

Have you ever wondered why some women have no issues maintaining their weight, despite your constant struggle to lose weight no matter what you do? Have you ever heard of Lipedema Legs? If you’re a woman and have noticed weight gain in your lower body that you can’t seem to control, you may have lipedema. Lipedema is a chronic and progressive medical condition that affects the limbs (and sometimes the abdomen, too!) of women. In this blog, we’ll be exploring the causes, symptoms, and treatment options for lipedema legs.
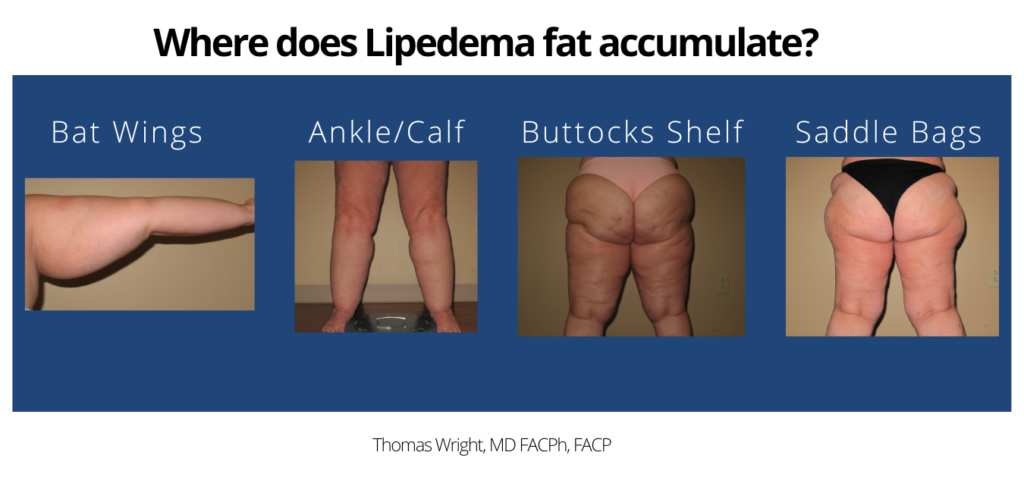
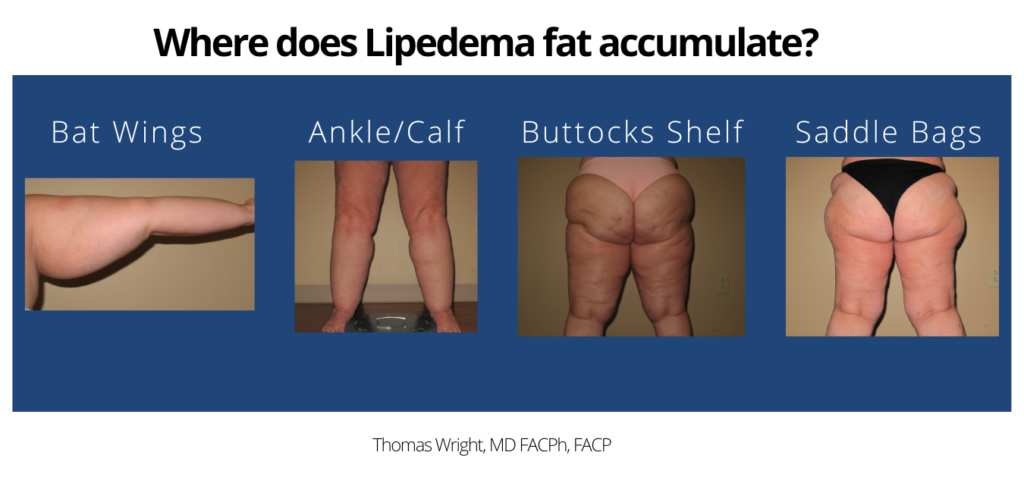
Lipedema is a medical condition that affects many women worldwide. The condition is also known as Lipoedema. It is a disorder that causes fat to accumulate in the legs, hips, buttocks, arms, and/or abdomen of many women. Fat accumulation occurs in the form of nodules and can cause pain, inflammation, and swelling. It is estimated that 11% of women in the United States suffer from lipedema, and most are unaware of their condition.
Lipedema is believed to be linked to genetics and hormones. Research suggests that hormones such as estrogen may play a role in the development of lipedema. It is also thought that lipedema has a vital hereditary component, meaning if your mother or grandmother had lipedema, you might be more likely to develop the condition. The symptoms of lipedema legs vary from person to person. The most common symptom is swollen legs, especially in the lower legs. Other symptoms include pain, tightness, and discomfort. In some cases, lipedema can cause pain, numbness, and tingling in the legs. The leg fat can also be easily bruised and is often resistant to diet and exercise.
Lipedema legs can cause a wide range of symptoms, including swelling, pain, and tightness in the legs. The leg fat can also be easily bruised and is often resistant to diet and exercise. In some cases, lipedema can cause numbness and itchiness or tingle in the legs. In addition, leg fat can cause an uneven weight distribution, resulting in pain and discomfort.
The symptoms of lipedema can vary from person to person. Some people may experience little to no symptoms, while others may experience more severe symptoms. The severity of the symptoms can also vary over time.
The diagnosis of lipedema legs is based on a physical examination and a review of the patient’s medical history. The doctor will look for signs of fat accumulation in the legs, hips, and buttocks. They may also check for signs of inflammation and swelling. The doctor may also perform a lipedema test, which involves measuring the circumference of the legs, hips, and buttocks. This test can help determine if the patient has an accumulation of fat in the affected areas. In addition, the doctor may perform a stemmer sign test.
The stemmer sign is a test used to diagnose lipedema. The test involves pressing the thumb against the skin of the affected area. If the skin does not indent, this is a sign of lipedema. This test is used to differentiate between lipedema and other causes of swollen legs, such as lymphedema. The stemmer sign test can also help determine the severity of the lipedema. In mild cases, the skin may indent slightly, while in more severe cases, the skin may not indent at all. This can help the doctor determine the best course of treatment for the patient.
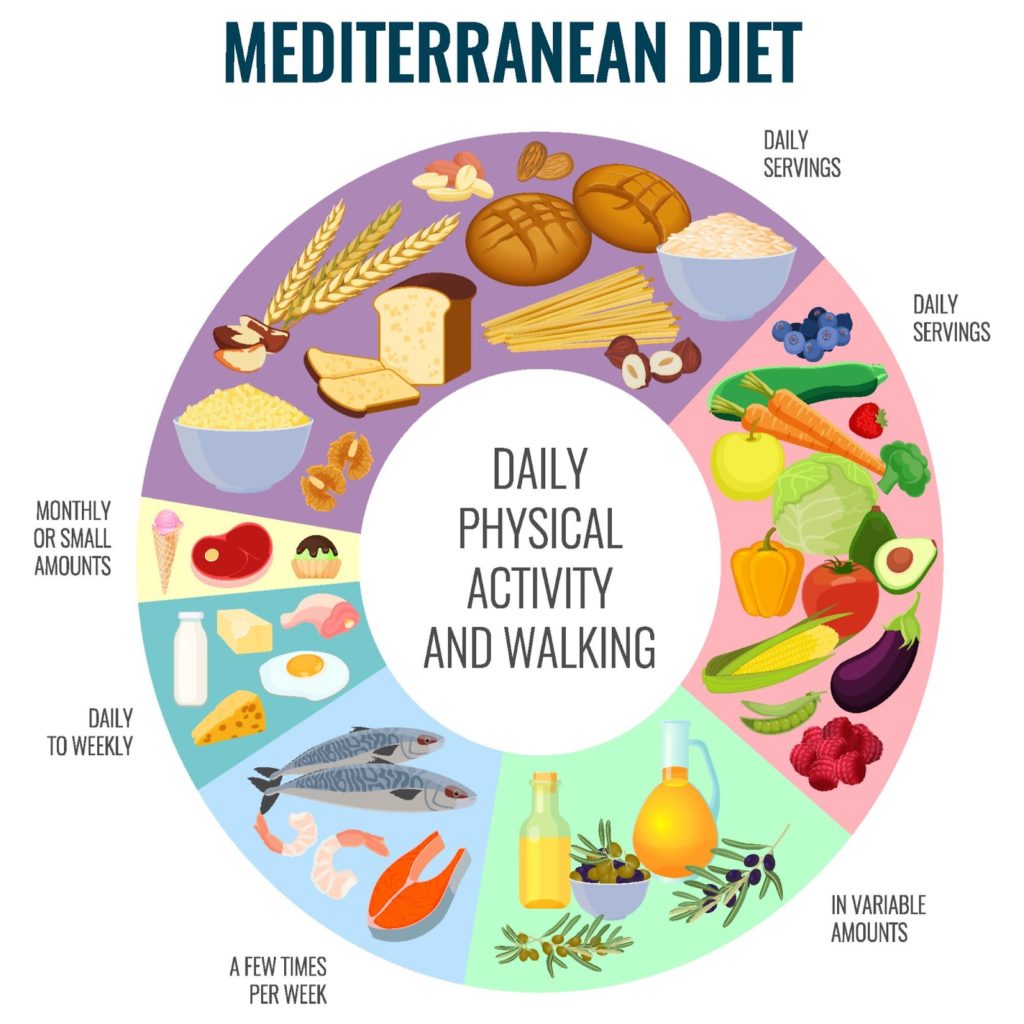
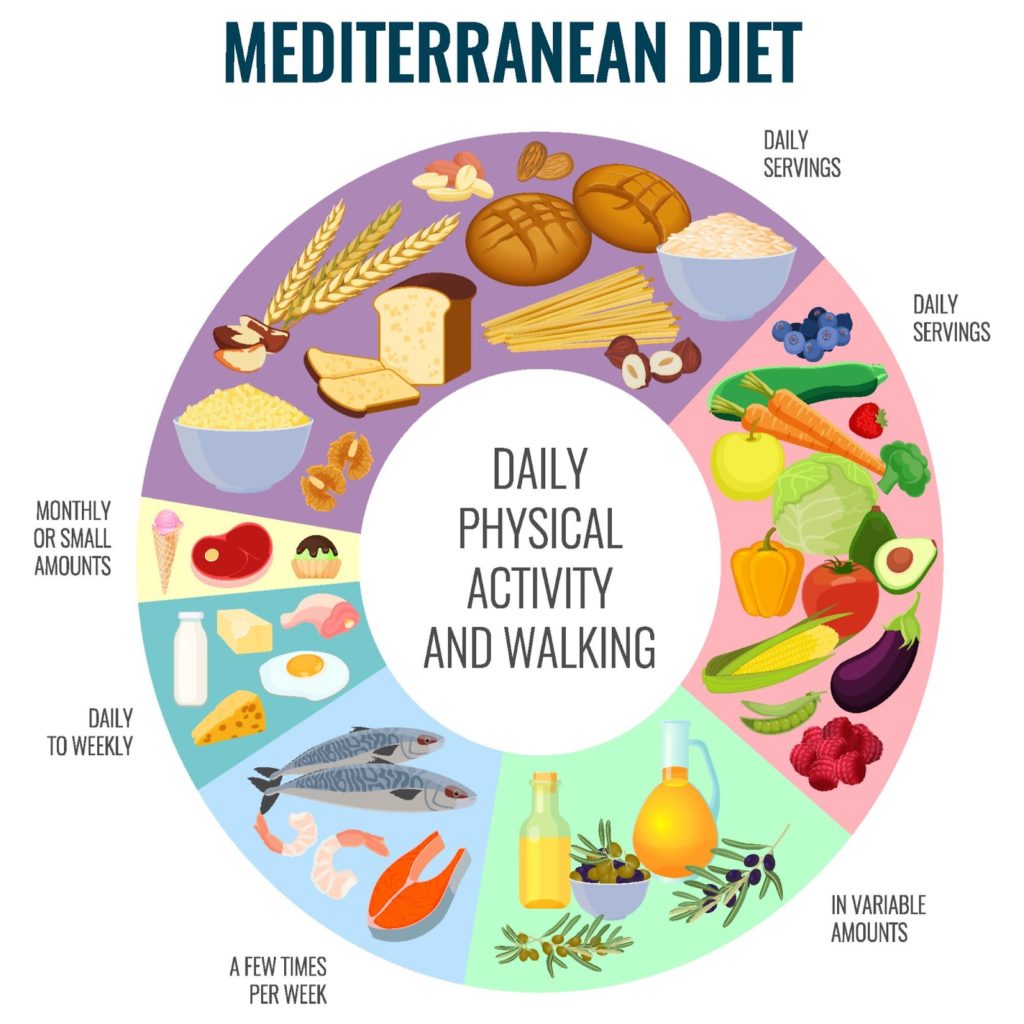
Once the diagnosis of lipedema legs has been made, the doctor will recommend a treatment plan. The treatment plan will vary depending on the severity of the condition. In mild cases, the doctor may recommend lifestyle changes such as diet and exercise focused on decreasing inflammation triggers. Medical-grade compression help reduce the inflammation is lipedema tissue in the legs. In more severe cases, the doctor may recommend medication or surgery. Medication and surgery are typically used to reduce the swelling and inflammation associated with lipedema. Medication can help reduce the number of fat cells in the affected area and can also help reduce swelling and inflammation. Surgery can help remove fat cells from the affected area and can also help reduce swelling and inflammation.
If you think you may have lipedema, you must see a doctor. The doctor will perform a physical examination and review your medical history. They may also perform a lipedema test and a stemmer sign test. Once the diagnosis has been made, the doctor will recommend a treatment plan. Treatment may include lifestyle changes, medication, and surgery.
Lipedema legs can be a difficult condition to live with, but with the right treatment, it is possible to manage the disease. With the right treatment, you can live a healthier and more active life.


