Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. Sufferers experience easy bruising and tenderness, pain in the affected areas, and significant disability in daily life. In severe and more progressive fat disorder cases, the trunk and upper body may also be affected, including the arms and upper back. Little is known about the disorder, and it’s often misdiagnosed and incorrectly treated as general obesity.
For anyone affected, diet and exercise aren’t an effective way to get rid of Lipedema fat; Lipedema fat has proved relatively immune to these lifestyle changes and won’t budge. While women are likely to experience some weight loss with a healthy diet and regular exercise routines, weight loss is usually mostly loss of non-Lipedema fat. In these instances, the stubborn, lipedema painful fat remains.

This cycle becomes a difficult one to break for those with the disorder: Yo-yo dieting leads to more weight gain. More weight gain leads to increased lipedema painful fat and disability. Increased pain and disability make it more challenging to manage mobility and secondary obesity increases. Lipedema fat also appears to be relatively resistant to bariatric surgery, meaning many women are undergoing dangerous surgeries without experiencing the intended benefit of significant loss of lipedema fat.
Unlike common obesity, Lipedema fat disorder is comprised of fat deposits and swelling that typically does not affect the feet or hands; it’s as if patients are wearing a tight bracelet or rope at their wrists or ankles that cause everything above to swell and everything below to remain unaffected. At more progressive stages, the swelling increases and leads to a diagnosis of lymphedema, which makes it even less likely Lipedema is diagnosed and treated promptly and adequately.
Despite the strong impact of Lipedema fat disorder on millions of women across the world, only limited research exists to determine its cause. In many cases, the genetic background can provide some context, but enough research has yet to offer a comprehensive understanding of the disease.
To gain more understanding of this disorder, ten medical professionals focusing on Lipedema surveyed 209 female patients in Germany. Each patient had already been diagnosed with Lipedema and undergone tumescent liposuction treatment, the only known permanent & effective treatment. Participants were recruited from patient support groups, plastic surgeons who knew their background, or from local lymphedema clinics. The survey sought to understand the patient’s journey and to evaluate what life was like before and after treatment. The full report, insights, and data can be viewed here.
Who Was Surveyed?
- All females diagnosed and treated for Lipedema fat disorder.
- All females residing in Germany.
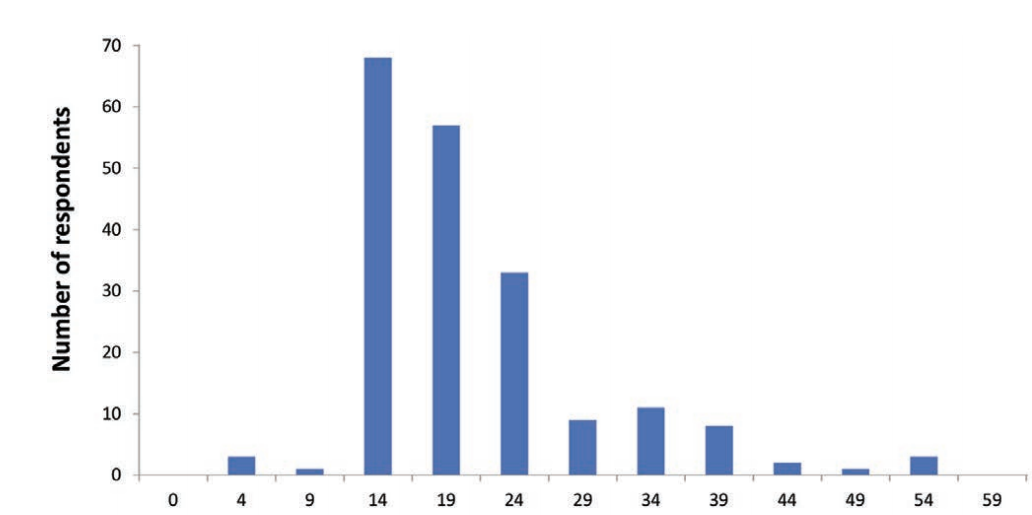
- Average age: 38 years (typically between 28 and 48 years old). The oldest participant was 68 years old, and the youngest was 20 years old.
