Good news, these conditions are not life-threatening on their own. However, if undiagnosed or untreated, they will worsen over time and may contribute to several other secondary ailments and complications. If you have signs of swelling, and pain in your body, especially in your legs and arms, seek treatment starting with your primary care physician. Ongoing care of lipedema and lymphedema with a vascular expert lessens the risk of other serious problems.
For instance:
Remember, you are in control of how you manage your health and well-being. Educate yourself and do not hesitate tol ask for help. A great resource for emotional support from the comfort of your home is https://www.mind-diagnostics.org. A study by researchers at the University of California, Berkeley found online counseling can be just as effective as face-to-face therapy while being more convenient, affordable, and accessible.
Sources:
https://www.healthgrades.com/right-care/symptoms-and-conditions/lymphedema
https://my.clevelandclinic.org/health/diseases/8353-lymphedema
https://www.nhs.uk/conditions/postural-tachycardia-
syndrome/#:~:text=Postural%20tachycardia%20syndrome%20(PoTS)%20is,as%20postural%20orthostati
c%20tachycardia%20syndrome
https://www.aapmr.org/about-physiatry/conditions-treatments/pain-neuromuscular-medicine-
rehabilitation/degenerative-joint-disease
https://www.nhs.uk/mental-health/conditions/body-
dysmorphia/#:~:text=Body%20dysmorphic%20disorder%20(BDD)%2C,affects%20both%20men%20and%
20women.
https://www.betterhelp.com/study/Study_of_BetterHelp_eCounseling.pdf
In celebration of Lipedema Awareness month back in June, Dr. Wright and Dr. Herbst updated the world on the latest insights and understandings on Lipedema vs normal fat. Sponsored by Lipedema UK and Lipedema LIO ITALIA, we’ve summarized the key learnings and helpful information below. Don’t miss updates in the future on our “Lipedema in the News” section, and feel free to watch the full 1.5-hour webinar here.
