Before tackling the issues and symptoms associated with lipedema, it is important to assess your vein health by working closely with a vein specialist. Vein issues and lipedema, both can cause painful, heavy legs, and tenderness, so it can be difficult to know if your symptoms are related to veins or solely to lipedema. An experienced vein specialist can get you on the right path to a diagnosis and treatment plan.
Common Vein Issues
- Venous insufficiency causes inflammation in the veins which can contribute to lipedema swelling (edema) and inflammation. This worsens lipedema.
- Venous Insufficiency can cause progressive fibrosis (hardening of the skin) and can cause by itself lymphedema (lymphatic dysfunction, often a secondary condition paired with lymphedema called “lipolymphedema”). Having both vein problems and lipedema significantly increases your risk of lymphedema and can cause progression of lymphedema
- Varicose veins which are common and a network of small veins in the skin seen in lipedema can increase bleeding around the time of surgery in patients undergoing lipedema reduction surgery.
Understanding the limits of vein treatment in lipedema
Many women with lipedema require lifelong use of compression garments, so the advantages of treating vein issues are somewhat limited. Plus, unfortunately, edema in the legs of lipedema patients generally does not significantly improve after vein treatment. However, lipedema reduction surgery can at least temporarily treat venous insufficiency. Vein issues and issues with the lymphatic system are connected.