One of Dr. Wright’s newer patients, Crystal, was diagnosed with Lipedema for the first time just 3 months ago, and she’s already feeling the joy and relief that comes with an official Lipedema diagnosis.
“I felt a sense of relief and joy come over me instantly,” she says.
Crystal was diagnosed by Dr. Wright with Stage 3, Type 3, and 4 Lipo-Lymphedema. Over the next 90 days post-diagnosis, she’s undergone two Lipedema surgeries and overcome a lifetime of challenges when it came to “her relationship with gravity”, as she calls it. She lost just over 70 pounds after the two surgeries and is relieved to be on a path of healing.


Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Nearly 17 million women in the U.S. and nearly 370 million women across the globe suffer from Lipedema. What is regularly associated with unruly weight gain in its initial stages can quickly spiral out of control if left undiagnosed. Often striking in a woman’s mid-20s, Lipedema is a disease that leads to the excessive buildup of fat cells primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often present with pockets of fat on the limbs that appear disproportionate in comparison to the rest of the body.
Women suffering from this disease often report the association with lipedema pain symptoms that trigger difficulties dealing with everyday life activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provokes vascular and lymphatic swelling which can lead to further medical complications.
Lipedema is often misdiagnosed as standard obesity, leaving patients to deal with an endless cycle of disappointment and ongoing, painful lipedema symptoms. As they continue, their weight refuses to fall off. Unfortunately, Lipedema does not respond to a simple calorie restriction or increased exercise and ultimately requires surgical intervention in order to alleviate the appearance and pain of symptoms.
Patients often report that the road to their initial Lipedema diagnosis is an uphill battle. Women with Lipedema are typically diagnosed by their primary care provider with traditional obesity, and all treatment methods follow this diagnosis.
Unfortunately, as any Lipedema specialist will tell you, this treatment proves ineffective, and leaves women with Lipedema without answers, without a solution, and with continued pain and continued frustration as their, Lipedema continues to progress. Liposuction performed on the affected limbs is one of the most effective forms of treatment. Removing fat deposits that are diseased not only helps reduce swelling of the limbs but alleviates the pain that holds patients back from everyday activities. But before women with Lipedema and even consider these procedures and treatment options, they must first find a doctor who is an expert in this field and start with a proper diagnosis of the disease.
Just like Crystal, many women search for answers for years before getting an official diagnosis and validation for their struggles. “My body really needed this healing,” Crystal says. “I needed answers and I was craving [an] explanation why my body was fighting me.” While she contributes 15 pounds lost directly to her surgeries, she says she’s done the non-surgical work to get rid of additional lipedema swelling and fluid alongside surgery. She says she monitors what she eats and when, and eliminated a few types of foods that directly increase swelling, helping her lose more than 50 pounds on her own, and improving the outcomes of both her surgeries tenfold.
She encourages other women who think they may have Lipedema to contact Dr. Wright and his team to get the same help she’s received. “If you have lipedema or lipo lymphedema like I do, go easy on yourself,” she says. “There isn’t anything you could have done to prevent it, but I’m living proof there are things you can do to live better and have a higher quality of life.”
Good news, these conditions are not life-threatening on their own. However, if undiagnosed or untreated, they will worsen over time and may contribute to several other secondary ailments and complications. If you have signs of swelling, and pain in your body, especially in your legs and arms, seek treatment starting with your primary care physician. Ongoing care of lipedema and lymphedema with a vascular expert lessens the risk of other serious problems.
For instance:
Remember, you are in control of how you manage your health and well-being. Educate yourself and do not hesitate tol ask for help. A great resource for emotional support from the comfort of your home is https://www.mind-diagnostics.org. A study by researchers at the University of California, Berkeley found online counseling can be just as effective as face-to-face therapy while being more convenient, affordable, and accessible.
Sources:
https://www.healthgrades.com/right-care/symptoms-and-conditions/lymphedema
https://my.clevelandclinic.org/health/diseases/8353-lymphedema
https://www.nhs.uk/conditions/postural-tachycardia-
syndrome/#:~:text=Postural%20tachycardia%20syndrome%20(PoTS)%20is,as%20postural%20orthostati
c%20tachycardia%20syndrome
https://www.aapmr.org/about-physiatry/conditions-treatments/pain-neuromuscular-medicine-
rehabilitation/degenerative-joint-disease
https://www.nhs.uk/mental-health/conditions/body-
dysmorphia/#:~:text=Body%20dysmorphic%20disorder%20(BDD)%2C,affects%20both%20men%20and%
20women.
https://www.betterhelp.com/study/Study_of_BetterHelp_eCounseling.pdf
3 independent studies find lipedema is an inherited condition.
As reported by The Cleveland Clinic [#} on its website, the exact cause of lipedema is unknown, but the condition runs in families and may be inherited. This statement is supported by three independent studies conducted by leading research teams in Europe who validated lipedema is a genetic condition. Lipedema appears to primarily affect females, presumably driven by estrogen as it usually manifests at puberty. Lipedema disease is different from obesity and is often misdiagnosed as primary obesity because these conditions commonly overlap.
Researchers hope to continue to study as many families as possible with multiple cases of lipedema to create a stronger genetic linkage and determine the biochemical makeup of this disorder. Having this data may help researchers identify the gene that causes lipedema to increase understanding and improve treatment for this painful condition.
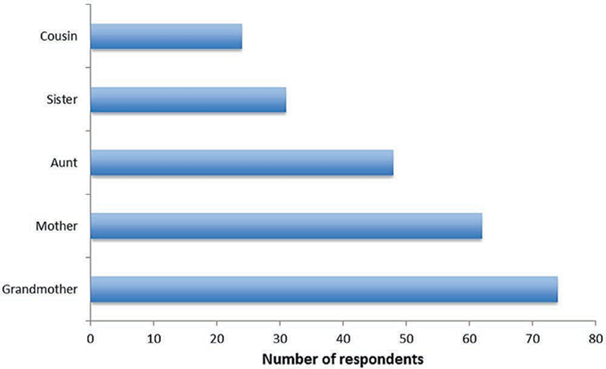
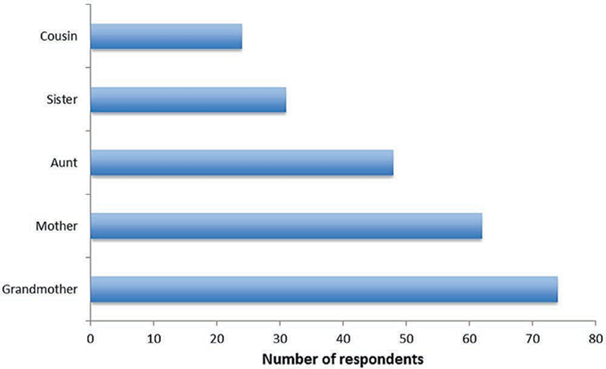
Fig 1. Bauer and etal. study reaffirms relatives of lipedema patients also suffer with lipedema. In most cases, grandmothers and mothers were affected the most, followed by aunts, sisters, and cousins.
The familial nature of the condition suggests that lipedema can demonstrate heritability[1]. The exact nature of the form of inheritance is difficult to determine.
Of lipedema patients who participated in a study, 73% reported they had one or suspected multiple family members also had lipedema. Most frequently affected was the mother (38%), followed by grandmother (17%), aunt (8%), sister (6%) and cousin (5%).