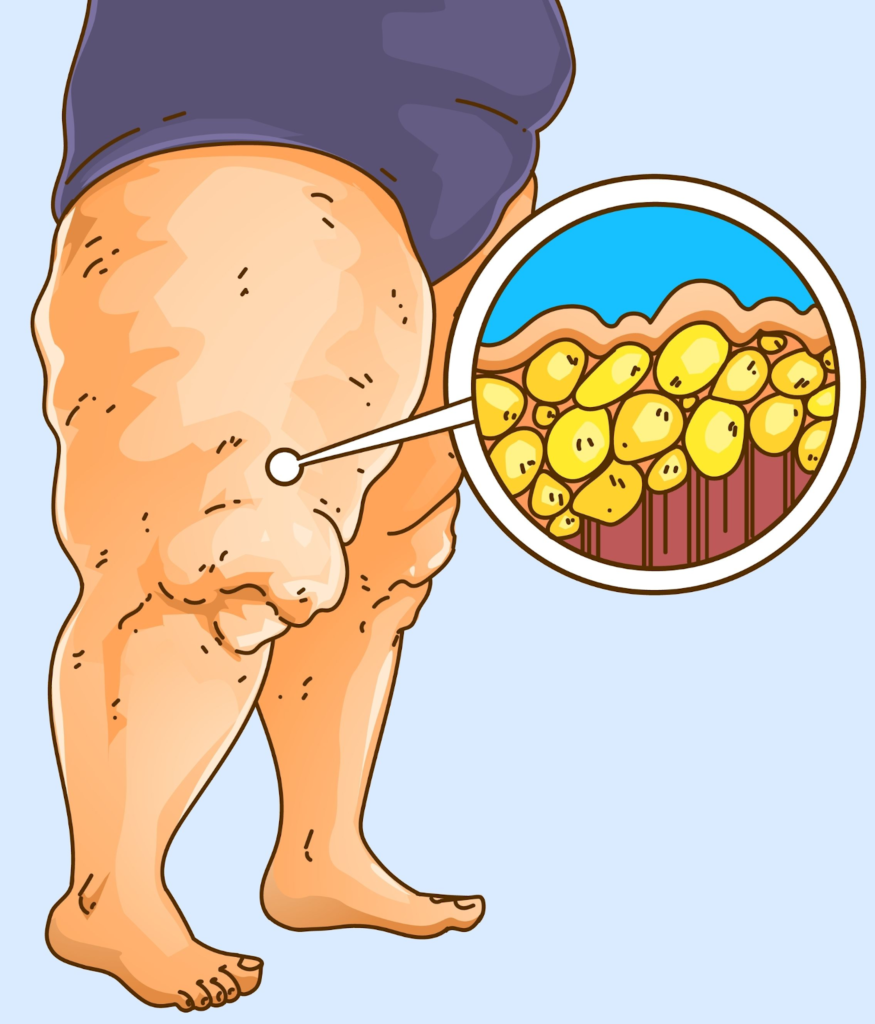
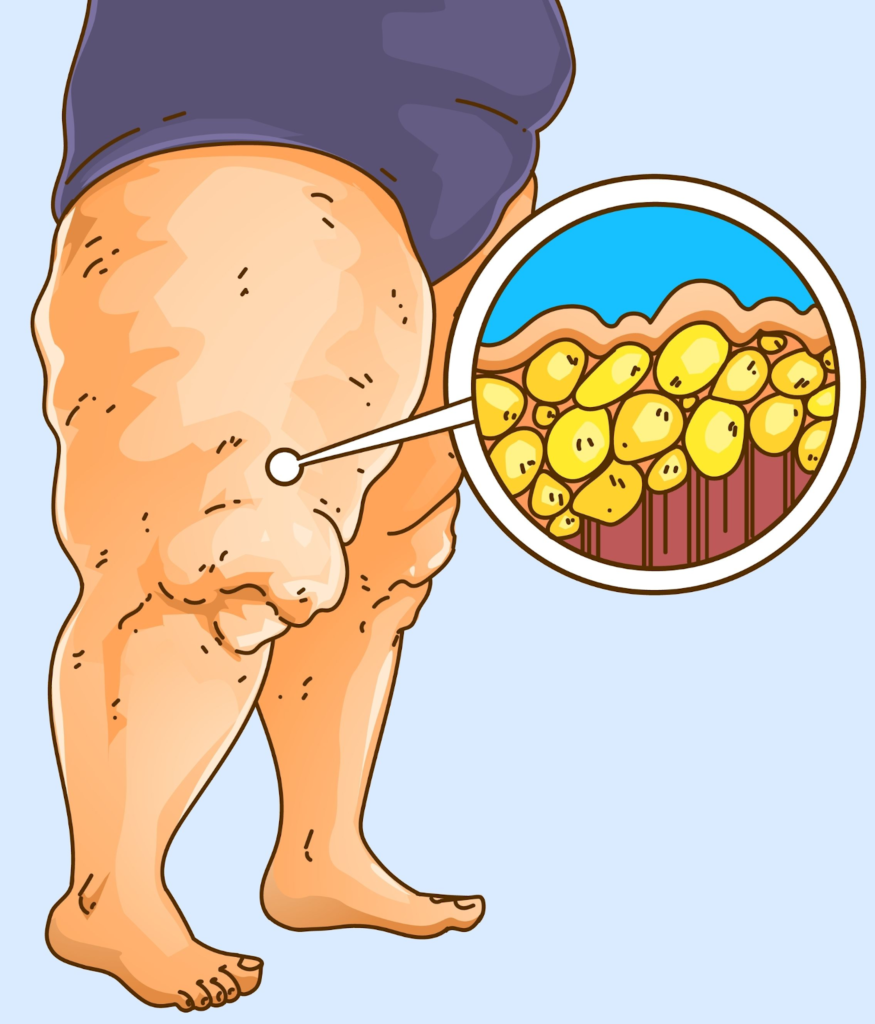
Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. Sufferers living with lipedema experience easy bruising and tenderness, pain in the affected areas, and significant disability in daily life. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back. Little is known about the disorder, and it’s often misdiagnosed and incorrectly treated as general obesity.
For anyone affected, diet and exercise alone aren’t effective ways to get rid of Lipedema fat; Lipedema fat has proved relatively immune to these lifestyle changes and won’t budge. While women are likely to experience some weight loss with a healthy diet and regular exercise routines, weight loss is usually mostly loss of non-Lipedema fat. In these instances, the painful, stubborn fat remains. This cycle becomes a difficult one to break for those with the disorder: Yo-yo dieting leads to more weight gain. More weight gain leads to increased pain and disability. Increased pain and disability make it more challenging to manage mobility and secondary obesity increases. Lipedema fat also appears to be relatively resistant to bariatric surgery, meaning many women are undergoing dangerous surgeries without experiencing the intended benefit of significant loss of lipedema fat.
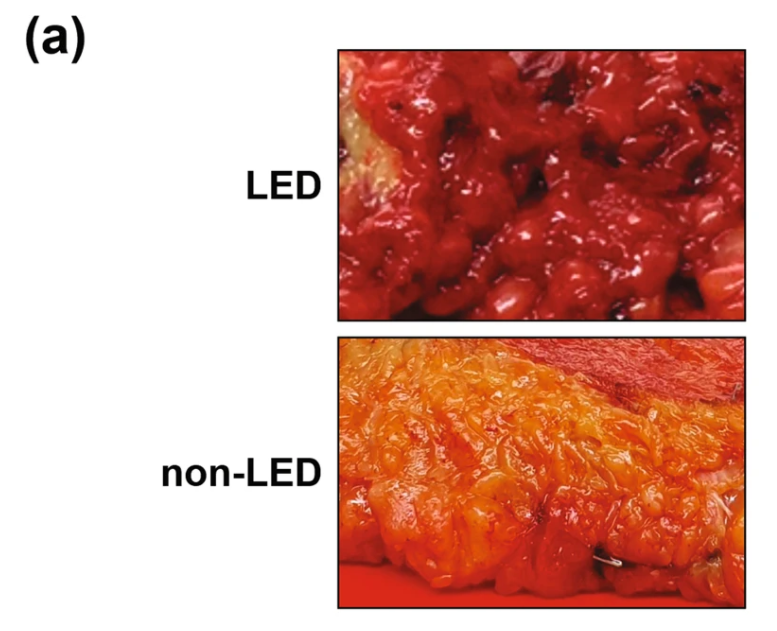
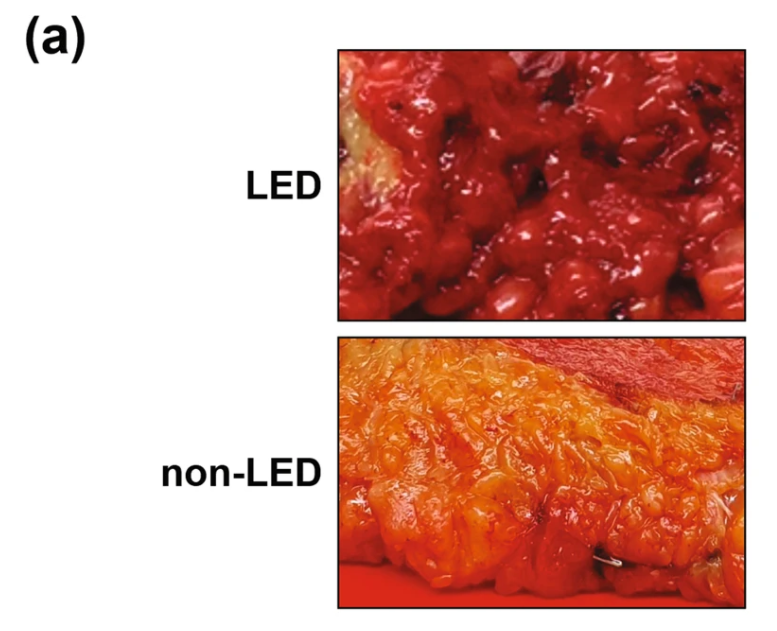
Lipedema adipose fat tissue is different from normal adipose tissue. When looking at this fat tissue in lipedema patients, we find a more fibrous, nodular, tender adipose tissue than in patients without lipedema. The look and feel of lipedema fat tissue can be physically seen when performing lipedema surgery in addition to under a microscope when analyzing the tissue components. It’s clearly a different type of fatty tissue, explaining why lipedema patients experience different side effects and symptoms than those with traditional obesity.