- Tumescent liposuction was completed twelve months before completing the survey.
What Were They Trying to Find?
Survey questions were designed to determine the average age the first signs of lipedema were experienced by the patient, how long they lived with the disease before being diagnosed with Lipedema, the patient’s health background and family history that may be related to the fat disorder, and what kind of effects treatment provided.
What Does the Data Tell Us?
Early Life & Treatment for Lipedema Painful Fat Disorder
Most responses indicate patients noticed the onset of Lipedema symptoms early in life, on average, at 16 years old. Tragically, participants reported living with the disease for an average of 15 years, meaning their symptoms progressed in severity until the proper treatment could be applied. From the survey, we can also find the average number of surgeries needed was three; On the low side, patients required only one operation, and on the high side, they needed 16. The thighs, calves, buttocks, back, and abdomen were the areas treated.
Before treatment, participants reported gaining an average of 6.21 kgs (13.7 lbs) per year, without knowledge or reason for the increase in weight and body size. During surgery, on average, 10.1 liters of pure fat were removed from patients per procedure, and post-surgery the average body weight was 84.3 kg (185.8 lbs).
Family History of Fat Disorders & Other Health Issues
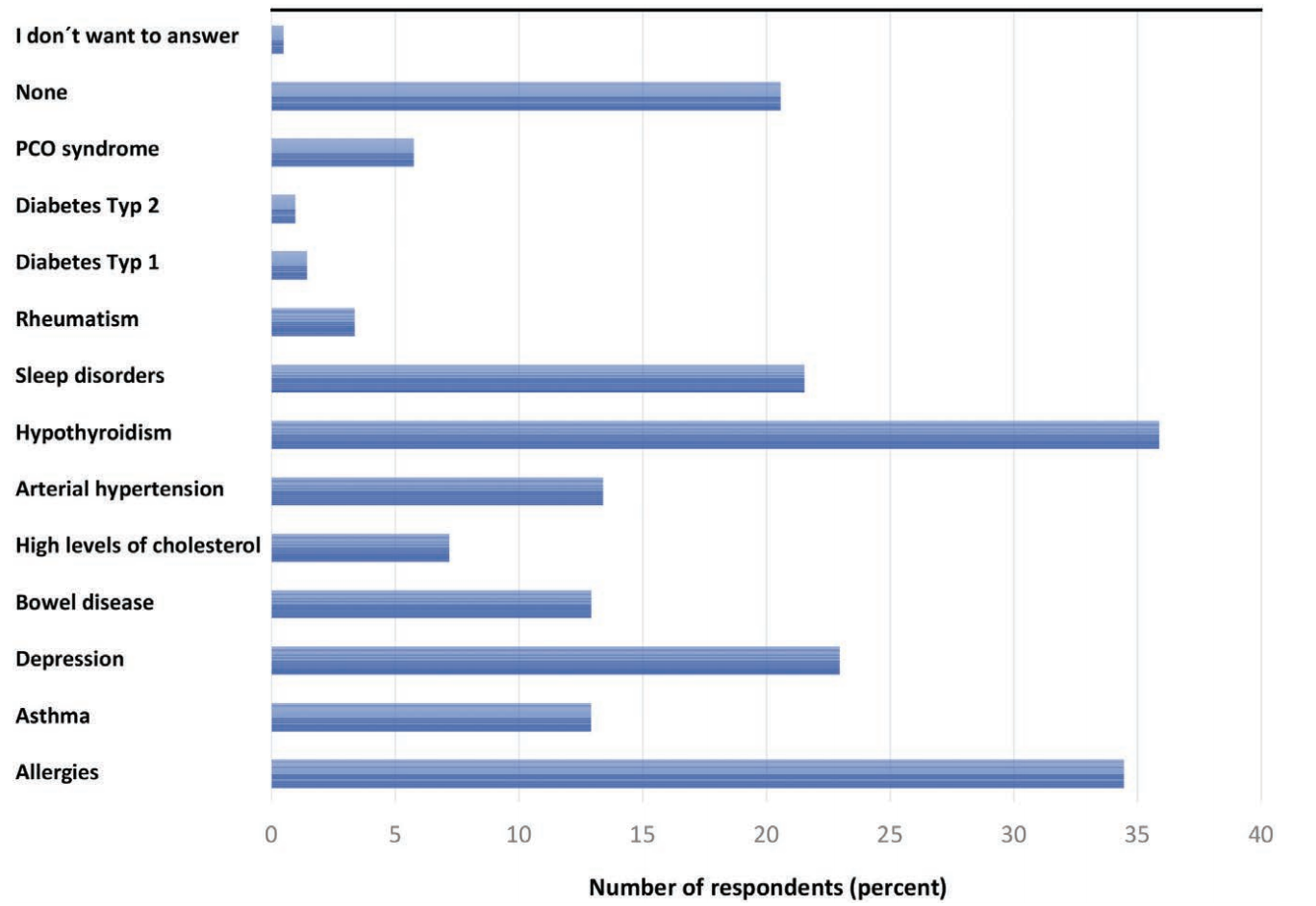
In most responses, Lipedema ran in the family. Most commonly, a patient’s grandmother or mother suffered from Lipedema, but others also had aunts, sisters, or female cousins with Lipedema. The survey also found that 166 of the 209 participants suffered from additional health issues that may or may not be related to Lipedema. For example, and most commonly reported, 36% of all participants reported suffering from hypothyroidism, a disorder where the thyroid gland does not produce enough thyroid hormone to keep the body running normally. Other commonly reported health issues include allergies (34% of all participants), depression (23%), and migraines (24%).