A study from 2010 showed that within six families of more than three generations with lipedema disease, a genetic autosomal-dominant hereditary pattern [2]was found.
Frequent studies of mother-to-daughter mode of inheritance led researchers to theorize lipedema is a genetic disorder.


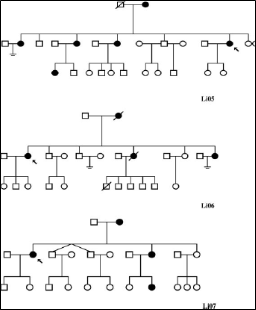
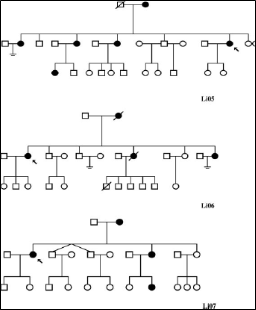
Fig 2. The largest family pedigrees (with a minimum of three living affected members in at least two generations) are demonstrated in Figure 2.
Family clusters of lipedema where more than one family member has the condition indicates a genetic component with a possibly X-chromosome[3] dominance inheritance pattern.
All affected family members were female first- or second-degree relatives of female patients.
One family had six living affected members in three generations, two families had five affected members, two had four affected members, and one further family had three living affected members.
As lipedema appears to be most common at puberty, it is reasonable to assume that hormonal influence underlies the marked female limitation shown in studies to date.
Estrogen is also considered to play a key role in regulating the manner of development of the condition.
—
Study participants:
Between all three studies, women ages 16-83 (average age, late 30s)
Do you suspect you or a loved one may have lipedema? We can confirm your condition and start you on your journey to feeling better. Contact us to schedule an appointment, today.
References
Bauer AT, et al. Plast Reconstr Surg. 2019 Dec;144(6):1475-1484 https://pubmed.ncbi.nlm.nih.gov/31764671/
Ghods M, Georgiou I, Schmidt J, Kruppa P. Disease progression and comorbidities in lipedema patients: A 10-year retrospective analysis. Dermatologic Therapy. 2020;e14534. https://doi.org/10.1111/dtch.14534
Child AH, Gordon KD, Sharpe P, Brice G, Ostergaard P, Jeffery S, Mortimer PS. 2010. Lipedema: An inherited condition. Am J Med Genet Part A 152A:970–976. https://pubmed.ncbi.nlm.nih.gov/20358611/ and https://www.researchgate.net/publication/346917917_Disease_progression_and_comorbidities_in_lipedema_patients_A_10-year_retrospective_analysis/figures
# Cleveland Clinic Lipedema https://my.clevelandclinic.org/health/diseases/17175-lipedema
[1] Heritability is a measure of how well differences in people’s genes account for differences in their traits
[2] Autosomal dominant inheritance is a way a genetic trait or condition can be passed down from parent to child.
[3] The X chromosome is one of two sex chromosomes. Humans have two sex chromosomes, the X and Y. Females have two X chromosomes in their cells, while males have X and Y chromosomes in their cells.
When dealing with the effects of lipedema, your body can also feel the repercussions of direct impact on your lymphatic and venous circulation system. Both systems together help the body create lymph. Venous disorders like venous hypertension and venous reflux impact these combined systems to create excess lymph production. Having an overwhelmed production can lead to overloaded lymphatic circulation. Both the venous system and our lymphatic circulation utilize passive contractions to clear this fluid from our limbs.
As a result, our team has put together some of the most important and most impactful information about Lipedema, how it can affect your veins, and how to get a proper diagnosis. Read it, re-read it, and share it with the women in your life. Some of the pain we’ve lived with for decades may actually have a life-changing solution!


Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.
Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
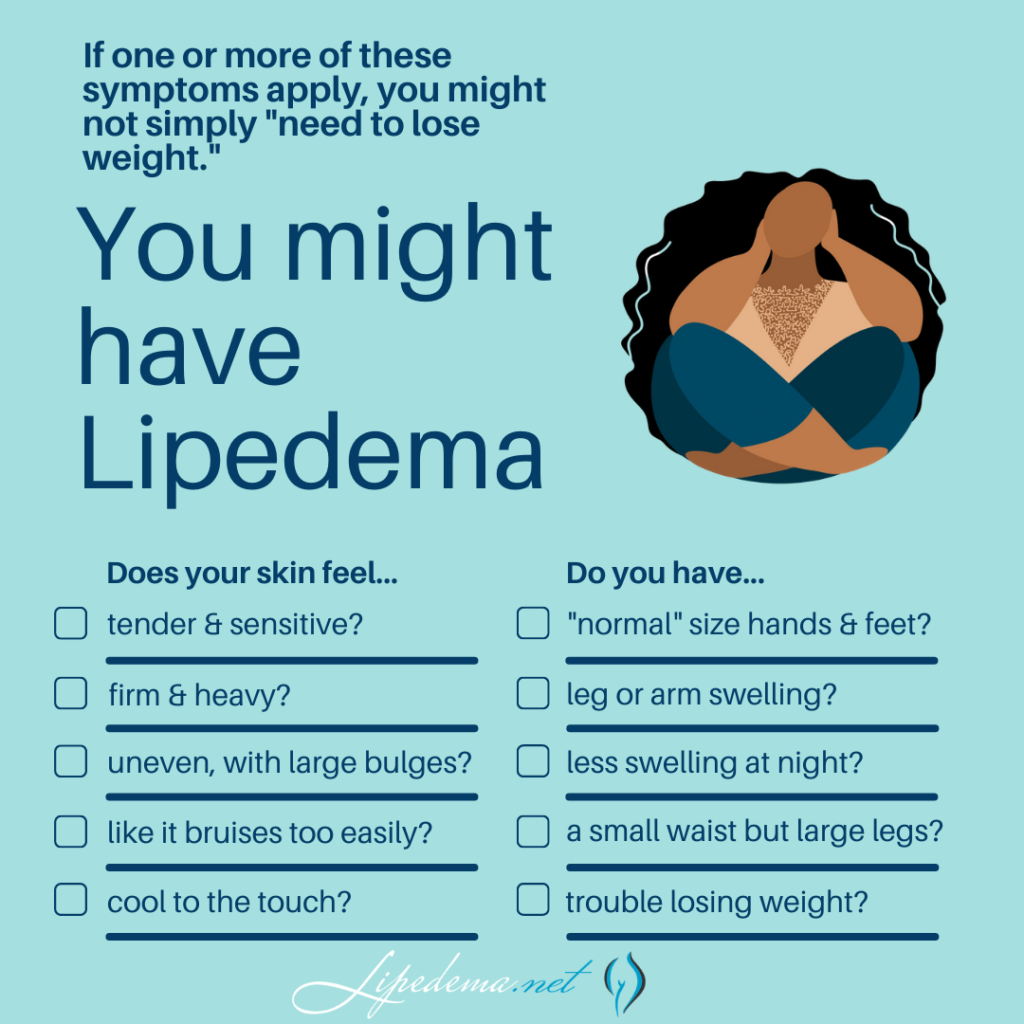
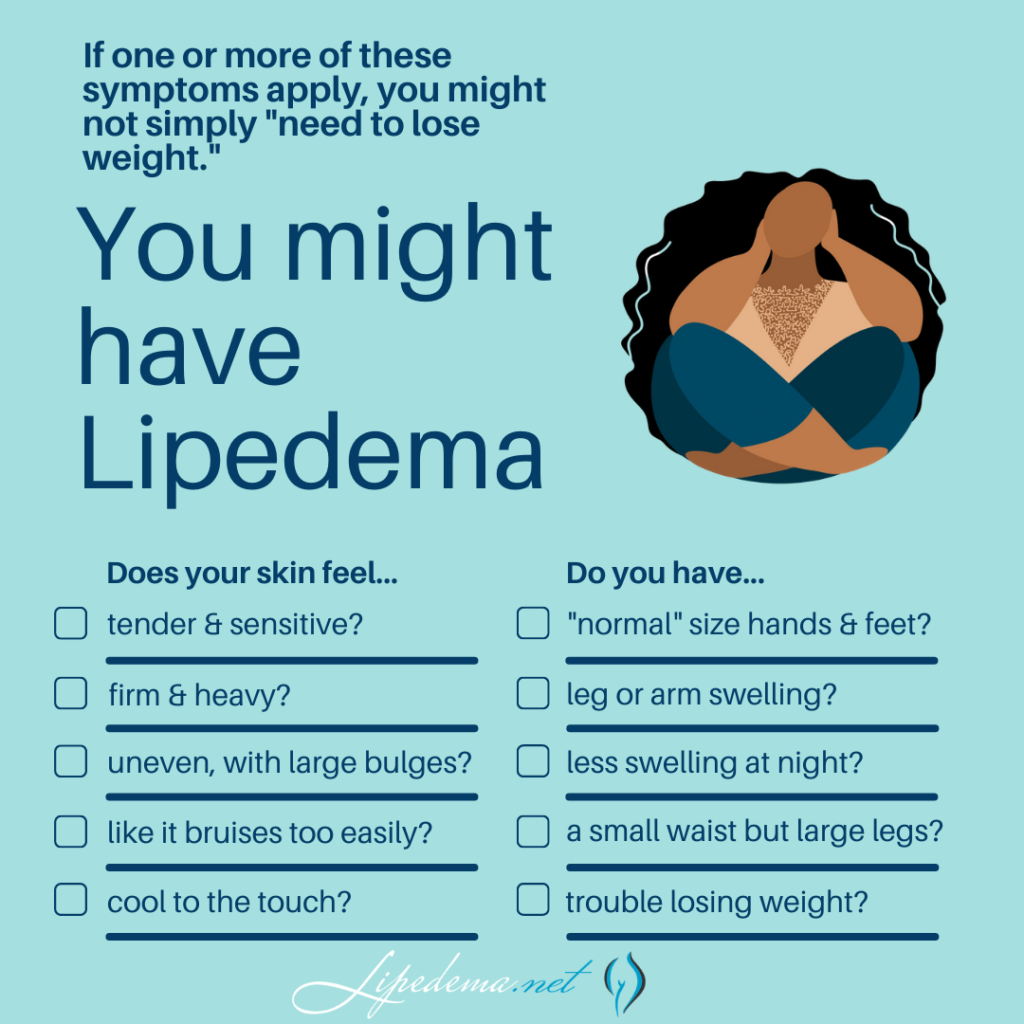
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
Lipedema Symptoms Checklist:
☑Tender skin that is sensitive to the touch, feels pressure when walking or climbing stairs, crossing your legs, or sitting for long periods of time.
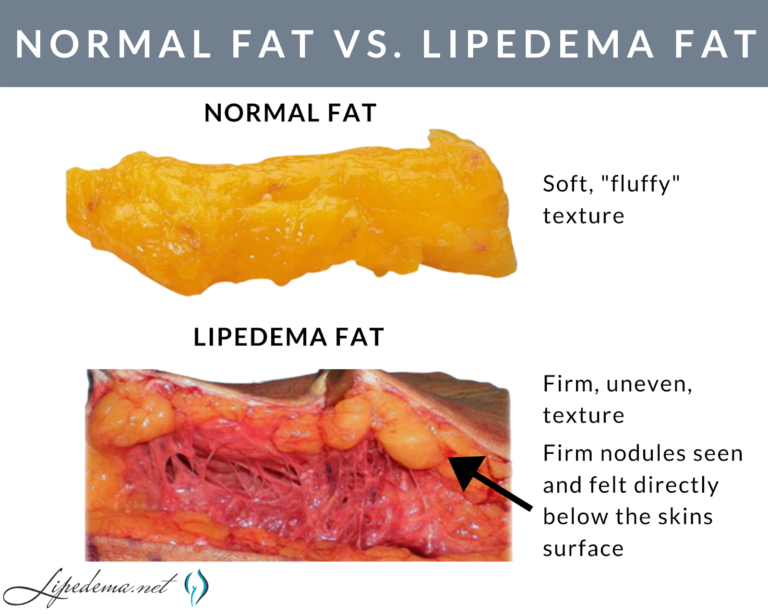
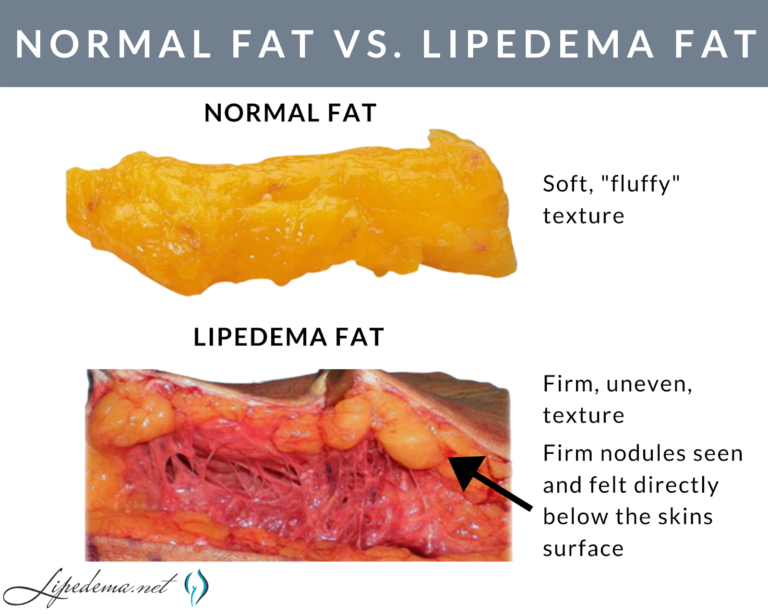
☑Skin’s surface feels nodular and firm, like beans in a bean bag or rubber balls.
☑Skin’s surface is uneven, with large bulges and valleys up and down. Areas that were traditionally thought of as cellulite are much more dramatic and bulging.
☑Skin’s temperature is relatively cool.
☑Legs feel heavy and tired.
☑Swelling in the affected area (legs, arms), worsening during the day, and better at night after you’re able to elevate your limbs (such as laying in bed).
☑Easy bruising.
☑Visible veins.
☑Disproportionate fat accumulation, not affected by calorie restriction. Think extreme “pear-shaped” body.
☑Feet and hands are unaffected by weight gain or swelling. As a result, there’s often a “cuff” at the ankles or wrists.
Our lymphatic system has several key jobs to help our body function properly. First, it drains our body cells of any debris that needs to be removed. It also drains any excess fluid our tissues have built up. The lymphatic system also transports any clean fluid back to our blood that needs it. With such an important job for our body, it is critical to understand how lipedema can cause additional lymphatic issues. Individuals with lipedema will notice that their lymph fluids are not properly draining, causing a buildup in the legs. This fluid building can be painful and cause additional swelling.


Our venous system is made up of deep venous pumps and veins located throughout the legs. These pumps when properly working pump 90% of the blood from the legs. The other 10% of the blood is pumped through a superficial venous system. While this system is typically less important than the deep venous pumps, they are at more risk when lipedema is involved. Blood flow may reverse and flow in the opposite direction; healthy vein valves ensure our blood is flowing in one direction for a healthy system.
The symptoms of Lipedema and venous insufficiency are similar. They both cause heaviness, tenderness, fatigue, and swelling. They often both have discoloration in the shins, easy bruising, and prominent veins. In more advanced cases of venous insufficiency, not only does venous lymphedema develop, but a secondary Veno- Lipo- Lymphedema develops. With the overwhelmed lymph circulation, the ability to clear fatty acids from the affected tissue is compromised and a secondary fat accumulation occurs. In many cases, the best way to differentiate between lipedema and venous insufficiency and veno- lipo-lymphedema is to have a specialized standing venous Doppler ultrasound to check for venous reflux.