A study published in the International Journal of Obesity in November 2021 (Ishaq et al) highlighted the cellular differences that signaled the differences in lipedema fat than traditional adipose tissue.
The study had the following key findings:
This means that lipedema fat actually causes the body to turn on a different gene than we see in non-lipedema patients. Fat tissue from lipedema was compared to location, gender and age-matched tissue from non-lipedema patients. In the photo below, we see a heatmap gene expression of adipose tissue by Z-score fold-change value: red indicates upregulation and blue indicates downregulation.
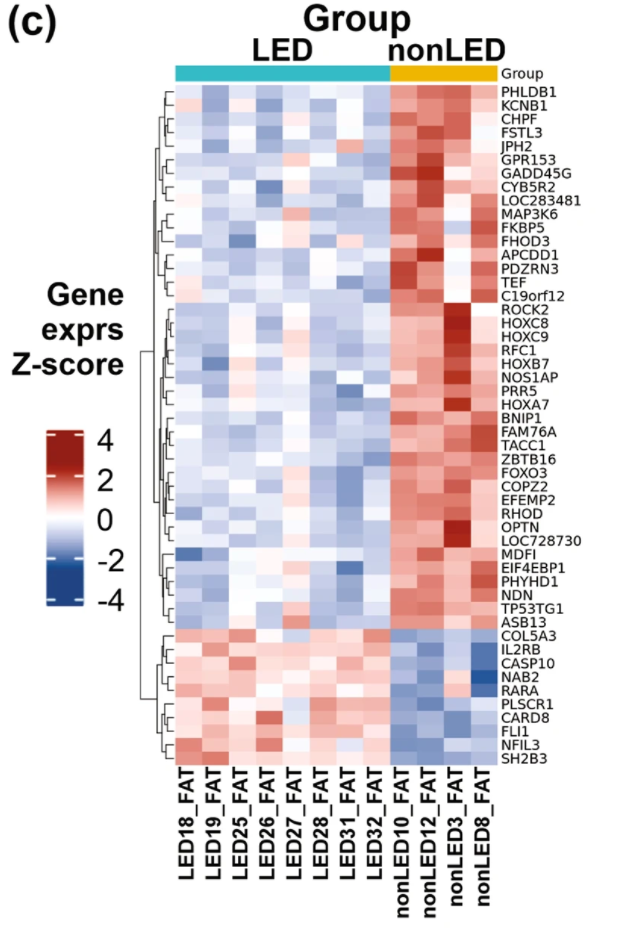
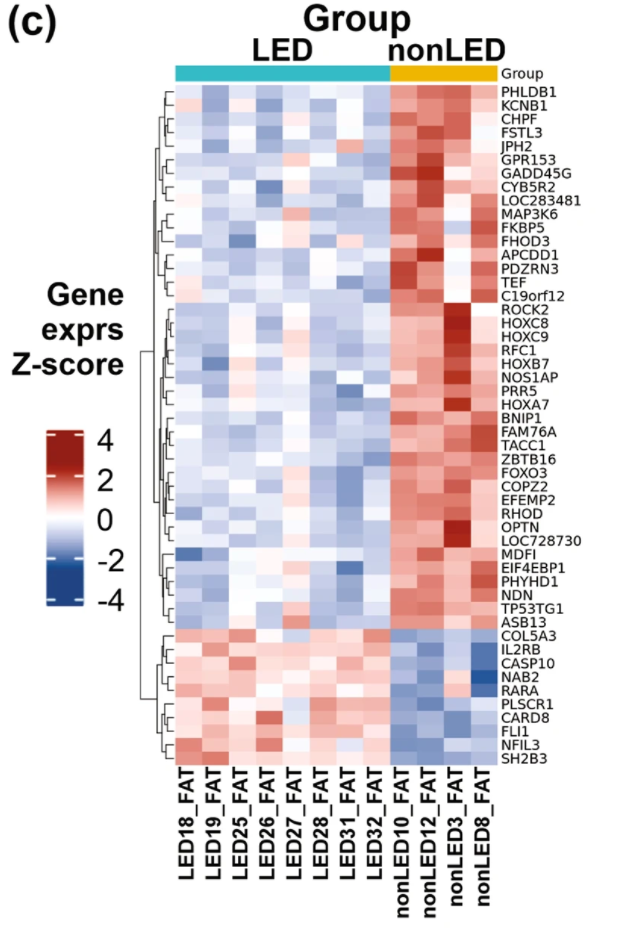
What does this mean? Lipedema fat has a different metabolism, characterized by a differing production of phospholipid production compared to normal fat. Lipedema adipocytes are shown on the left half [Header Bright Red] and non-lipedema adipocytes are shown on the right side of the hierarchal plot of lipid composition [Green Header over columns].


In this study, stem cells [ADSCs] from lipedema fat were compared to stem cells of matched people without lipedema. The stems in lipedema are increased in number.
