June is Lipedema Awareness Month, a time dedicated to raising awareness, providing resources, sharing knowledge, and advocating for equitable healthcare for patients with this complicated, misunderstood, and often misdiagnosed disease. This article will explore the history of lipedema, its symptoms, stages, diagnosis, treatment options, and the importance of research and awareness campaigns. By understanding the key aspects of lipedema and its management, we can help support those affected by the condition and contribute to a more informed and inclusive healthcare system.
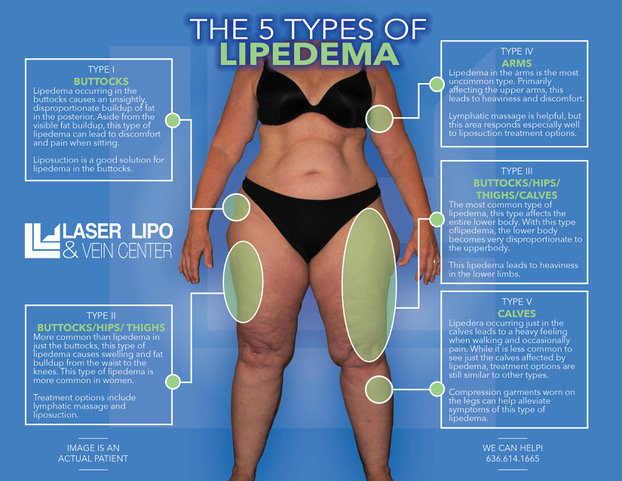
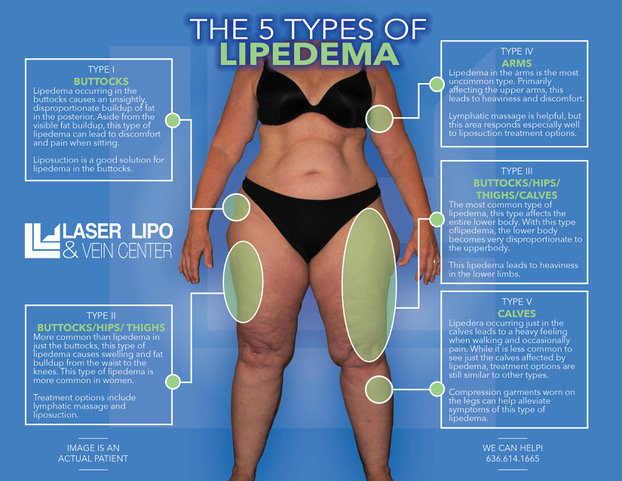
Lipedema is a fat disorder that mainly affects women and causes enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Medical professionals often misdiagnose and dismiss lipedema as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
Women suffering from Lipedema often report the disease associated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.
Lipedema is characterized by an abnormal accumulation of fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected, but the condition can also spread to the torso and arms. Symptoms of lipedema can be debilitating, and the fat cells associated with the condition are resistant to both diet and exercise programs.