3 Reasons to Treat Vein Issues before Lipedema
- Cross-over in symptoms of between vein issues and lipedema.
- Vein issues stress the lymphatic system.
- Always treat varicose veins before leg liposuction to prevent complications during the liposuction procedure.


What is Lipedema?
Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. Sufferers living with lipedema experience easy bruising and tenderness, pain in the affected areas, and significant disability in daily life. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back. Little is known about the disorder, and it’s often misdiagnosed and incorrectly treated as general obesity.
What is lipedema reduction surgery?
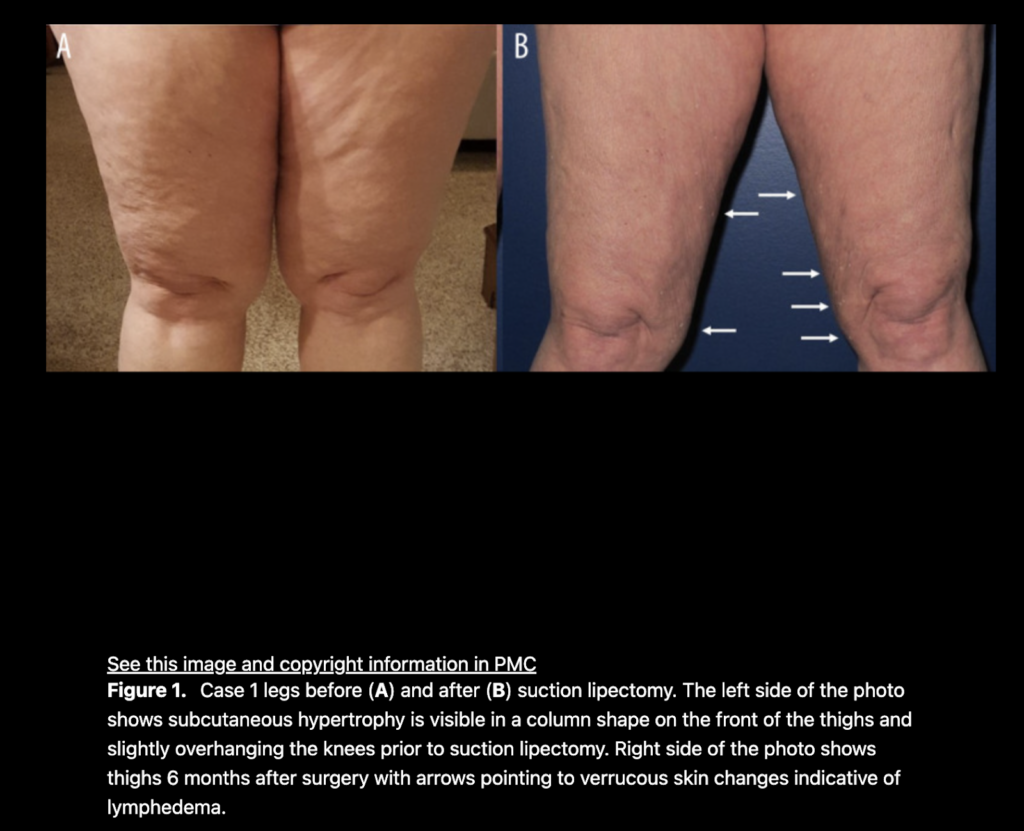
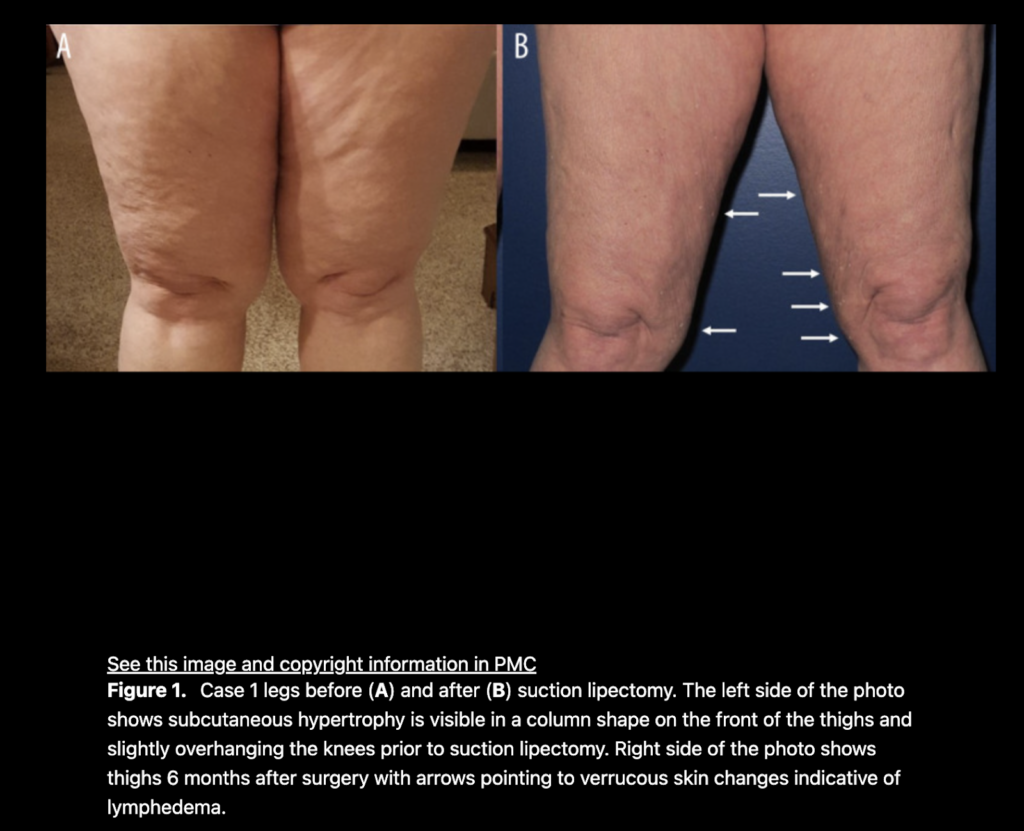
Lipedema reduction surgery is a spin-off of liposuction focused on the reduction of lipedema tissues including fibrous tissue, fat, and extracellular contents. It is possible for lymphatics to be injured by a suction cannula during lipedema reduction surgery and/or cosmetic liposuction. Some argue whether this is possible, but studies show it can, and unfortunately, may happen for some. So, it is important if you have lipedema, or suspect you may have lipedema that you get a proper diagnosis and work closely with skilled surgeons well-versed in lipedema, lymphatics and lymphedema for the best possible outcomes and treatment plan before you proceed with any type of liposuction.