Note: ADSCs are stem cells. They can continuously divide and renew themselves. The ADSCs stem cells can also become mature fat cells or other types of cells to sustain or grow fat tissue. This means that lipedema fat replicates their cells more than regular fat, increasing the growth of this painful, fibrous fat tissue in lipedema patients!
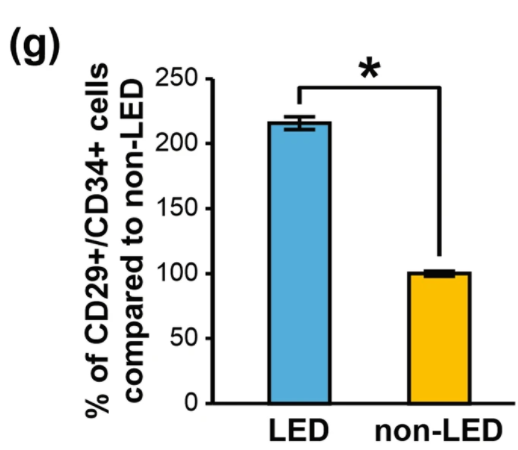
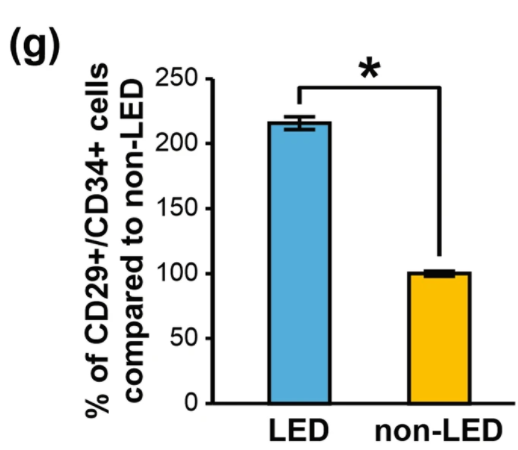
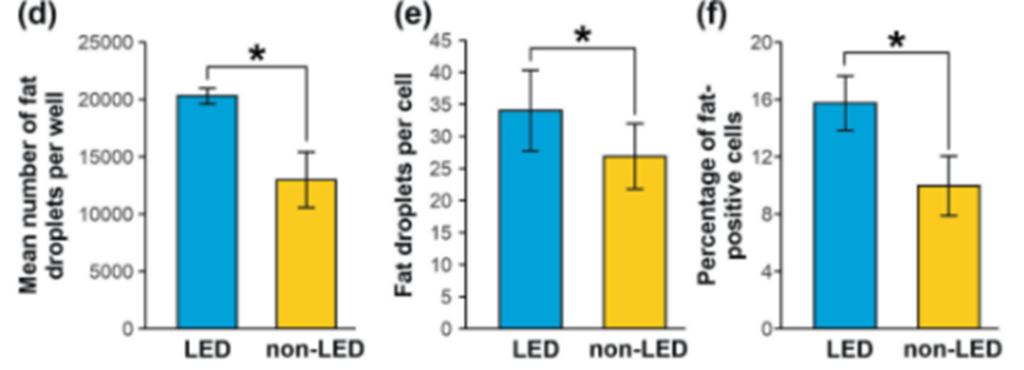
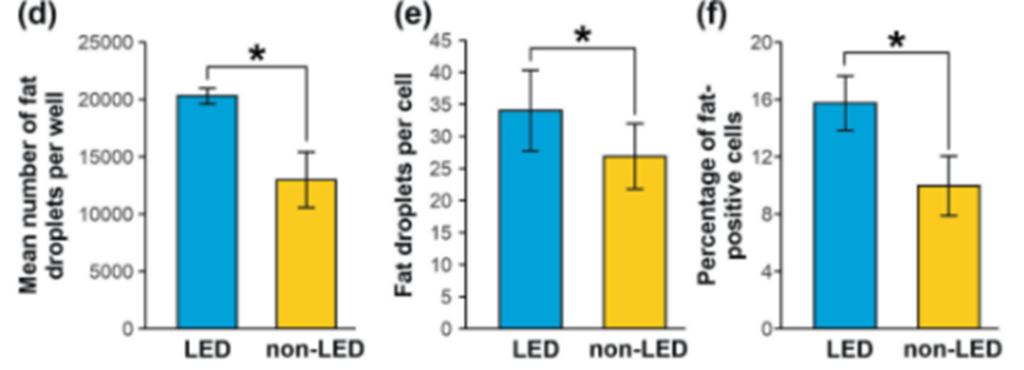
Additionally, Lipedema Stem Cells contain Fat Droplets and have More Fat Droplets per cell than non-lipedema fat cells. The number of fat droplets, percentage of fat-positive cells, and the number of fat droplets per cell were significantly increased in lipedema adipocytes compared to controls. Lipedema fat cells had more fat in them, and the presence of fat droplets in stem cells (ASCDs) indicates maturation toward an adipocyte.
Cell-cycle genes involved in regulating cell growth and proliferation are dysregulated in lipedema ADSCs and may contribute to the increased adipocyte number, and maldistribution and accumulation of dystrophic fat in lipedema. Because of the lack of regulation, lipedema cells again are able to replicate and grow at a higher speed and frequency than non-lipedema fat.
For example, Bub1, which is one of the cell cycle genes, is turned on more or upregulated in lipedema.
First, and most validating for people with lipedema, these findings prove that lipedema fat and normal fat are not the same. Adipocytes and stem cells from individuals with lipedema are structurally different and behave differently from cells of normal fat tissue. Second, diet and general nutrition do not affect lipedema fat in the same way it does for non-lipedema fat. Given the same nutritional support, lipedema-derived stem cells proliferated compared to normal fat-derived stem cells. And third, the faster growth of lipedema fat compared to non-lipedema fat can be explained at a cellular level. The different cell biology of the lipedema cells that leads to hyperproliferation of fat tissue may explain disproportionate growth compared to other adipose tissue.