Some common symptoms of lipedema include:
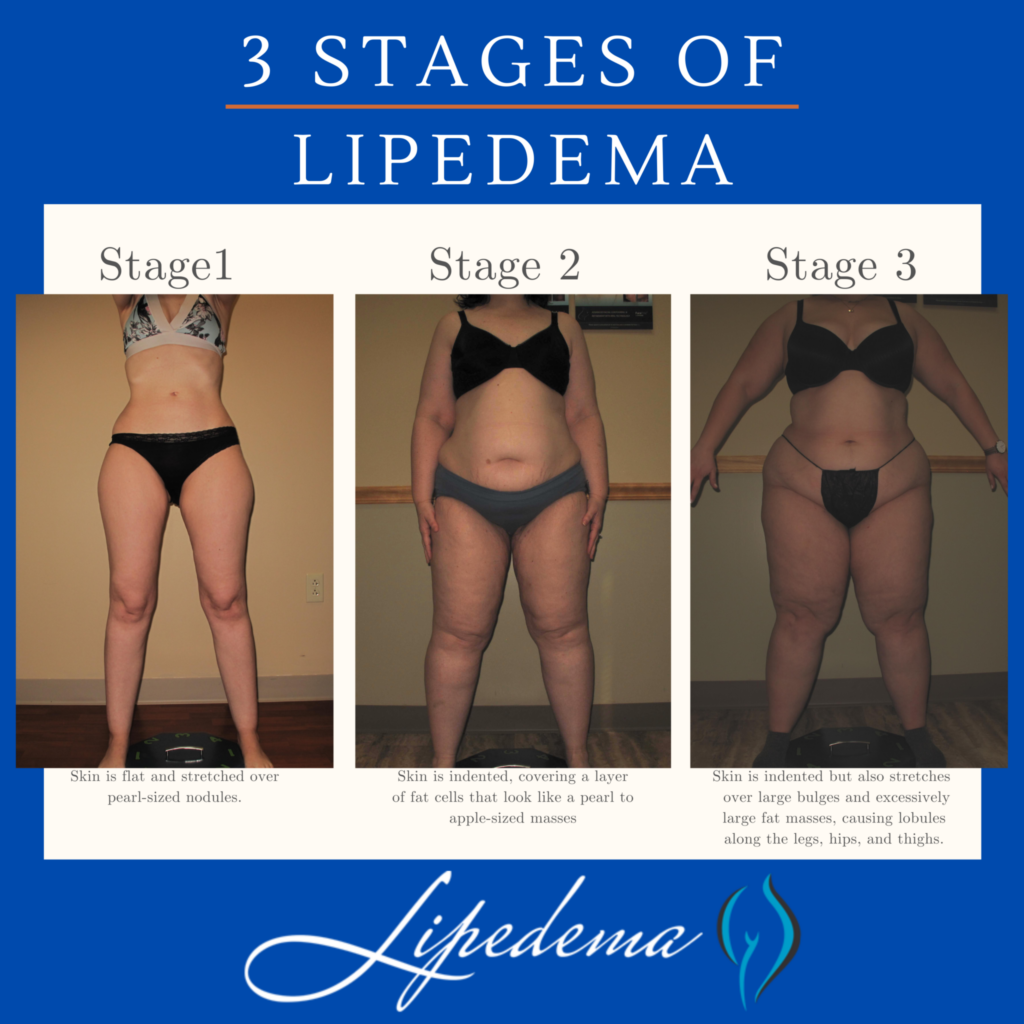
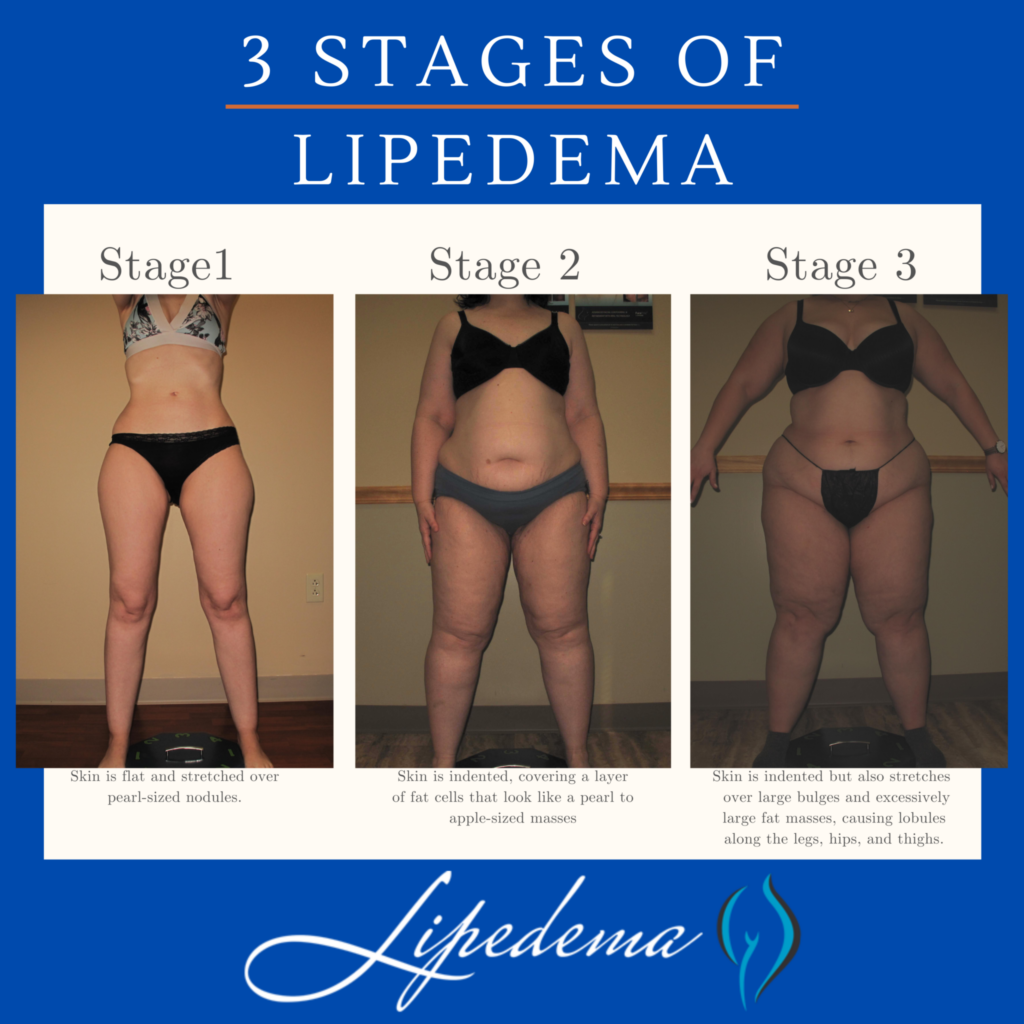
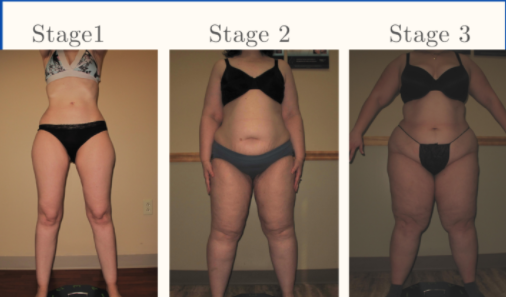
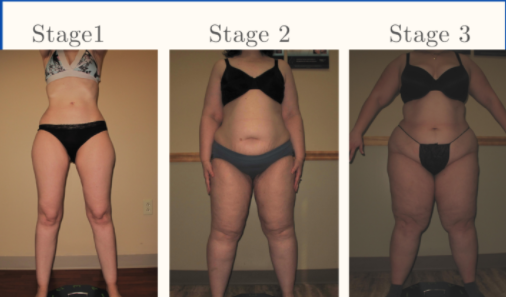
Lipedema progresses through three distinct stages, each with its own set of characteristics:
Several conditions can present similar symptoms to lipedema, making accurate diagnosis challenging. These conditions include:
Obtaining a correct lipedema diagnosis is crucial for effective treatment and management. Diagnosis typically involves a combination of a physical exam, patient questionnaires, and additional testing, such as ultrasounds or Doppler imaging. Some diagnostic tests used to differentiate lipedema from related conditions include:
While there is no definitive cure for lipedema, several treatment options can help manage the condition and improve the patient’s quality of life. These treatments may include:


Liposuction: This surgical intervention removes excess fat deposits and may provide long-term relief for some lipedema patients. However, it should be considered in consultation with a qualified healthcare professional and as part of a comprehensive treatment plan.


Despite being identified over 80 years ago, lipedema remains under-researched and poorly understood. Increased research efforts can lead to improved diagnostic techniques, better treatment options, and a deeper understanding of the condition’s underlying causes. Lipedema Awareness Month serves as an opportunity to raise awareness of the condition, educate healthcare professionals and the public, and support ongoing research initiatives.
There are several ways to participate in Lipedema Awareness Month and support patients living with the condition:
Lipedema Awareness Month is a crucial time for raising awareness, providing resources, and advocating for patients living with this often misunderstood and misdiagnosed condition. By educating ourselves and others, supporting research efforts, and promoting inclusive healthcare policies, we can contribute to a more informed and compassionate healthcare system for all those affected by lipedema.