According to a study by Wright and Herbst, in patients with normal lymphatic function, and no severe injury to the lymphatic collectors, the lymphatic system almost always recovers and returns to a normal state. Suction lipectomy with small blunt cannulas and surgical techniques that focus on avoiding lymphatic damage have been reported to halt lipedema progression. A modification of suction lipectomy can result in alleviating or at least improving the swelling, leg heaviness and fatigue, the need for limb compression, and the need for lymphatic massage in women with lipedema. In patients with an impaired lymphatic function such as chronic lymphedema (or lipedema), careful suction lipectomy using techniques to avoid lymphatic injury can result in improved lymphatic function and a decreased rate of secondary infection or cellulitis in the affected limbs.
Lymphatics and Lipedema
There are well-documented changes in the lymphatics of women with lipedema. The lymphatics are dilated and tortuous. Here are the differences between lipedema and lymphedema:
What are measures that may protect lymphatics?
Protective measures to lessen risk of lymphatic injury include:
- Map out the important vein and lymphatic structures
- Generous tumescent fluid (A mix of saline, Lidocaine, and a vasoconstrictor—epinephrine—which is injected before liposuction and facilitates fat removal, provides anesthesia, decreased swelling, bleeding, bruising, and improves post-op recovery)
- Longitudinal cannula technique (a wet liposuction technique that is more conservative and gentler on lymphatic injury
- Multiple positions to allow optimal orientation of the cannulas
- Small blunt cannulas versus large incisions
Effective techniques to lower the risk of lymphatic injury
The short answer is this issue is hard to study as it is not possible to examine on live patients. There is one study by Hoffman which showed a longitudinal cannula technique and tumescent solution caused less injury to the lymphatics post-mortem. There is some evidence that the preoperative mapping of venous and lymphatic structures can lower the risk of lymphatic injury. While there is clear evidence lymphatic injury can occur, there is no definitive proof of what surgical techniques can prevent lymphatic injury from liposuction or lipedema reduction surgery. Lymphatic injury complications are poorly recognized after suction lipectomy surgeries and therefore are less likely to be reported in the literature for both lymphedema and lipedema.
—
References
Crescenzi R, Marton A, Donahue PMC, Tissue sodium content is elevated in the skin and subcutaneous adipose tissue in women with lipedema: Obesity (Silver Spring), 2018; 26(2); 310-17.
Hoffmann JN, Fertmann JP, Baumeister RG, Putz R, Frick A. Tumescent and dry liposuction of lower extremities: differences in lymph vessel injury. Plast Reconstr Surg. 2004 Feb;113(2):718-24; discussion 725-6. doi: 10.1097/01.PRS.0000101506.84361.C9. PMID: 14758241.
Iker E, Mayfield CK, Gould DJ, Patel KM, Characterizing lower extremity lymphedema and lipedema with cutaneous ultrasonography and an objective computer-assisted measurement of dermal echogenicity: Lymphat Res Biol, 2019; 7(10); 525-30.
Peprah K, MacDougall D: Liposuction for the treatment of lipedema: A review of clinical effectiveness and guidelines, 2019, Ottawa (ON), Canadian Agency for Drugs and Technologies in Health.
Rasmussen 2022. Lymphatic function and anatomy in early stages of lipedema
It also well reported that higher stages of lipedema are associated with impaired lymphatic functioning. ,7–9].
The Diagnosis and Treatment of Peripheral Lymphedema: 2016 Consensus Document of the International Society of Lymphology: Lymphology, 2016; 49(4); 170-84.
Wright TF, Herbst KL. A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema. Am J Case Rep. 2022 Jul 11;23:e935016. doi: 10.12659/AJCR.935016. PMID: 35811389; PMCID: PMC9284075.\