While these lipedema vs normal fat findings are exciting for lipedema providers, and even more validating for patients seeking insights and treatment options, one question still remains: Is the biology of lipedema fat different because of genetic differences or is the difference in the fat cell biology of lipedema a product of an altered environment?
Even with all the challenges presented by lipedema, there are those who you can trust. Dr. Wright continues to strive for better education, research, and coverage for the lipedema community. Do not let these challenges bring you down even further; let Dr. Wright and his expert team help you to reduce the symptoms of lipedema and live your life fully! Dr. Wright can help find the right procedure to help manage your lipedema symptoms. Don’t let lipedema take over your life; contact us today!
Hi everyone – it’s Cat again!
If you haven’t read my story or seen any of my videos before, I’m a long-time patient of Dr. Wright and am working towards completing a total of five Lipedema liposuction surgeries with him. I’ve put together some helpful tips and a bit about my story, and you can find all my videos on Dr. Wrights YouTube channel.
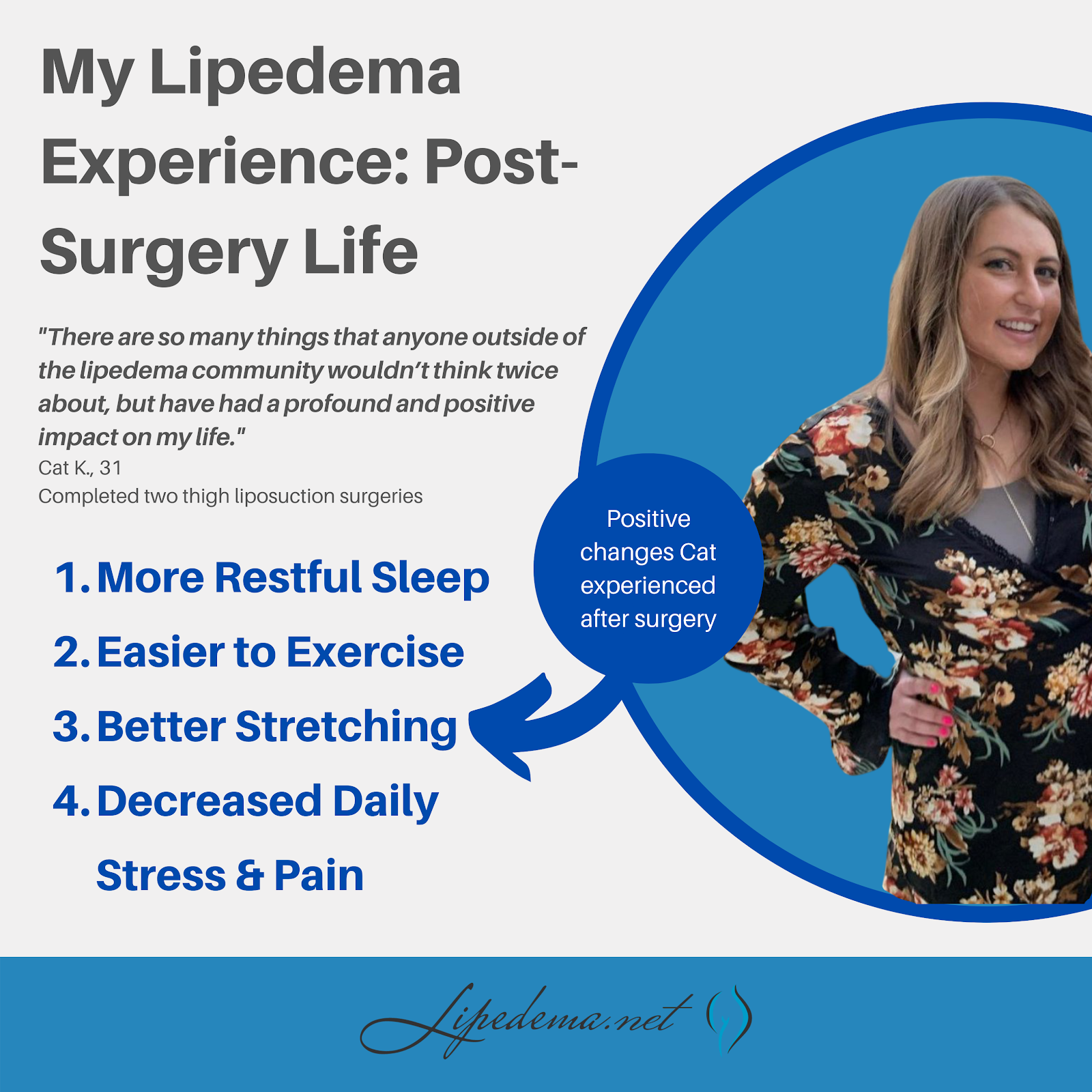
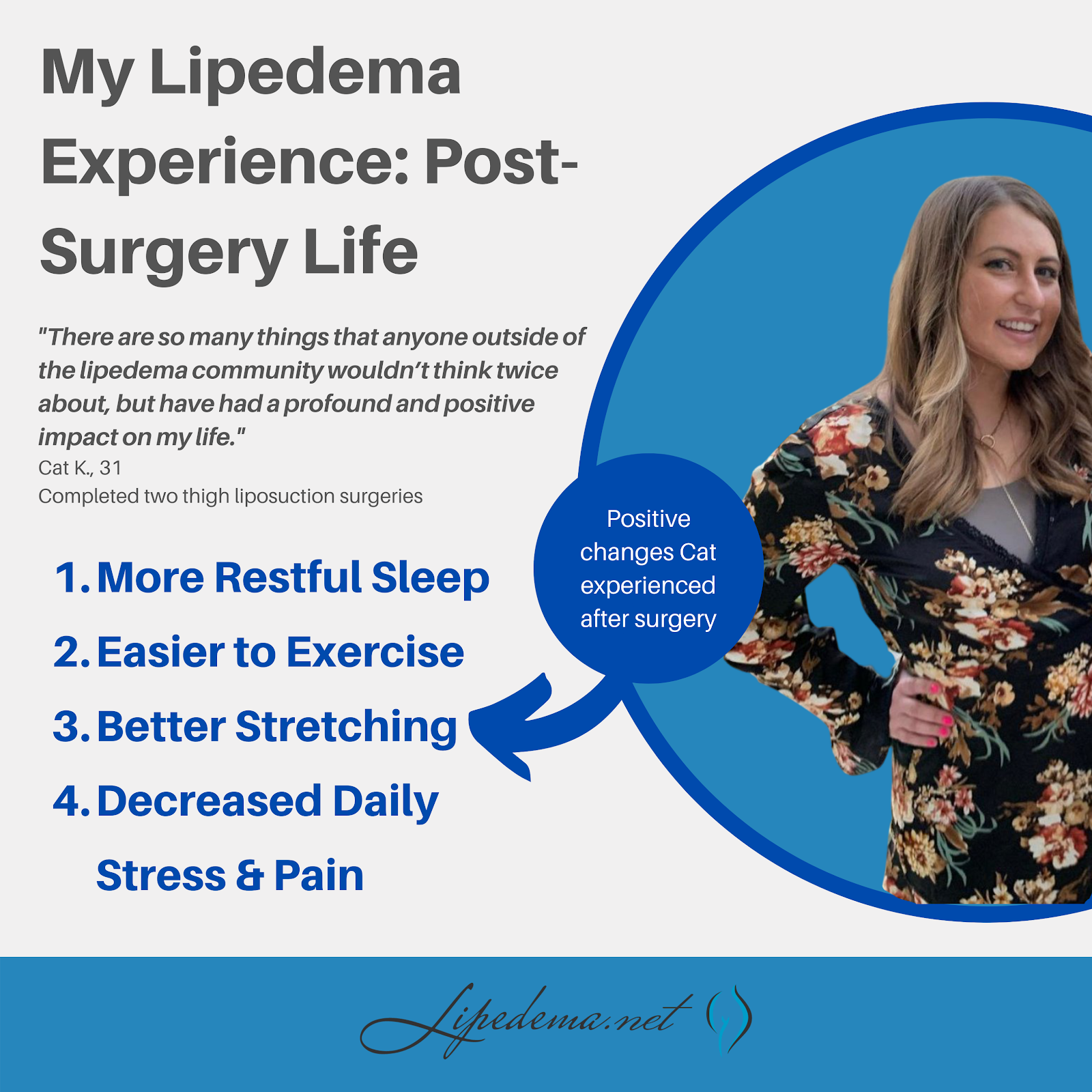
At the end of February, I hit the one-year mark since undergoing my second Lipedema surgery. My initial goal was to get all five surgeries completed within one year of being diagnosed (in October 2019). However, thanks to COVID-19 and life and money and insurance unhelpful companies, here I am; It’s already March of 2021, and I’m praying I can get a third surgery done soon! Until then, I want to continue helping women like me who are struggling with Lipedema, in the hopes that I can show you the light at the end of the tunnel, and help make the journey a little less overwhelming! In the video below and through this post, I’ll take you through what my life has been like since recovering from my 2nd surgery, and what it’s like being half-healed; I’m living in the in-between of some areas being treated while others are still in the midst of the struggle.
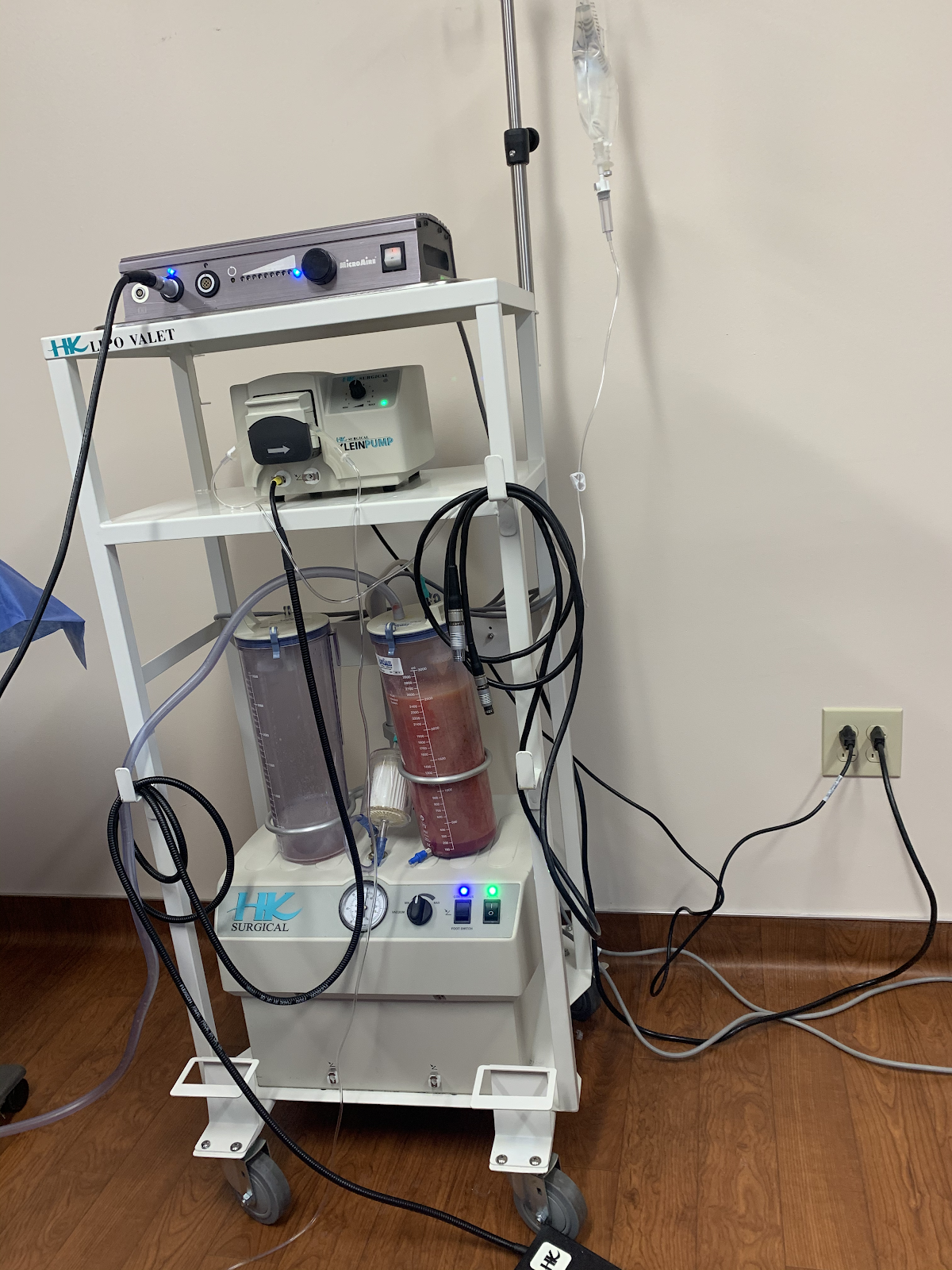
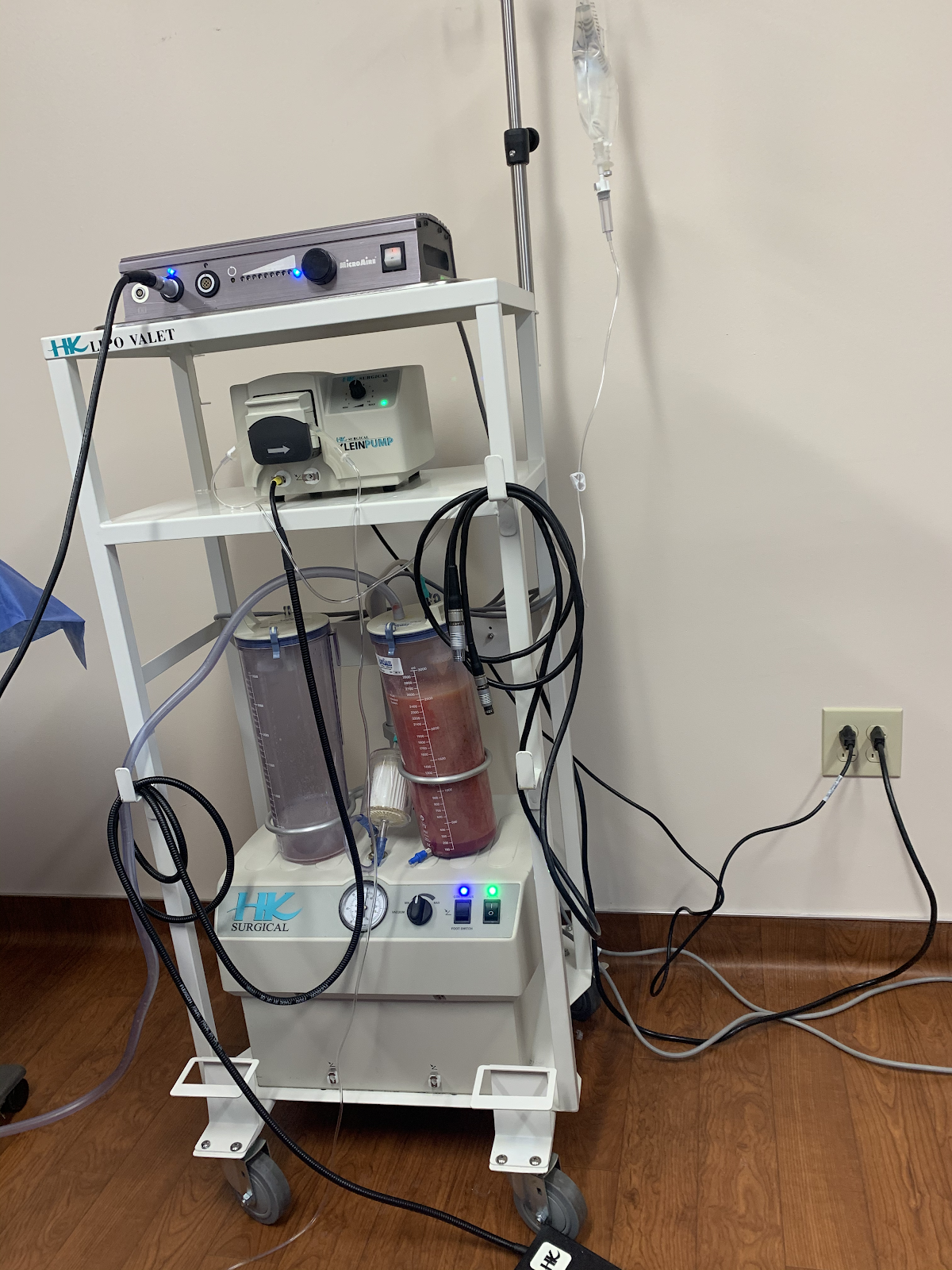
After being officially diagnosed and working on non-surgical treatments, I met with Dr. Wright and his team to determine what surgeries I would need and on what areas of my body. We determined that I had Lipedema swelling and fat in my legs, abdomen, and arms, and would need a total of five surgeries: My legs, abdomen, front of my thighs, back of my thighs + buttocks, and my calves. I completed the front of my thighs in December 2019 and the back of my thighs and buttocks in February 2020. I had about 8 liters of fat removed in the first Lipedema removal surgery, and 12 liters (INSANE) in my 2nd surgery. To give you an idea of this volume, 8 liters is about 2 gallons of fat. So between the two, I’m free of a huge amount of lippy fat and am about 35 pounds lighter.