June is Lipedema Awareness month, one in which the Lipedema community focuses (even more than usual) on how to reach women who have lived with this painful and distressing disease. While we’ve seen great strides in awareness, insurance coverage, and slightly greater recognition of this disease in the medical community, we continue to fight an uphill battle as women are underdiagnosed or completely dismissed when discussing their struggles and side effects with their providers. As a result, our team has put together some of the most important and most impactful information for all of you! Read it, re-read it, and share it with the women in your life. Some of the pain we’ve lived with for decades may actually have a life-changing solution!


Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.


Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper Lipedema diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
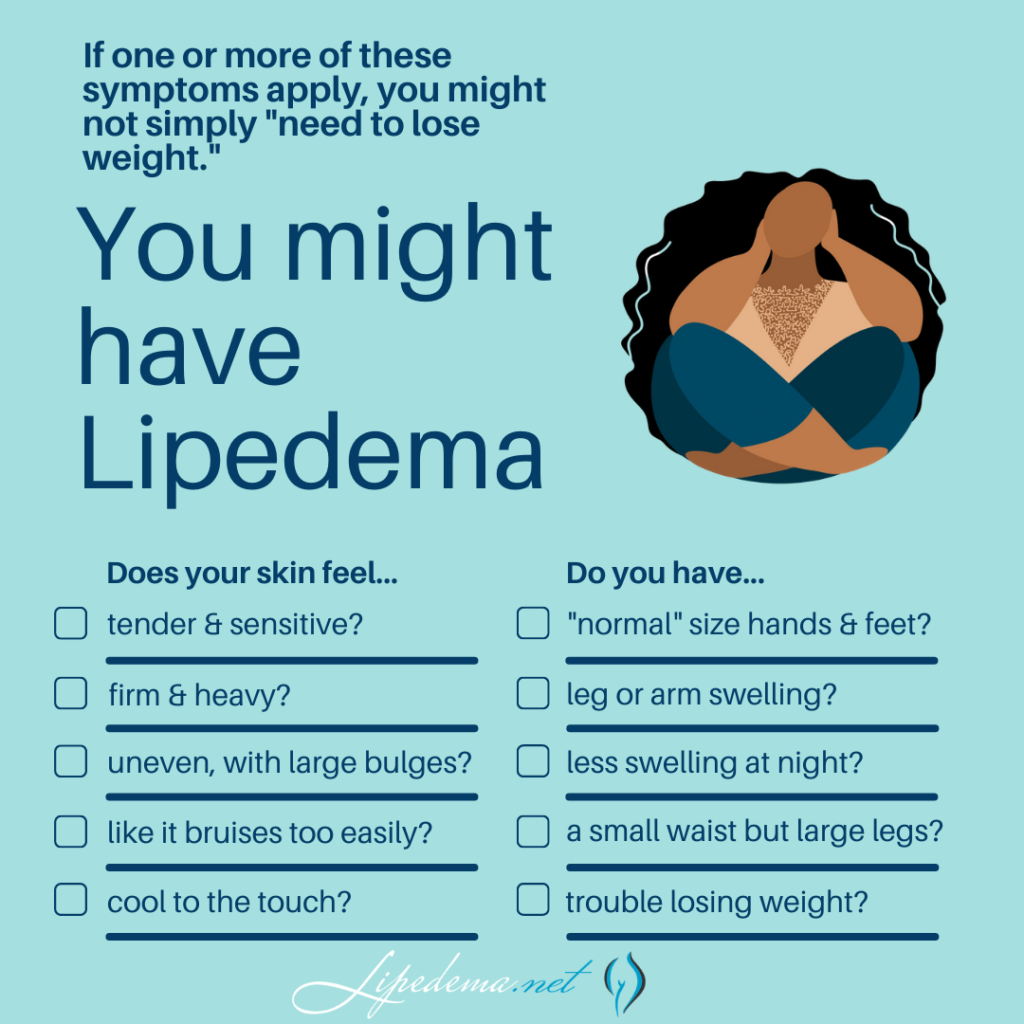
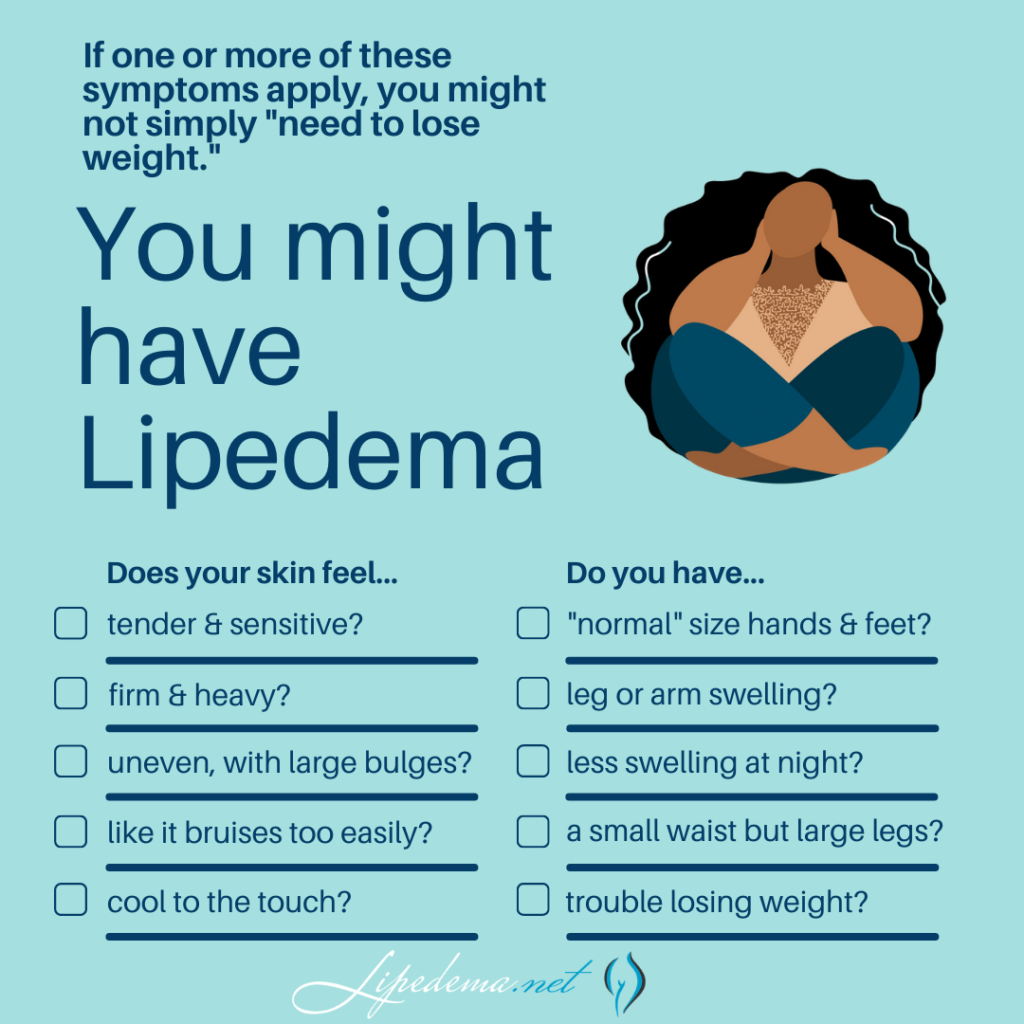
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
Overall, Lipedema appears in a series of three stages. Do any of these sounds like you?
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like a pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them. If you’re diagnosed with one of these conditions but you feel strongly that the diagnosis is incorrect, these summaries can help highlight why.
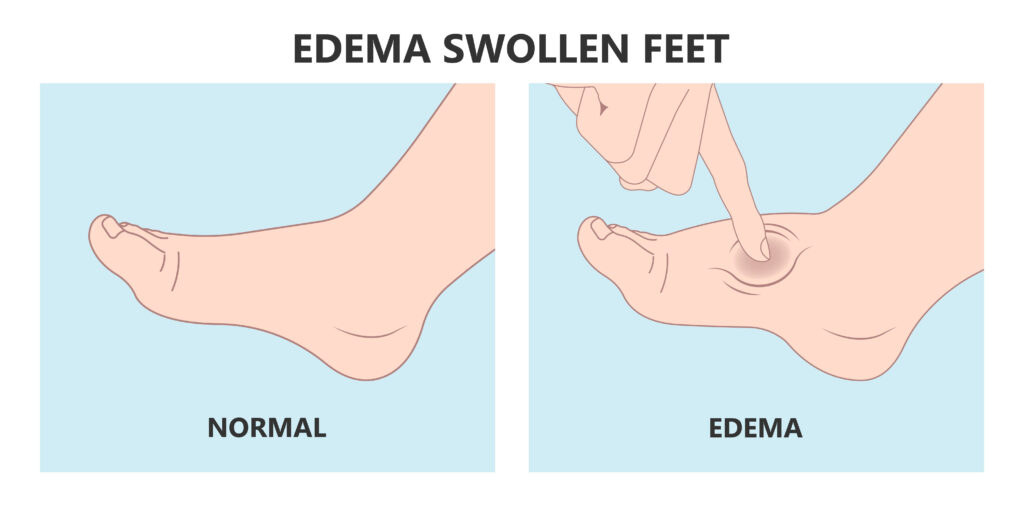
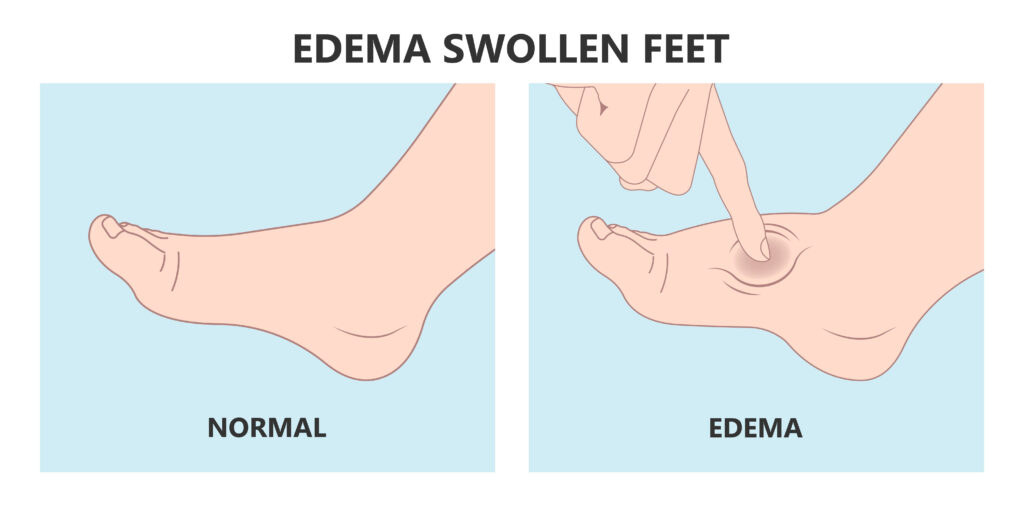
While Lipedema typically does not have to swell in the patient’s feet and hands, Lymphedema will always have swelling in these areas. Lipedema symmetrically affects both legs equally, but Lymphedema usually affects one leg or arm and leaves the other leg or arm unaffected. There may be overlap in these two diseases and treatments can be similar, but some patients only experience Lymphedema after their Lipedema progresses into later stages.
Obesity is much more common than Lipedema, and the most common misdiagnosis for it. While obesity is the accumulation of excess fat, stored centrally inside the abdomen or belly, Lipedema is the excess accumulation of fat out of proportion on the extremities, and typically not in the abdomen or belly. There may be overlap in these two conditions, too. In fact, sometimes obesity develops as a secondary condition due to the mobility problems caused by the Lipedema. So, not only is lipedema often misidentified as just obesity, but obesity can also complicate Lipedema, and be a symptom of it.