Other reported disorders:
- Sleep disorders (22%)
- Arterial Hypertension (13%)
- Asthma & bowel disorders (13%)
- High Cholesterol (7%)
- Polycystic Ovary Syndrome (6%)
- Rheumatism (3%)
- Type I Diabetes (1%)
Migraines
While not the most commonly reported underlying health issue, migraines offer potential insights into Lipedema treatment and link to other secondary disorders. Among the 47 participants diagnosed with migraines, 41 reported experiencing, at minimum, five migraines per month, and the remaining 6 reported suffering at least 10 per month. However, post-liposuction treatment, 40% reported a significant decrease, down to only one monthly migraine attack.
Additionally, 30% said that the intensity of the migraines had decreased, 53% stated that the frequency declined, and 21% no longer experienced them. While the link between migraines and Lipedema is unclear, this may suggest that some underlying or secondary health issues are linked to the disorder. Misdiagnoses of the secondary diseases are more likely, and further research and attention to Lipedema fat disorder is even more critical to complete.
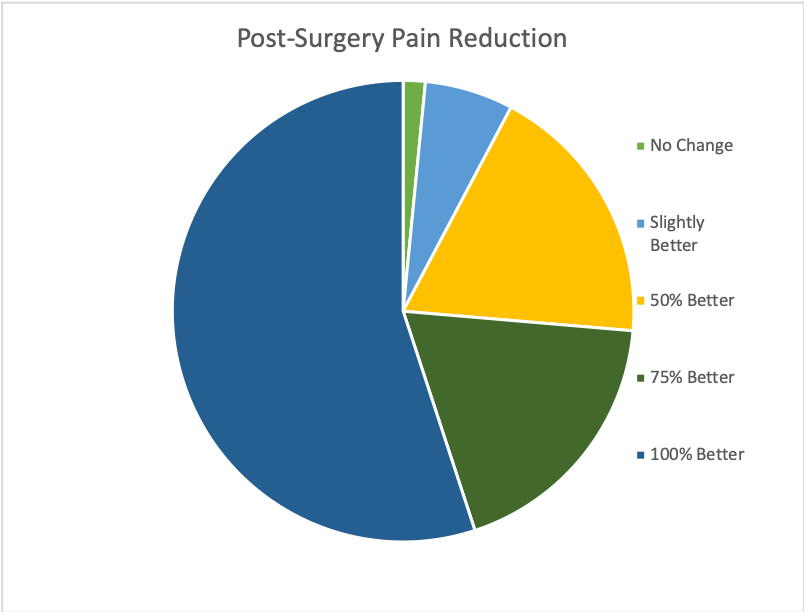
Lipedema Fat Disorder-Related Pain & Hormone Imbalances
Perhaps most importantly, the survey sought to examine what pain Lipedema patients experienced over time. More than 75% of respondents reported severe pain before surgical treatment, and only 10% reported having mild pain. After undergoing the lymph-sparing liposuction procedure, an overwhelming 97% confirmed that the pain had significantly decreased, including any tenderness or pressure previously experienced. Easy bruising and hematoma from everyday activities improved for 77% of all participants post-surgery. Out of all premenopausal patients, 31% of this subgroup reported imbalances of sexual hormones before treatment. Post-treatment and recovery, 40% said the imbalances were corrected.
