Dr. Wright discusses the current thinking of physicians on the various stages of lipedema. He starts by defining lipedema and introducing lipedema symptoms, as well as some of the ways physicians are currently diagnosing lipedema. He then explains the different stages of lipedema and their characteristics. Finally, he ends with a few ways that physicians are attempting to treat this disease.



Overview of Lipedema Transcription
Thanks to everyone for showing up, this really is a passion of mine, helping the most amazing patients. I’m grateful for this opportunity to speak.
We’re going to go through just the basic definition of lipedema, lipedema symptoms, how lipedema is diagnosed, stages, conservative treatment options, surgical treatment options, insurance, research, and then we will have time for questions and answers.
What is lipedema? Lipedema is a chronic disease almost exclusively occurring in women. It’s characterized by bilateral symmetric excessive tissue in specific areas out in the extremities out of proportion to the rest of the body. It’s an inherited condition and it does accumulate; the fat accumulates in particular patterns out of the hip, upper and lower legs, and arms as well. So, we’ll talk about that.
Dr. Herbst’s most recent publication about four years ago showed that about 80% of ladies have the arms affected. In earlier studies, it was approximated at 20% or 30%. So, it’s still an evolving thing of how, what, where patterns and what percentage of different extremities etc.
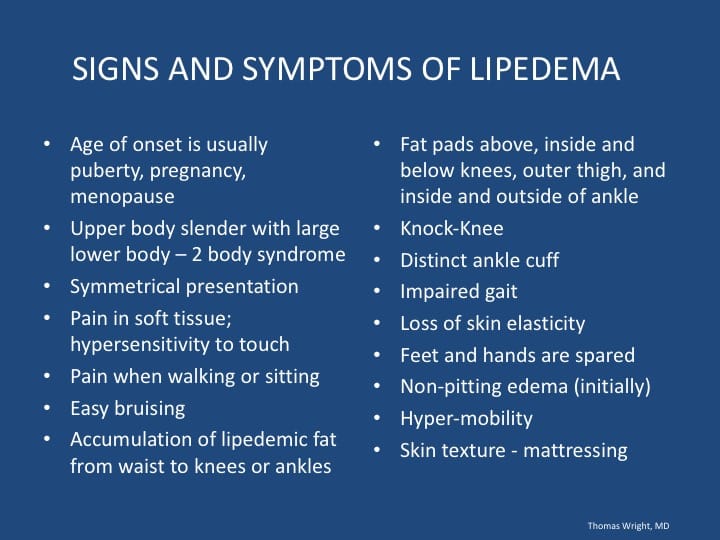
Lipedema symptoms and signs: Typically, the pattern manifests at puberty. Often the changes can in retrospect can be seen and traced back to puberty. Though it may not be present with symptoms or really declare itself until later in life, in fact the typical patient doesn’t really become very aware of it until their 30’s and may not be diagnosed until around menopause. Hopefully, as greater awareness occurs, we’ll diagnose the recognition both by physicians, nurses, and the patients themselves.
It is a two-body syndrome where the trunk is relatively smaller than the extremities, and as we mentioned earlier, it’s symmetrical. The symptoms are hypersensitivity to touch, pain, fatigue while walking and sitting, and easy bruise ability. Then, it also is associated with some orthopedic or mechanical things, such as impaired gait. There’s also a characteristic distribution of an ankle cuff, a loss in elasticity, and an edema. Now, hypermobility is not necessarily part of the diagnosis, but hypermobility is seen with increased prevalence for those who have liked the team and through the various stages the skin is affected.
[slide 4] This is just an example of some of the things I was talking about, a relatively small waist with hypertrophy in the thighs and calves, and here you see the ankle cuff. This is a classic example of a fat pad over the lateral thigh, and yet you can see this patient is actually anorectic, so it still has that hypertrophy of fat in their legs and even all the way down to the ankles. Then, in the more advanced cases, lobules of fat in the knock-kneed orthopedic derangement with still a relatively small waist. These are the different stages, so we’ll get more into that.
[slide 6] The pathophysiology is not clearly known. Lymphatics and fat are intimately connected, so lymphatic tissue only occurs or develops near fat cells, but especially the fat cells [which] mirror lymphatics are different than other fat cells. They are less resistant to diet or calorie restriction, so there is something going on with increased lymphatic flow with eventual overwhelming of the lymphatics and then leading to progressive fat growth. This is our most current theories about the pathophysiology now.