The symptoms of Lipedema and venous insufficiency are similar. They both cause heaviness, tenderness, fatigue, and swelling. They often both have discoloration in the shins, easy bruising, and prominent veins. In more advanced cases of venous insufficiency, not only does venous lymphedema develop, but a secondary Veno- Lipo- Lymphedema develops. With the overwhelmed lymph circulation, the ability to clear fatty acids from the affected tissue is compromised and a secondary fat accumulation occurs. In many cases, the best way to differentiate between lipedema and venous insufficiency and veno- lipo-lymphedema is to have a specialized standing venous Doppler ultrasound to check for venous reflux.
Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time to find a Lipedema specialist and get tested! Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema. Lipedema has many similarities to venous insufficiency (as explained above), so this can help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. Unfortunately, most hospital vascular labs complete Venous Doppler Ultrasounds with the patient lying down, While this is the typical way to find Deep Vein Thrombosis (DVT), it is definitely not a successful method to detect venous insufficiency. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
First – congratulations! We know the road to diagnosis is emotionally draining, physically painful, and it can feel lonely and discouraging. The time and research it takes to make it to this point are huge, and you should be proud of yourself and the courage it takes to be your own advocate. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.


After going through the diagnosis process and receiving a positive Lipedema diagnosis, most patients are relieved, overjoyed, and validated by their endless search. After years of living with the private struggle and knowledge that “something just isn’t right” in their body, putting a name to the issues is a huge win. And after an official diagnosis, there are many different treatment paths available to you! A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, it can give you an idea of what options may be available to you. Good luck!
Each year the country stops and takes a month to give more awareness to lipedema and those who have been diagnosed with it. June has been designated as Lipedema Awareness Month and has been observed for several years now. Take a look at what you should know about his important month each year:
When observing Lipedema Awareness Month, it is important to understand the start of lipedema itself. Lipedema was first recognized in 1940 by Mayo Clinic physicians Dr. Edgar Hines and Dr. Edgar Allen. They specifically identified the fat tissue that typically develops in the legs and occasionally arms for those diagnosed with lipedema. Even with the condition having been identified for 80 years, we still do not know everything there is to know about its cause.
Lipedema Awareness Month helps to identify lipedema for those who were not familiar with it before. Several different non-profit organizations currently offer education and research into understanding lipedema further. Become more aware of what is currently being done in this field and help those who are currently researching possible causes and cures for lipedema. One great organization to which you can donate is The Lipedema Project. You can also attend online and in-person programs to help you handle living with lipedema. Having a community behind you can make it much easier to deal with this disease.
Each year during Lipedema Awareness Month, the Fat Disorders Research Society put on their annual conference to help education those with lipedema and discuss current trends related to it. Panels are led by some of the top clinicians in the field can cover topics such as managing pain, getting emotional support, helping your lymphatic flow, and much more. Additional panels will show findings from current research into lipedema and what they mean for the future. Unfortunately, this year’s Fat Disorders Research Society Conference has been cancelled due to the ongoing COVID-19 health crisis. However, start planning today if you are interested in next year’s set of events that will be announced in the following months.
Participating in Lipedema Awareness Month is always important, but so is staying knowledgeable about lipedema at all times. Lipedema.Net along with Dr. Wright will continue to offer you everything you need to know about lipedema from research to current treatments being offered. Let us help you live easier with lipedema.
How common is lipedema? Find out here.


On the tv show The Doctors, lipedema has once again come up. This time it’s with someone who’s big behind has made her a star. This isn’t the first time I’ve run into Raylynn on the internet. I came across her picture elsewhere, where people were less kind about her body type. I went to her Instagram account and could instantly tell what she had was lipedema. It’s just so obvious with the tiny waist and flat stomach. You can see her lipedema arms getting slightly bigger now too. Anyhow, on this The Doctors segment, they have plastic surgeon Dr. Andrew Ordon do a brief exam on Raylynn and he diagnosed her with this horrible condition. I’m actually excited about this particular diagnosis because she’s an internet celebrity and this is going to make some rounds. Her fans are going to talk about this episode thus talk about lipedema. I feel we’re one step closer to the right direction.