Lymphatic Drainage & Patient Satisfaction
Blockages of lymph passages cause the swelling seen in both Lipedema and Lymphedema patients. To help decrease these blockages as much as possible, patients either perform manual lymph drainage on their own or regularly see a specialist. The technique for Lymphatic drainage uses light pressure and long, gentle, and rhythmic movements to increase the lymph flow and decrease blockages and swelling.
In addition to massage, compression garments are regularly prescribed to patients for the same reason – to help encourage the body’s lymphatic system to flow as necessary without blockages and swelling. However, because of the reduced swelling and removal of Lipedema fat during following liposuction, this lymphatic drainage practice may no longer be necessary.
Before surgical treatment, 81% of patients reported getting treatment through lymphatic massage at least once per week, 78% reported wearing compression garments 24 hours per day, and 20% were unable to wear compression garments because they were too painful. Post-surgery, patients seeking lymphatic drainage dropped 30%, and those wearing compression garments dropped by just over 50%. Across all patients, 98% stated they would go through surgery again and would recommend it to anyone affected by Lipedema.
What Does the Data for This Fat Disease Mean?
The majority of patients in this survey reported first experiencing symptoms during puberty, with some experiencing them for the first time as late as their early 30s. Most importantly, the data provides further support that liposuction treatment provides long-lasting and positive effects on patients, especially by decreasing their pain and increasing their quality of life long-term.
The study shows that some secondary health issues may be related to Lipedema fat disorder. For example, hypothyroidism was experienced by 35% of respondents, which is far above average. We already know that hypothyroidism patients typically have a higher body mass index, which is also typical of Lipedema patients, but further research is necessary. Migraines also were prevalent among patients but were widely decreased in occurrence and severity after Lipedema treatment. While we don’t know the exact connection, we know that migraines have many causes or triggers, including stress and depression, both of which are reported among Lipedema patients. However, after treatment, patients reported a significant decrease in symptoms. If a patient’s quality of life increases post-surgery, and their general stress and depression also subsides, it’s not surprising that their migraines would also decrease.
Additionally, 23% of respondents were diagnosed with depression, a percentage significantly higher than the average of the general population. Similar findings have determined the same correlation between obesity and depression. Not surprisingly, however, post-surgical patients experienced a decrease in depression after their weight loss and decreased long-term pain. But again, more research must be done to determine specifics.
While the report shows many links between secondary physical and mental health issues, it also shed light on what has little to no connections to Lipedema. For example, Type I and II Diabetes were underrepresented in patients. Hypertension, High Cholesterol, Dyslipidemia, Polycystic Ovary Syndrome also did not share any correlation with Lipedema patients. Interestingly, each of these is typical in obese patients, so the lack of relationship here further highlights the difference between Lipedema and general obesity.
If you asked a Lipedema patient what their journey towards surgical treatment was like, they would likely tell you that it was long and painful. Misdiagnosis and being dismissed by medical professionals when discussing the possibility of Lipedema is common. Patients often report feeling frustrated, uncertain, depressed, and helpless. Despite their best efforts, they continue to put on weight, their pain increases, and their physical mobility decreases. The data found underlines these experiences, as well as the positive outcomes after being correctly treated with lymph-sparing liposuction. The survey confirms what medical professionals have previously reported about the disorder. In essence, liposuction is the best course of action for long-lasting positive effects on the quality of life in Lipedema patients.
References: