Getting an initial Lipedema diagnosis is a challenge for many women suffering from it. In fact, an overwhelming majority of patients seeking treatment are well into their forties, fifties, sixties, or later in age, simply because they had never heard of lipedema or been diagnosed with it. After decades of being diagnosed with a high Body Mass Index (BMI) followed by a general obesity diagnosis or misdiagnosed as lymphedema, some of these women with lipedema sought alternate explanations for their pain, discomfort, and unsuccessful weight loss, despite regular diet, exercise, and in some advanced cases even after undergoing bariatric surgery.


The Body Mass Index (BMI) calculation is an unfortunate oversimplification of a person’s health, and ignores extremely important factors that are imperative for accurate diagnosis and treatment plans. Family history and genetics, general lifestyle and activity levels, age, gender, and body composition (muscle mass, water content, bone mass) are all essential parts of our health profile, all of which are ignored by the BMI calculation. Despite all of this, it continues to be used worldwide to aid in diagnosing (or misdiagnosing and oversimplifying) patient health profiles.
Body Mass Index (BMI) = weight in pounds (or kilograms) divided by height in feet squared (or meters squared).
Body Mass Index (BMI) is simply an overall numerical score (like height and weight) which is not a biological representation of a person’s overall health. While the World Health Organization (WHO) defines a BMI over 25 as overweight and over 30 as obese, this is actually an inaccurate and incomplete assessment. Overall, obesity is a condition where fat mass affects patients metabolically, chemically, and mechanically (for example, in your joints).
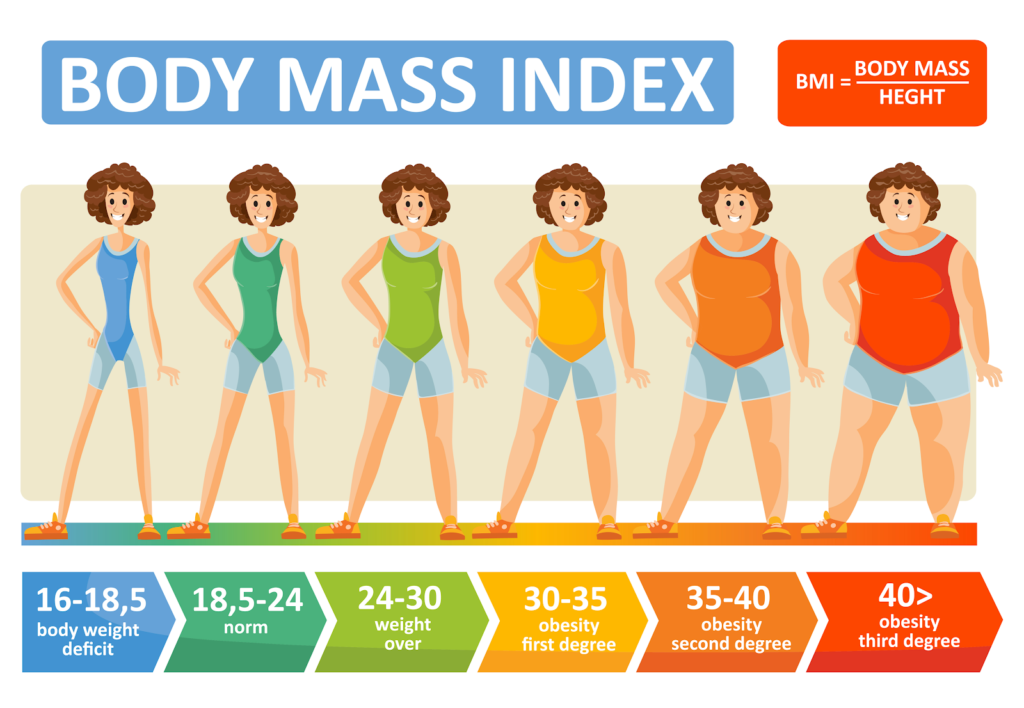
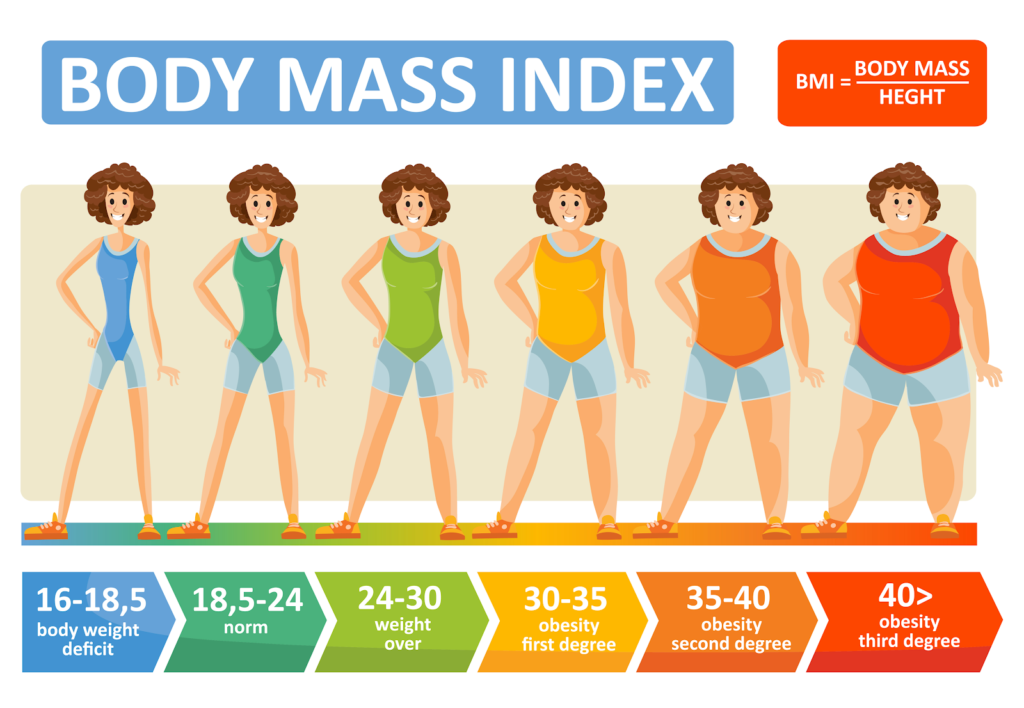
Because Body Mass Index (BMI) is a calculation that illustrations the relationship between a person’s weight and height, it equips healthcare providers with one tool in evaluating a patient’s overall health. Specifically, these ranges are used to categorize whether a person is underweight, in a normal weight range, overweight, or obese. While BMI does not provide the full picture of a patient’s health or the full body composition breakdown, it is a commonly used factor in diagnosing numerous diseases.
Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, and in many cases, excessive clustering of fat cells is noticed in the arms as well.
However, Lipedema causes fat in a different proportion on the body and has a different metabolic, chemical, and mechanical effect. Both obesity and Lipedema have increased BMIs, but they are not one and the same. When we use BMI as a blanket for Lipedema diagnosis, it’s an unfair and incomplete assessment.
Lipedema is metabolically the opposite of obesity – both are associated with excess fat accumulation, however, obesity presents with fat accumulated in the central area of the body, primarily in the abdomen, and is associated with diseases such as diabetes, high blood pressure, high cholesterol, and cardiovascular disease. However, lipedema presents with peripheral fat in the extremities, while the abdomen and/or waist are typically unaffected. But because both diseases increase a patient’s BMI, misdiagnoses are common and destructive. This illustrates one reason why BMI is not a biologically valid way to diagnose obesity or lipedema.
Interestingly, the origins of this formula were not used for individual health assessments at all! While Body Mass Index has been around since the early 19th century, the man who initially created the calculation knew at that time that it was flawed. Lambert Adolphe Jacques Quetelet, a Belgian mathematician, created the BMI formula as a way to quickly and easily estimate what percentage of the overall population might be obese. He was attempting to assist the country’s leaders in properly allocating resources in the 1830s. The formula Quetelet produced does is not biologically valid or based on any metabolic or physiologic princinciples. In other words, it is a 200-year-old hack that was never intended to describe diagnose obesity.
Simply put – where your body accumulates fat matters. This doesn’t only illustrate what you may or may not be suffering from (if anything) but also can help patients avoid misdiagnosis of more serious ailments that require more serious treatments. Ignoring fat distribution can easily lead to being either over or under-diagnosed, leaving patients with a false sense of security in their health, or in the reverse, being treated for something they don’t actually have.


