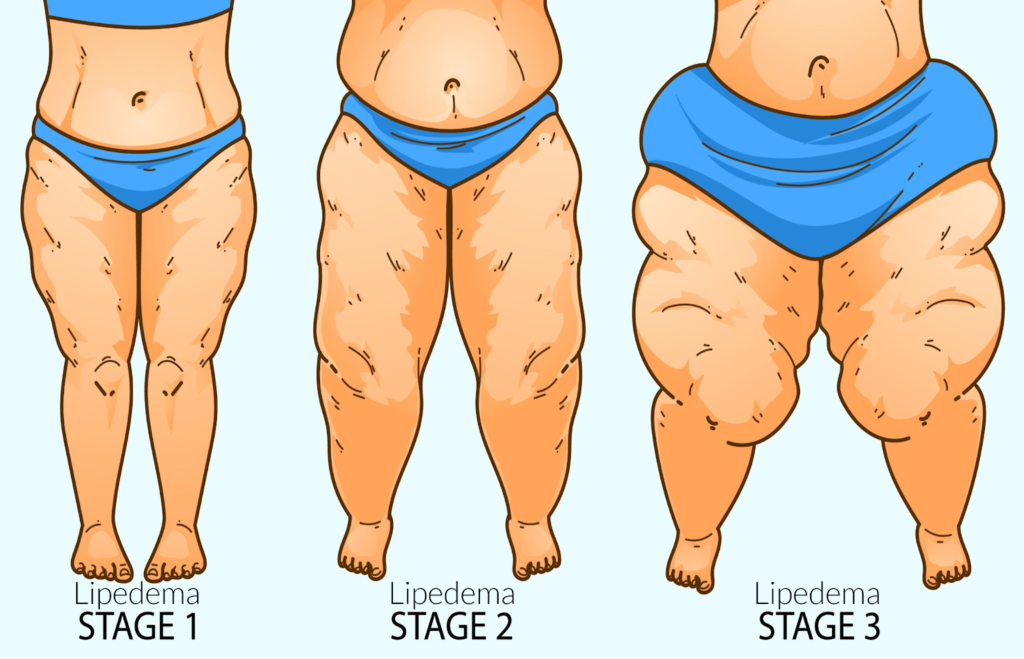
Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. Sufferers living with lipedema experience easy bruising and tenderness, pain in the affected areas, and significant disability in daily life. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back. Little is known about the disorder, and it’s often misdiagnosed and incorrectly treated as general obesity.
For anyone affected, diet and exercise alone aren’t effective ways to get rid of Lipedema fat; Lipedema fat has proved relatively immune to these lifestyle changes and won’t budge. While women are likely to experience some weight loss with a healthy diet and regular exercise routines, weight loss is usually mostly loss of non-Lipedema fat. In these instances, the painful, stubborn fat remains. This cycle becomes a difficult one to break for those with the disorder: Yo-yo dieting leads to more weight gain. More weight gain leads to increased pain and disability. Increased pain and disability make it more challenging to manage mobility and secondary obesity increases. Lipedema fat also appears to be relatively resistant to bariatric surgery, meaning many women are undergoing dangerous surgeries without experiencing the intended benefit of significant loss of lipedema fat. Read on below to learn more about lipedema medication.
Lipedema vs. Obesity
Unlike common obesity, Lipedema is comprised of fat deposits and swelling that typically does not affect the feet or hands; it’s as if patients are wearing a tight bracelet or rope at their wrists or ankles that causes every above to swell and everything below to remain unaffected. At more progressive stages, the swelling increases and leads to a diagnosis of lymphedema, which makes it even less likely Lipedema is diagnosed and treated promptly and adequately.
Despite the strong impact of Lipedema on millions of women across the world, only limited research exists to determine its cause. In many cases, the genetic background can provide some context, but enough research has yet to offer a comprehensive understanding of the disease.
Dr. Wright and his team at St. Louis Laser Lipo & Vein Center have put together a helpful list of Lipedema Do’s and Don’ts for living with this difficult disease.
Take This Cold Lipedema Medication Regularly
Guaifenesin, best known by the brand name Mucinex©, and often prescribed as an over-the-counter expectorant to treat the common cold, may help reduce lipedema swelling and inflammation.


To our knowledge, there are no published, controlled studies showing the use of Guaifenisn to treat lipedema or lymphedema. However, there are abundant reports from clinicians and lipedema patients stating that Guaifenisn helps lipedema. In our limited clinical experience, about 20 – 30 % of lipedema patients report reduced pain and/or swelling when taking this Lipedema medication. Plus, there are reports of Guaifenisn being used for pain relief to treat other diseases. Guaifenesin has shown modest but significant analgesic and anti-inflammatory effects in neck and back pain and some other conditions. It is thought guaifenesin may be working as a muscle relaxant effect that occurs in these conditions. Mucinex / guaifenesin may help pain or it may work as an expectorant in lipedema tissue and thin out extracellular proteins. However, there are no studies to support these theories in lipedema.
Guaifenesin Medication for Lipedema: Dose and Use
Guaifenesin is approved for safe use at 600 mg twice a day (or 1,200 mg twice a day) for no more than 2,400 mg per day. Studies in the use of Mucinex for other medical conditions report it takes a least a week to see effects. I recommend lipedema suffers try this medication for Lipedema for two weeks to see if they notice any positive changes in addition to their consistent treatment plans including compression, supplements, and a healthy diet as prescribed. May not be suitable for people with a persistent cough due to asthma, bronchitis, emphysema, or smoking, or who have a cough that is producing excessive amounts of phlegm. Talk with your doctor first before using Mucinex if you are pregnant or breastfeeding.
Use Diosmin to Combat Lipedema
Diosmin is a flavonoid extract made from orange peels used to treat vein disease. Diosmin helps reduce inflammation along vein walls in people with chronic venous insufficiency and it can also have very positive results for people with lipedema and lymphedema.


Benefits
- Reduces white blood cell activation, migration, and adhesion
- Decreases capillary permeability and stimulates lymphatic flow
- Less leg heaviness, swelling, and tenderness
- Diosmin infused intravenously results in a nearly 200% increase in measured lymphatic flow
In a recent case study, Diosmin had positive results when used in combination with other supplements, diet, compression, and other anti-inflammatory measures to non-surgically manage lipedema. Based on these studies, and my experience prescribing Diosmin to patients, I recommend Diosmin as part of an overall conservative management treatment plan for lipedema and lymphedema.
Where to Get Diosmin for Lipedema
In the United States, Diosmin is sold under the brand name Vasculera, which is available in pharmacies by prescription from a physician. Vasculera is approved by the FDA as a medical food.
Diosmin is also available as a supplement without a prescription. We recommend Vein Formula, as we trust its formulation. Be sure to order any supplements from a reputable website for the best safety and quality.