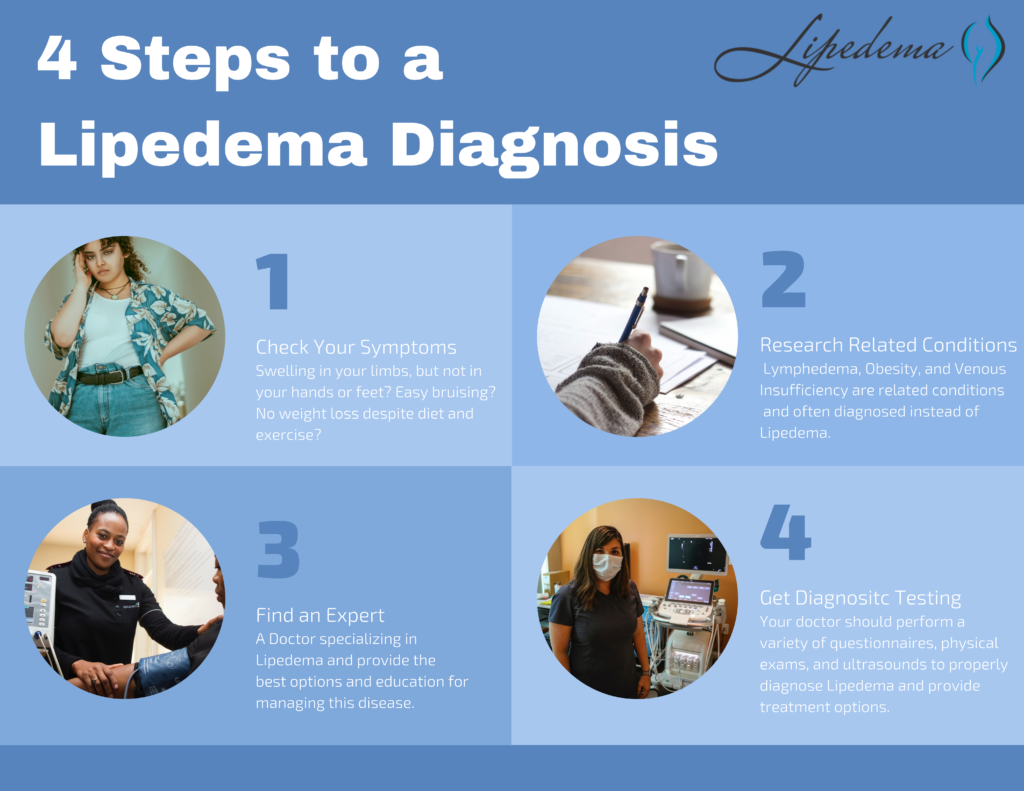
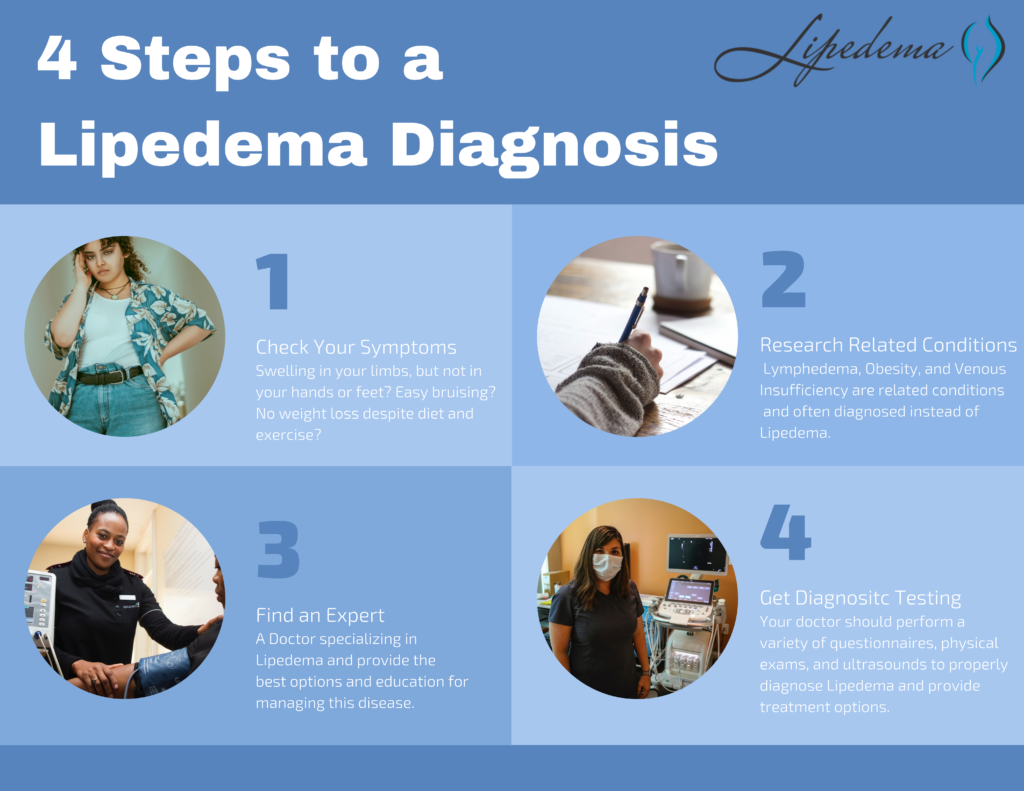
Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time to find a Lipedema specialist and get tested! Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
Note: There is no single test to diagnose Lipedema. Tests, however, are important to rule out a related disorder.
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema. Lipedema has many similarities to venous insufficiency (as explained above), so this can help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. Unfortunately, most hospital vascular labs complete Venous Doppler Ultrasounds with the patient lying down, While this is the typical way to find Deep Vein Thrombosis (DVT), it is definitely not a successful method to detect venous insufficiency. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
Vein insufficiency and other venous issues can cause your lipedema symptoms to worsen over time. Significant vein insufficiency can cause venous issues that are not superficial such as ulcers. If you are looking into surgical treatment for lipedema, you will need your vein issues to be treated first. Vein issues can cause problems during surgery if blood flow is not working correctly. It can also lead to poor wound healing after the procedure has been completed. The increased risk of blood clots is one factor any surgeon will want to avoid.
First – congratulations! We know the road to diagnosis is emotionally draining, physically painful, and it can feel lonely and discouraging. The time and research it takes to make it to this point are huge, and you should be proud of yourself and the courage it takes to be your own advocate. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.


After going through the diagnosis process and receiving a positive Lipedema diagnosis, most patients are relieved, overjoyed, and validated by their endless search. After years of living with the private struggle and knowledge that “something just isn’t right” in their body, putting a name to the issues is a huge win. And after an official diagnosis, there are many different treatment paths available to you! A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about the non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, they can give you an idea of what options may be available to you. Good luck!
June is Lipedema Awareness month, one in which the Lipedema community focuses (even more than usual) on how to reach women who have lived with this painful and distressing disease. While we’ve seen great strides in awareness, insurance coverage, and slightly greater recognition of this disease in the medical community, we continue to fight an uphill battle as women are underdiagnosed or completely dismissed when discussing their struggles and side effects with their providers. As a result, our team has put together some of the most important and most impactful information for all of you! Read it, re-read it, and share it with the women in your life. Some of the pain we’ve lived with for decades may actually have a life-changing solution!


Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.


Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper Lipedema diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
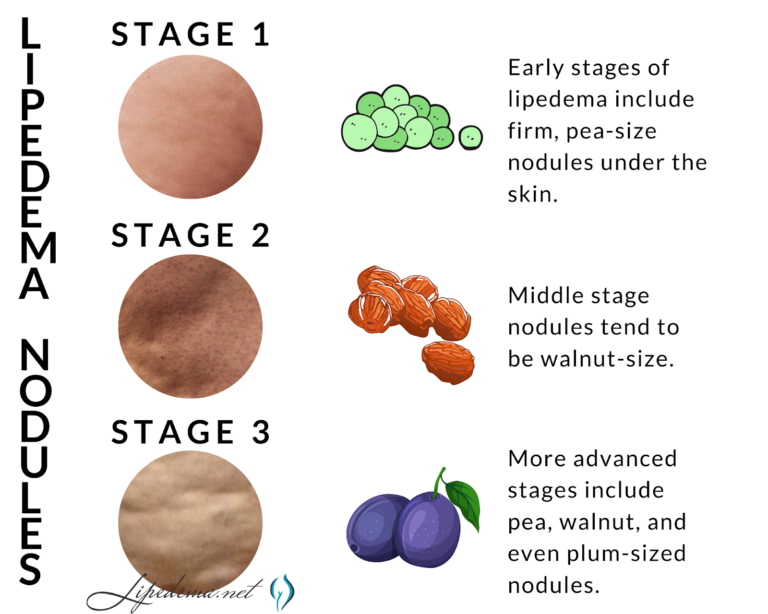
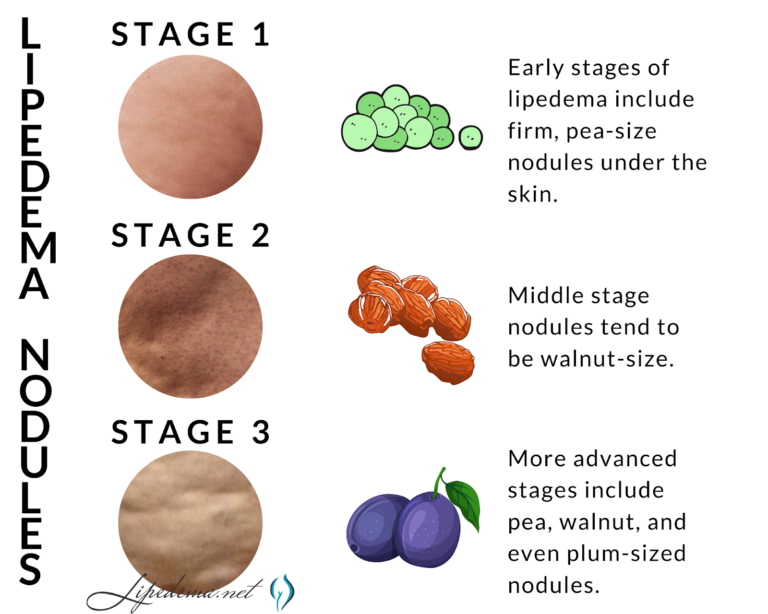
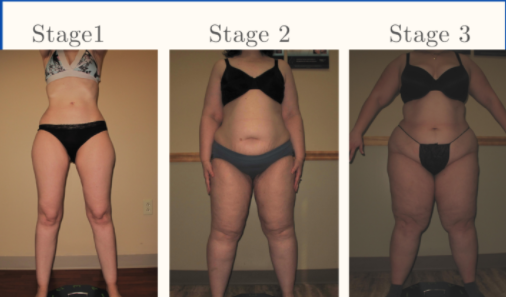
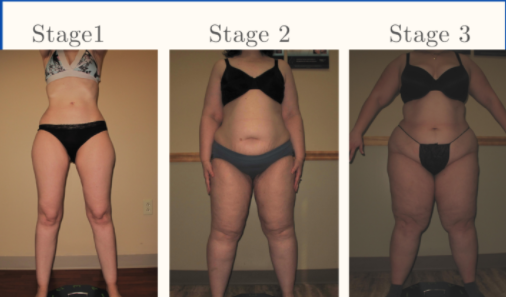
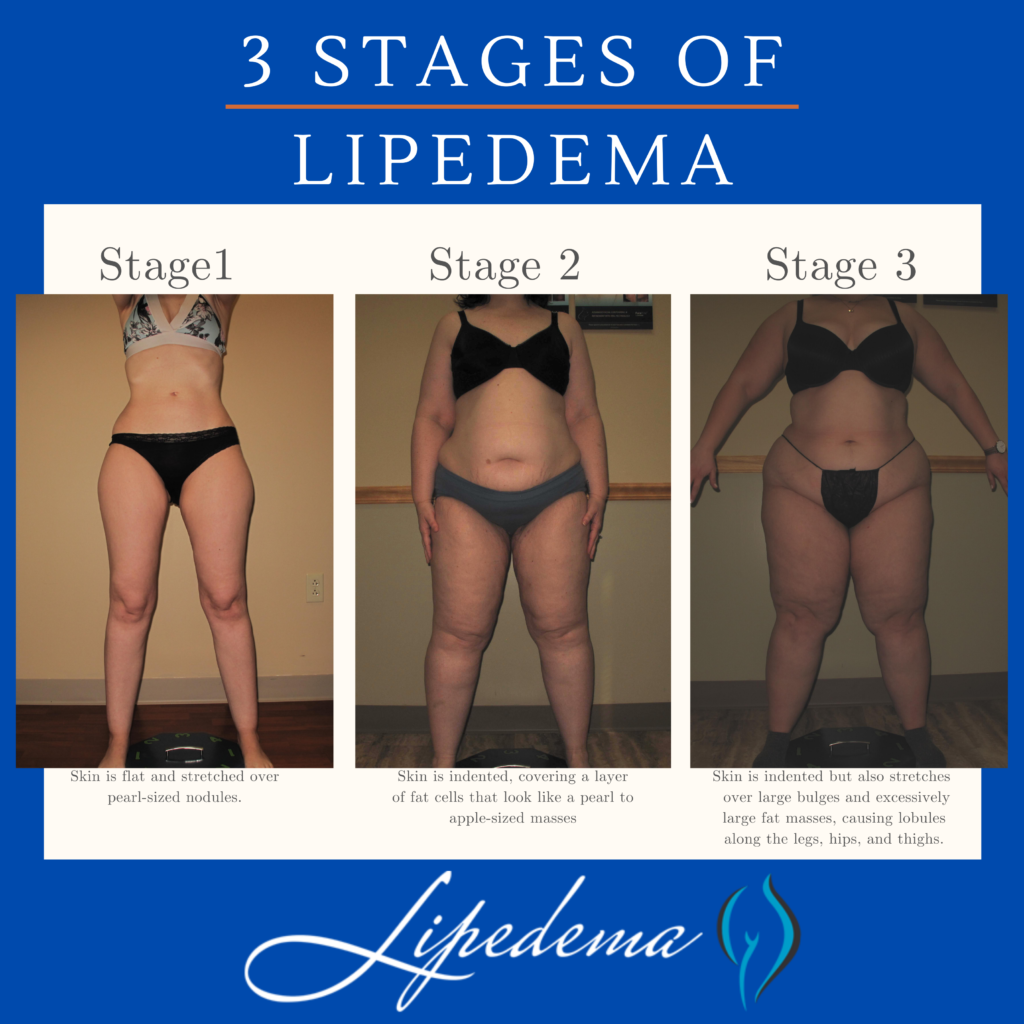
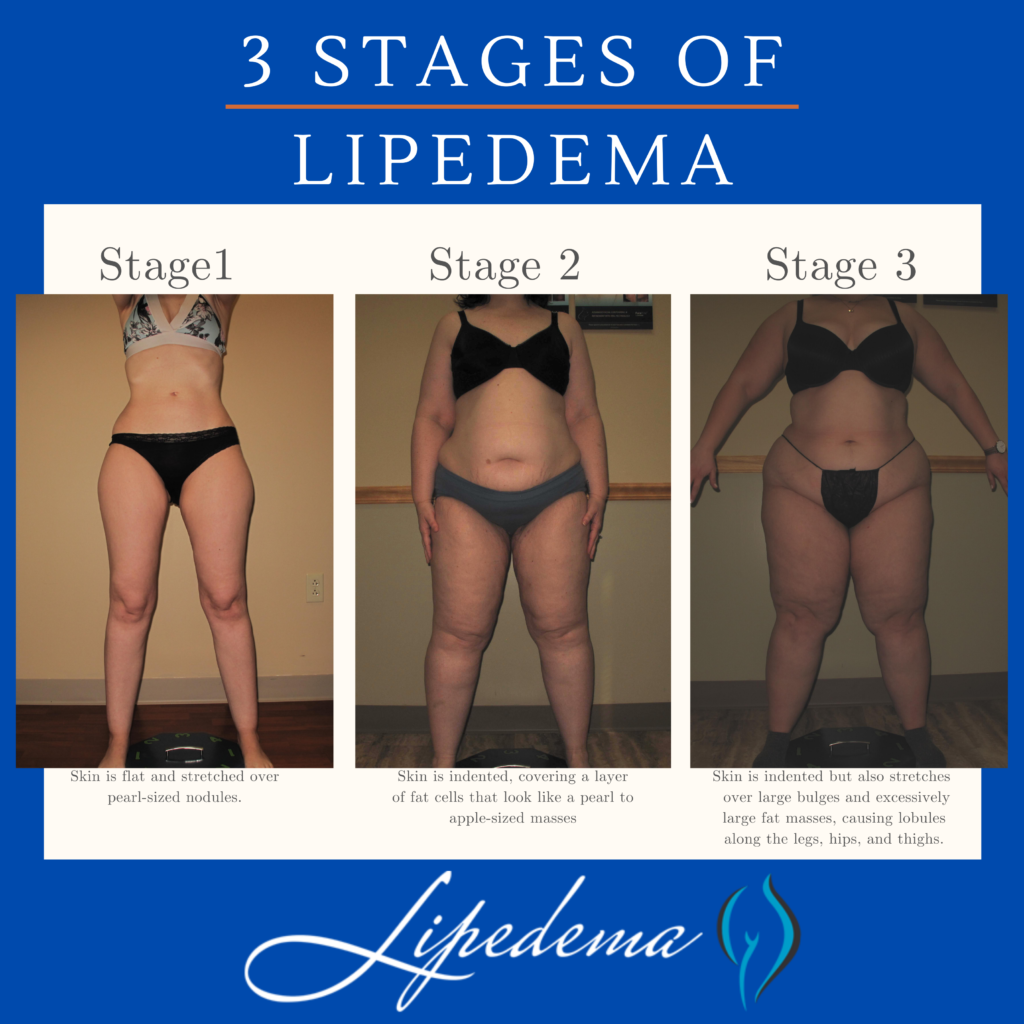
Overall, Lipedema appears in a series of three stages. Do any of these sounds like you?
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like a pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them. If you’re diagnosed with one of these conditions but you feel strongly that the diagnosis is incorrect, these summaries can help highlight why.
While Lipedema typically does not have to swell in the patient’s feet and hands, Lymphedema will always have swelling in these areas. Lipedema symmetrically affects both legs equally, but Lymphedema usually affects one leg or arm and leaves the other leg or arm unaffected. There may be overlap in these two diseases and treatments can be similar, but some patients only experience Lymphedema after their Lipedema progresses into later stages.
Obesity is much more common than Lipedema, and the most common misdiagnosis for it. While obesity is the accumulation of excess fat, stored centrally inside the abdomen or belly, Lipedema is the excess accumulation of fat out of proportion on the extremities, and typically not in the abdomen or belly. There may be overlap in these two conditions, too. In fact, sometimes obesity develops as a secondary condition due to the mobility problems caused by the Lipedema. So, not only is lipedema often misidentified as just obesity, but obesity can also complicate Lipedema, and be a symptom of it.
The symptoms of Lipedema and venous insufficiency are similar. They both cause heaviness, tenderness, fatigue, and swelling. They often both have discoloration in the shins, easy bruising, and prominent veins. In more advanced cases of venous insufficiency, not only does venous lymphedema develop, but a secondary Veno- Lipo- Lymphedema develops. With the overwhelmed lymph circulation, the ability to clear fatty acids from the affected tissue is compromised and a secondary fat accumulation occurs. In many cases, the best way to differentiate between lipedema and venous insufficiency and veno- lipo-lymphedema is to have a specialized standing venous Doppler ultrasound to check for venous reflux.
Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time to find a Lipedema specialist and get tested! Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema. Lipedema has many similarities to venous insufficiency (as explained above), so this can help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. Unfortunately, most hospital vascular labs complete Venous Doppler Ultrasounds with the patient lying down, While this is the typical way to find Deep Vein Thrombosis (DVT), it is definitely not a successful method to detect venous insufficiency. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
First – congratulations! We know the road to diagnosis is emotionally draining, physically painful, and it can feel lonely and discouraging. The time and research it takes to make it to this point are huge, and you should be proud of yourself and the courage it takes to be your own advocate. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.


After going through the diagnosis process and receiving a positive Lipedema diagnosis, most patients are relieved, overjoyed, and validated by their endless search. After years of living with the private struggle and knowledge that “something just isn’t right” in their body, putting a name to the issues is a huge win. And after an official diagnosis, there are many different treatment paths available to you! A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, it can give you an idea of what options may be available to you. Good luck!
Getting an initial Lipedema diagnosis is a challenge for many women suffering from it. In fact, an overwhelming majority of patients seeking treatment are well into their forties, fifties, sixties, or later in age, simply because they had never heard of lipedema or been diagnosed with it. After decades of being diagnosed with a high Body Mass Index (BMI) followed by a general obesity diagnosis or misdiagnosed as lymphedema, some of these women with lipedema sought alternate explanations for their pain, discomfort, and unsuccessful weight loss, despite regular diet, exercise, and in some advanced cases even after undergoing bariatric surgery.


The Body Mass Index (BMI) calculation is an unfortunate oversimplification of a person’s health, and ignores extremely important factors that are imperative for accurate diagnosis and treatment plans. Family history and genetics, general lifestyle and activity levels, age, gender, and body composition (muscle mass, water content, bone mass) are all essential parts of our health profile, all of which are ignored by the BMI calculation. Despite all of this, it continues to be used worldwide to aid in diagnosing (or misdiagnosing and oversimplifying) patient health profiles.
Body Mass Index (BMI) = weight in pounds (or kilograms) divided by height in feet squared (or meters squared).
Body Mass Index (BMI) is simply an overall numerical score (like height and weight) which is not a biological representation of a person’s overall health. While the World Health Organization (WHO) defines a BMI over 25 as overweight and over 30 as obese, this is actually an inaccurate and incomplete assessment. Overall, obesity is a condition where fat mass affects patients metabolically, chemically, and mechanically (for example, in your joints).
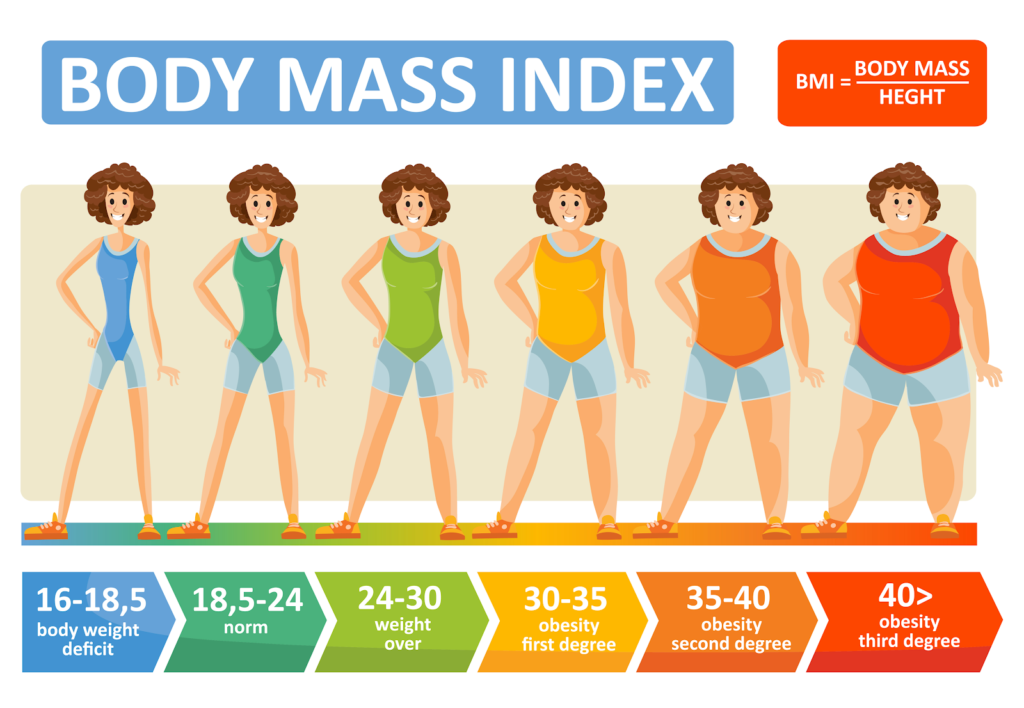
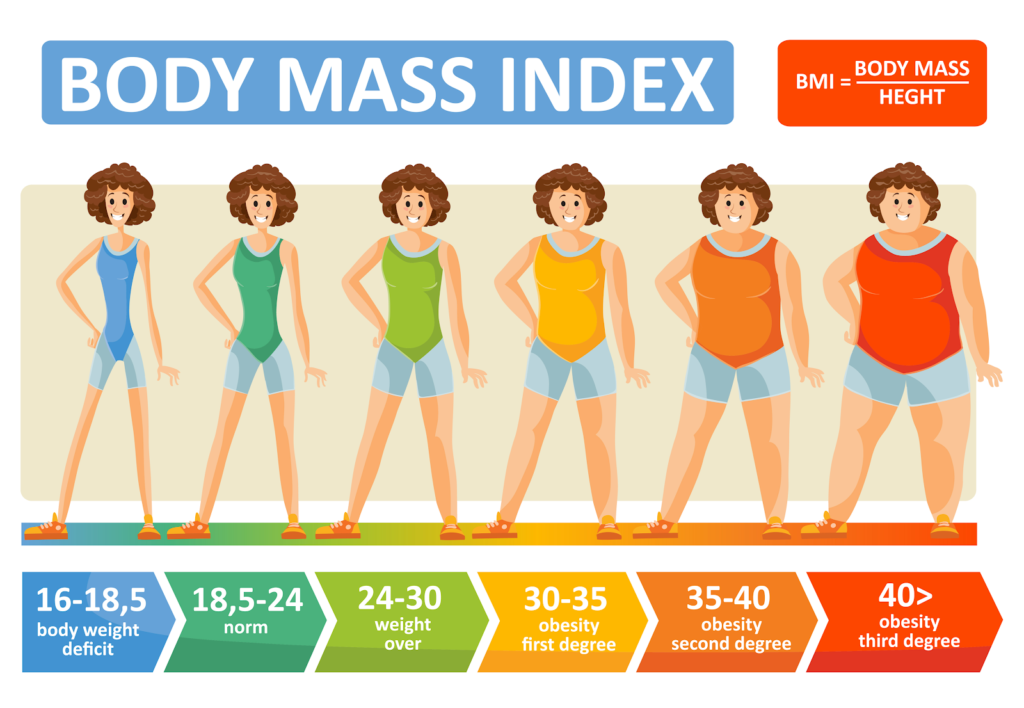
Because Body Mass Index (BMI) is a calculation that illustrations the relationship between a person’s weight and height, it equips healthcare providers with one tool in evaluating a patient’s overall health. Specifically, these ranges are used to categorize whether a person is underweight, in a normal weight range, overweight, or obese. While BMI does not provide the full picture of a patient’s health or the full body composition breakdown, it is a commonly used factor in diagnosing numerous diseases.
Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, and in many cases, excessive clustering of fat cells is noticed in the arms as well.
However, Lipedema causes fat in a different proportion on the body and has a different metabolic, chemical, and mechanical effect. Both obesity and Lipedema have increased BMIs, but they are not one and the same. When we use BMI as a blanket for Lipedema diagnosis, it’s an unfair and incomplete assessment.
Lipedema is metabolically the opposite of obesity – both are associated with excess fat accumulation, however, obesity presents with fat accumulated in the central area of the body, primarily in the abdomen, and is associated with diseases such as diabetes, high blood pressure, high cholesterol, and cardiovascular disease. However, lipedema presents with peripheral fat in the extremities, while the abdomen and/or waist are typically unaffected. But because both diseases increase a patient’s BMI, misdiagnoses are common and destructive. This illustrates one reason why BMI is not a biologically valid way to diagnose obesity or lipedema.
Interestingly, the origins of this formula were not used for individual health assessments at all! While Body Mass Index has been around since the early 19th century, the man who initially created the calculation knew at that time that it was flawed. Lambert Adolphe Jacques Quetelet, a Belgian mathematician, created the BMI formula as a way to quickly and easily estimate what percentage of the overall population might be obese. He was attempting to assist the country’s leaders in properly allocating resources in the 1830s. The formula Quetelet produced does is not biologically valid or based on any metabolic or physiologic princinciples. In other words, it is a 200-year-old hack that was never intended to describe diagnose obesity.
Simply put – where your body accumulates fat matters. This doesn’t only illustrate what you may or may not be suffering from (if anything) but also can help patients avoid misdiagnosis of more serious ailments that require more serious treatments. Ignoring fat distribution can easily lead to being either over or under-diagnosed, leaving patients with a false sense of security in their health, or in the reverse, being treated for something they don’t actually have.


For example, researches from the Medical Research Council (MRC) Epidemiology Unit in the UK concluded through a series of studies that waist size, regardless of BMI, can be a greater indicator of a person’s risk of developing type 2 diabetes. After gathering data from over 340,000 individuals from 8 European countries, Dr. Claudia Langenberg and her MRC team found that a larger waist circumference is just a likely to lead to developing Type 2 Diabetes as someone with a BMI over 30 (considered “obese”) (2). They found that non-obese males (according to their BMI) with a waist circumference of at least 40.2 inches was at just as much risk for developing Type 2 Diabetes as a male with a BMI indicating they were obese. They found the same indication in females with a waist of 34.6 inches or greater.
BMI calculations are oversimplified and do not account for the fact that bone is denser than muscle and twice as dense as fat, nor the amount of lean muscle an individual has. A person with strong bones, good muscle tone, and low fat will have a high BMI, so athletes and fit, health-conscious individuals will be classified as overweight, or even obese.
A female bodybuilder may have a higher BMI, but looking at their BMI number alone and diagnosing them as obese would be inaccurate. Similarly, while Lipedema will affect the BMI number, this BMI measure will not accurately pinpoint the cause of the higher measurement.