For example, researches from the Medical Research Council (MRC) Epidemiology Unit in the UK concluded through a series of studies that waist size, regardless of BMI, can be a greater indicator of a person’s risk of developing type 2 diabetes. After gathering data from over 340,000 individuals from 8 European countries, Dr. Claudia Langenberg and her MRC team found that a larger waist circumference is just a likely to lead to developing Type 2 Diabetes as someone with a BMI over 30 (considered “obese”) (2). They found that non-obese males (according to their BMI) with a waist circumference of at least 40.2 inches was at just as much risk for developing Type 2 Diabetes as a male with a BMI indicating they were obese. They found the same indication in females with a waist of 34.6 inches or greater.
BMI calculations are oversimplified and do not account for the fact that bone is denser than muscle and twice as dense as fat, nor the amount of lean muscle an individual has. A person with strong bones, good muscle tone, and low fat will have a high BMI, so athletes and fit, health-conscious individuals will be classified as overweight, or even obese.
A female bodybuilder may have a higher BMI, but looking at their BMI number alone and diagnosing them as obese would be inaccurate. Similarly, while Lipedema will affect the BMI number, this BMI measure will not accurately pinpoint the cause of the higher measurement.


Additionally, fluid and water weight are not included in BMIs simply calculation, which can also lead to more serious outcomes when misdiagnosed. For example, women with Lipedema and Lymphedema will inevitably have an accumulation of fat cells, however, both these diseases are also classified by the excessive accumulation of fluid in affected areas. When missed or ignored, women suffering from these diseases are often misdiagnosed as obese rather than obtaining treatment for the source of their higher BMIs.


Perhaps one of the most obvious and frustrating blind spots of the BMI calculation is that it will be more dramatically simplified for individuals who do not fall into an “average” category for height (between 5’5” and 5’9”). For both shorter and taller individuals, their “normal” BMI ranges will shrink or widen and distort the reality of their health.
For example, a person who is 6’2” in height and weighs 230 pounds has a BMI of 29.5, putting them at the far end of the overweight category, and teetering on obese. Despite having a lean body, their doctor may tell them there are concerns about their BMI and to focus on weight loss. At their height, they would need to be at around 170 pounds to fall into a “normal” category – which for many at this height would be extremely underweight and malnourished.
On the other hand, a young child who is only 4’4 and weighs 85 pounds would also be considered overweight, despite this being a generally healthy weight. Their pediatrician may push for diet or lifestyle changes that aren’t actually needed, both worrying the parents unnecessarily and instilling an unrealistic and unfair body image in the child at a very young age.