[slide 7] How is lipedema diagnosed? Well, the most important part of the diagnosis is a clinical exam, and it goes over the characteristics I went through here, with the characteristic distributions of the fat, the clinical symptoms, the family history, etcetera, and all are important for the diagnosis. But also, it’s just as important to rule out competing diagnosis, because you can actually get a phlebo-lymphedema / veno-lymphedema that looks exactly like lipedema. It can be symmetric, it can spare the feet, and with swelling in all our lymphedema disorders, there is also can be fat hypertrophy. So, it really is and sometimes it can be very hard to tease out those different things, and so it’s really critical that we rule out venous pathology as well as other lymphedema disorders when we diagnose that. The diagnosis must include a careful venous doppler looking for signs of venous insufficiency. It is on there as an example of how we detect venous insufficiency on a vast venous doppler exam, as well as how we rule out other types of lymphedema disorders. That’s a brief summary of the diagnosis of lipedema.
[slide 8] Dr. Herbst and I really believe there’s three stages of lipedema, instead of 4, because we believe that the lymphedema or swelling part of it is in all the stages. It is maybe more overtly manifested in the more advanced stages, and this goes back to the original description of it. It always involves slow swelling in the fat, and what people are often attributing to me, and where I think the confusion is, is that it doesn’t go on to swell in the hands until you’re getting actually a secondary lymphedema, but there’s always some swelling in the fat tissue, even in stage one. In that stage, the fat is smooth, and just more in its texture, it’s smooth, but it also feels swollen even in stage one. On the ultrasound, we can see even in the early stages some edema in the fatty tissue, and we can see some disruption of the fibrous tissue even before you can feel this; you could see these early signs, and that is sort of critical to our understanding, also of the pathogenesis or the cause of lipedema.
On stage 2, we see and feel nodularity, and this is described like buckshot or pebbles or that sort of thing—more poetically, pearls. That’s why I think that this is for those who you know are around me, I love to use poetic terms, because this is what I call just lusciousness, but here is where we have pearls.
Then, in stage three there are lobules that develop, and this is where these lobules are islands of fat that are in the skin that are separated by fibrous bands, and they complicate the treatment of this, because once the lobules are there, it makes it much harder to get into compression and much harder to make clothing and everything; they’re just a nightmare.
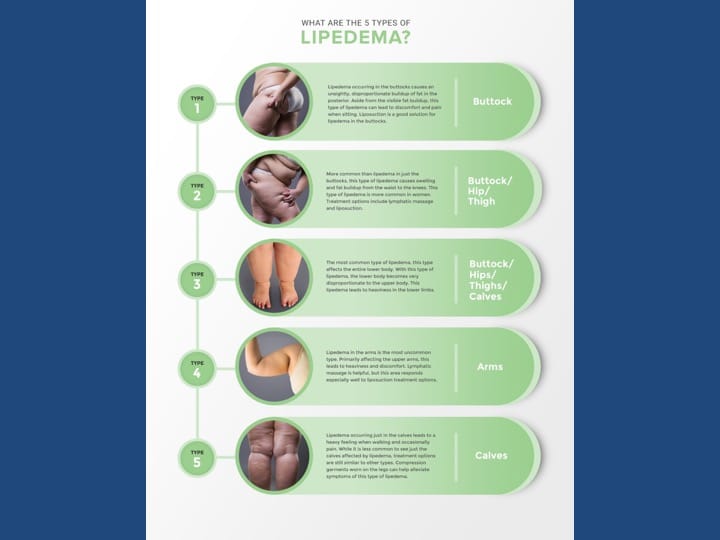
[Slide 9] Here are the 5 types of lipedema. What this is trying to show is type 1: really, the buttocks and our hips. Type 2 is the hips and thighs. Type 3 is from the ankles all the way up to the buttocks. Type 4 is in the arms, and type 5, which is the rarest type, is where it just affects the calves.
(Question: What type is the whole body?) That’s a good point, because while you guys know that comes up. Even though we’re describing where these types are where they are affecting the extremities. It does [affect the whole body]. The fact that it’s not part of the classification, because it does affect the trunk, [is that] we don’t want to make a big deal out of that, because then people will confuse it with obesity. The conservative treatment includes compression wraps and complete decongestive therapy.
Diet is very important. Let me explain about diet a little bit, because this fat is highly sensitive to insulin and carbohydrates. While it is relatively resistant to weight loss and calorie restriction, the opposite is not true; if there’s weight gain and a lot of carbohydrates and a high insulin state, it can hypertrophy and grow out of control. So, it is sensitive to diet, but it only goes one way. Exercise: water therapy and walking are two of the best exercises for this. We have the size of low-impact and aerobic exercise.
[slide 11 and 12] Liposuction is different than cosmetic liposuction, because the idea is to remove the sick fat, and it’s critical that they have decompression occur before surgery. The majority of people experience significant improvement in the clinical symptoms, pain edema, bruising, and improved quality of life after sparing liposuction, and they have reduced need for conservative treatments, but it does not cure.