Additionally, fluid and water weight are not included in BMIs simply calculation, which can also lead to more serious outcomes when misdiagnosed. For example, women with Lipedema and Lymphedema will inevitably have an accumulation of fat cells, however, both these diseases are also classified by the excessive accumulation of fluid in affected areas. When missed or ignored, women suffering from these diseases are often misdiagnosed as obese rather than obtaining treatment for the source of their higher BMIs.


Perhaps one of the most obvious and frustrating blind spots of the BMI calculation is that it will be more dramatically simplified for individuals who do not fall into an “average” category for height (between 5’5” and 5’9”). For both shorter and taller individuals, their “normal” BMI ranges will shrink or widen and distort the reality of their health.
For example, a person who is 6’2” in height and weighs 230 pounds has a BMI of 29.5, putting them at the far end of the overweight category, and teetering on obese. Despite having a lean body, their doctor may tell them there are concerns about their BMI and to focus on weight loss. At their height, they would need to be at around 170 pounds to fall into a “normal” category – which for many at this height would be extremely underweight and malnourished.
On the other hand, a young child who is only 4’4 and weighs 85 pounds would also be considered overweight, despite this being a generally healthy weight. Their pediatrician may push for diet or lifestyle changes that aren’t actually needed, both worrying the parents unnecessarily and instilling an unrealistic and unfair body image in the child at a very young age.
The story is almost always the same, and we hear it all the time; women are living in pain for the majority of their lives, begging for medical explanations and solutions, and are coming up empty. These women spend years – sometimes decades – struggling with uncontrollable and disproportional weight, deep bruising and tender skin from the lightest of touches, and have constant swelling. Their weight gain is typically in their limbs or “trunk” and widely does not affect their feet, hands, or upper body from the waist up. These symptoms progress, cause more pain, and often get to the point that women are unable to walk upstairs, take a brisk walk, or even sit for long periods of time without feeling intense pain and discomfort.
The consistent diagnosis from their primary care doctors centers around their weight, and are diagnosed for general obesity, and prescribed treatments that range from diet and exercise to more extreme surgeries to curb appetites and encourage weight loss. Unfortunately, for those who have Lipedema, these treatments will turn up useless and ineffective, yet their doctors assume the issue is from the patient’s lack of dedication to the prescribed program, rather than the misdiagnosis of the disease known as Lipedema.
Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.
Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
Lipedema Symptoms Checklist:
☑Tender skin that is sensitive to the touch, feels pressure when walking or climbing stairs, crossing your legs, or sitting for long periods of time.
☑Skin’s surface feels nodular and firm, like beans in a bean bag or rubber balls.
☑Skin’s surface is uneven, with large bulges and valleys up and down. Areas that were traditionally thought of as cellulite are much more dramatic and bulging.
☑Skin’s temperature is relatively cool.
☑Legs feel heavy and tired.
☑Swelling in the affected area (legs, arms), worsening during the day, and better at night after you’re able to elevate your limbs (such as laying in bed).
☑Easy bruising.
☑Visible veins.
☑Disproportionate fat accumulation, not affected by calorie restriction. Think extreme “pear-shaped” body.
☑Feet and hands are unaffected by weight gain or swelling. As a result, there’s often a “cuff” at the ankles or wrists.
Overall, Lipedema appears in a series of three stages. Do any of these sounds like you?
If one of these stages sounds like you, and you checked off multiple items on the list above, you may have Lipedema, but it’s impossible to say for sure. The only way to know for sure is to get a proper Lipedema diagnosis, which in itself is an important process.
The diagnosis of Lipedema is made based on a clinical evaluation from a physician with specific knowledge and experience of the disease in combination with supporting tests that rule out other diagnoses. For this reason, it’s no surprise that Lipedema is a poorly recognized and under-appreciated disease in the United States – it takes an expert to recognize it, and finding an expert is tough if you’ve just learned about it yourself! The recognition of characteristic features of Lipedema and the elimination of other conditions that can be confused with Lipedema is the key to the proper diagnosis. We know it can be overwhelming, but knowing as much as possible before speaking with your doctor or seeking out an expert is another tool in your pocket to ensure you receive the care you need. You can read more about related conditions here, but it’s important to know the main points to advocate for yourself.
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them. If you’re diagnosed with one of these conditions but you feel strongly that the diagnosis is incorrect, these summaries can help highlight why.
While Lipedema typically does not have to swell in the patient’s feet and hands, Lymphedema will always have swelling in these areas. Lipedema symmetrically affects both legs equally, but Lymphedema usually affects one leg or arm and leaves the other leg or arm unaffected. There may be overlap in these two diseases and treatments can be similar, but some patients only experience Lymphedema after their Lipedema progresses into later stages.
Obesity is much more common than Lipedema, and the most common misdiagnosis for it. While obesity is the accumulation of excess fat, stored centrally inside the abdomen or belly, Lipedema is the excess accumulation of fat out of proportion on the extremities, and typically not in the abdomen or belly. There may be overlap in these two conditions, too. In fact, sometimes obesity develops as a secondary condition due to the mobility problems caused by the Lipedema. So, not only is lipedema often misidentified as just obesity, but obesity can also complicate Lipedema, and be a symptom of it.
The symptoms of Lipedema and venous insufficiency are similar. They both cause heaviness, tenderness, fatigue, and swelling. They often both have discoloration in the shins, easy bruising, and prominent veins. In more advanced cases of venous insufficiency, not only does venous lymphedema develop, but a secondary Veno- Lipo- Lymphedema develops. With the overwhelmed lymph circulation, the ability to clear fatty acids from the affected tissue is compromised and a secondary fat accumulation occurs. In many cases, the best way to differentiate between lipedema and venous insufficiency and veno- lipo-lymphedema is to have a specialized standing venous Doppler ultrasound to check for venous reflux.


Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time for the final step – finding a Lipedema specialist and getting tested! Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema. Lipedema has many similarities to venous insufficiency (as explained above), so this can help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. Unfortunately, most hospital vascular labs complete Venous Doppler Ultrasounds with the patient lying down, While this is the typical way to find Deep Vein Thrombosis (DVT), it is definitely not a successful method to detect venous insufficiency. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
First – congratulations! We know the road to diagnosis is emotionally draining, physically painful, and it can feel lonely and discouraging. The time and research it takes to make it to this point are huge, and you should be proud of yourself and the courage it takes to be your own advocate. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.
After going through the diagnosis process and receiving a positive Lipedema diagnosis, most patients are relieved, overjoyed, and validated by their endless search. After years of living with the private struggle and knowledge that “something just isn’t right” in their body, putting a name to the issues is a huge win. And after an official diagnosis, there are many different treatment paths available to you! A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, it can give you an idea of what options may be available to you. Good luck!
Lipedema continues to be a poorly identified condition where diagnoses are often avoided by US physicians. Identifying lipedema involves a clinical evaluation from a medical physician with expert knowledge regarding this condition. Two factors that are critical in finding a proper lipedema diagnosis include identifying an abnormal fat deposition in impacted areas and identifying symptoms of lipedema.
Far too often Lipedema is misdiagnosed as obesity. The abnormal fat deposition of lipedema is very different from obesity. Individuals with lipedema typically accumulate disproportionate fat in soft tissue just below the skin on the arm and legs. Individuals with obesity typically see a proportional increase of fat issue around the body but it is more concentrated inside the abdomen, called visceral fat. Individuals with lipedema will instead see a much greater fat accumulation be around extremities and not the abdomen which is described as disproportionate when compared to the rest of the body.
Lipedema can be identified with five different types of the condition depending on where the fat tissue is found predominantly. Type I identifies lipedema with fat pockets around the buttocks. Type II identifies lipedema with fat around the hips and thighs in addition to the buttocks. Type III identifies fat tissue around the calves, ankles, and thighs. Type IV identifies lipedema with pockets of fat tissue on the arms while Type V is lipedema with fat tissue found exclusively on the calves and ankles.
Where does lipedema fat accumulate? Find out here.
It helps to properly identify lipedema by recognizing many of its common symptoms. Individuals who have been properly diagnoses often have tender skin that is sensitive to walking and pressure. Limbs affected by lipedema appear to be “fluffy” and have a rubbery feel to them. The skin tissue will eventually harden and feel like beans in a bag. Skin tissue will also lose elasticity and become uneven. The overall temperature of the skin will cool. Your legs will begin to feel heavy and lead to overall fatigue. Individuals with a newer development of lipedema will see that swelling will be frequent during the day and subside at night. Individuals who have been dealing with lipedema for years will notice that the swelling will progress at later stages. Finally, individuals with lipedema will also notice visible veins under the skin on impacted limbs and will bruise easily.
Properly identifying symptoms of lipedema and observing abnormal fat distribution will help with diagnosing this condition. Physicians now use tests to help with their diagnoses such as venous Doppler ultrasound and lymphoscintigraphy. Additional research will help with properly identifying lipedema from obesity and other fat-related conditions. Contact us for your proper lipedema diagnosis.