Because I live in Austin and Dr. Wright’s office is in St. Louis, the COVID-19 pandemic has made continuing surgeries difficult. His expertise, kindness, and genuine passion for helping women like us make the travel well worth it under any other circumstances, but we’re trying to be extremely cautious with flights. Over the last year, my partner and I have even thought about making the 13-hour drive to his office rather than continuing to wait, but the thought of riding in a car post-surgery is daunting.


In mid-march, I have a virtual consultation with Dr. Wright to touch base and make plans for my 3rd surgery, this time focused on my calves. I’m so excited to get the next phase rolling, and hoping that the world calms down and allows for safe travel soon!
My first and second surgery recoveries were actually extremely different. While the overall process and the surgeries themselves were all the same, I needed a week to recover the first time, and about two weeks to recover the second time. My backside was a bit harder to recover from due to the large volume of fat that was taken, and simply because sitting and laying down was more uncomfortable. I was able to drive, work, and get back to most of my routine within a few days, but I preferred to take it easy for the full two weeks because I was still leaking tumescent fluid, and putting on those compression garments is tough for the first two weeks (more like the first 6 weeks, just to set your expectations…) – I preferred to do this in the comfort of my home for as long as possible.


Interestingly, in the first surgery, I had a lot of numbness on the inside of my thighs, which lasted about a month. Numbness is completely normal after liposuction as your nerves start to heal, so it wasn’t necessarily worrisome, but it was uncomfortable. It made walking extremely uncomfortable and, to the delight of my friends and family, I waddled like a duck for several weeks. So even though I spent more time on the couch after my second surgery, I still “enjoyed” it far more than the first. It’s just proof that every area of the body and every patient is different. But I loved the end results of both!
As I sit here today, I find myself in a funny limbo in regards to living with my lipedema. The already-treated areas of my legs are doing great! No bruising, no swelling, and no sensitivity at all. In fact, my thighs even feel different to the touch – the remaining fat (I’m no bodybuilder yet, haha) is soft and fluffy – something I’ve never experienced before. The only fat I’ve ever encountered has been dominated by my lipedema fat – firm or tight, bulging, and sore.
But because I’m mid-treatment overall, the remaining areas of my body are still very much experiencing the pain of lipedema. The tops of my legs are great, and the bottom of my legs are struggling. My arms and abdomen are progressing and gaining more fluid and lipedema fat. As I work out, I get excited to see small changes in my thighs and depressed seeing no changes in the other parts of my body. When I bump into something with my calf and I get a pang of pain, I get angry and then grateful when I realize I can’t remember the last time I felt that in my thighs. It’s so many mental and physical feelings and changes all at once!
There are so many things that anyone outside of the lippy community wouldn’t think twice about but have had a profound and positive impact on my life post-surgery.
As I move into my next three surgeries, I’m sure I’ll have more updates! But until then, what questions do you have about my lipedema journey or the general process for getting treatment? Leave a comment or contact Dr. Wright and his team, and we’d be more than happy to put together more resources for you! We’re all in this together!
All the best,
Cat
The story is almost always the same, and we hear it all the time; women are living in pain for the majority of their lives, begging for medical explanations and solutions, and are coming up empty. These women spend years – sometimes decades – struggling with uncontrollable and disproportional weight, deep bruising and tender skin from the lightest of touches, and have constant swelling. Their weight gain is typically in their limbs or “trunk” and widely does not affect their feet, hands, or upper body from the waist up. These symptoms progress, cause more pain, and often get to the point that women are unable to walk upstairs, take a brisk walk, or even sit for long periods of time without feeling intense pain and discomfort.
The consistent diagnosis from their primary care doctors centers around their weight, and are diagnosed for general obesity, and prescribed treatments that range from diet and exercise to more extreme surgeries to curb appetites and encourage weight loss. Unfortunately, for those who have Lipedema, these treatments will turn up useless and ineffective, yet their doctors assume the issue is from the patient’s lack of dedication to the prescribed program, rather than the misdiagnosis of the disease known as Lipedema.
Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.
Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
Lipedema Symptoms Checklist:
☑Tender skin that is sensitive to the touch, feels pressure when walking or climbing stairs, crossing your legs, or sitting for long periods of time.
☑Skin’s surface feels nodular and firm, like beans in a bean bag or rubber balls.
☑Skin’s surface is uneven, with large bulges and valleys up and down. Areas that were traditionally thought of as cellulite are much more dramatic and bulging.
☑Skin’s temperature is relatively cool.
☑Legs feel heavy and tired.
☑Swelling in the affected area (legs, arms), worsening during the day, and better at night after you’re able to elevate your limbs (such as laying in bed).
☑Easy bruising.
☑Visible veins.
☑Disproportionate fat accumulation, not affected by calorie restriction. Think extreme “pear-shaped” body.
☑Feet and hands are unaffected by weight gain or swelling. As a result, there’s often a “cuff” at the ankles or wrists.
Overall, Lipedema appears in a series of three stages. Do any of these sounds like you?
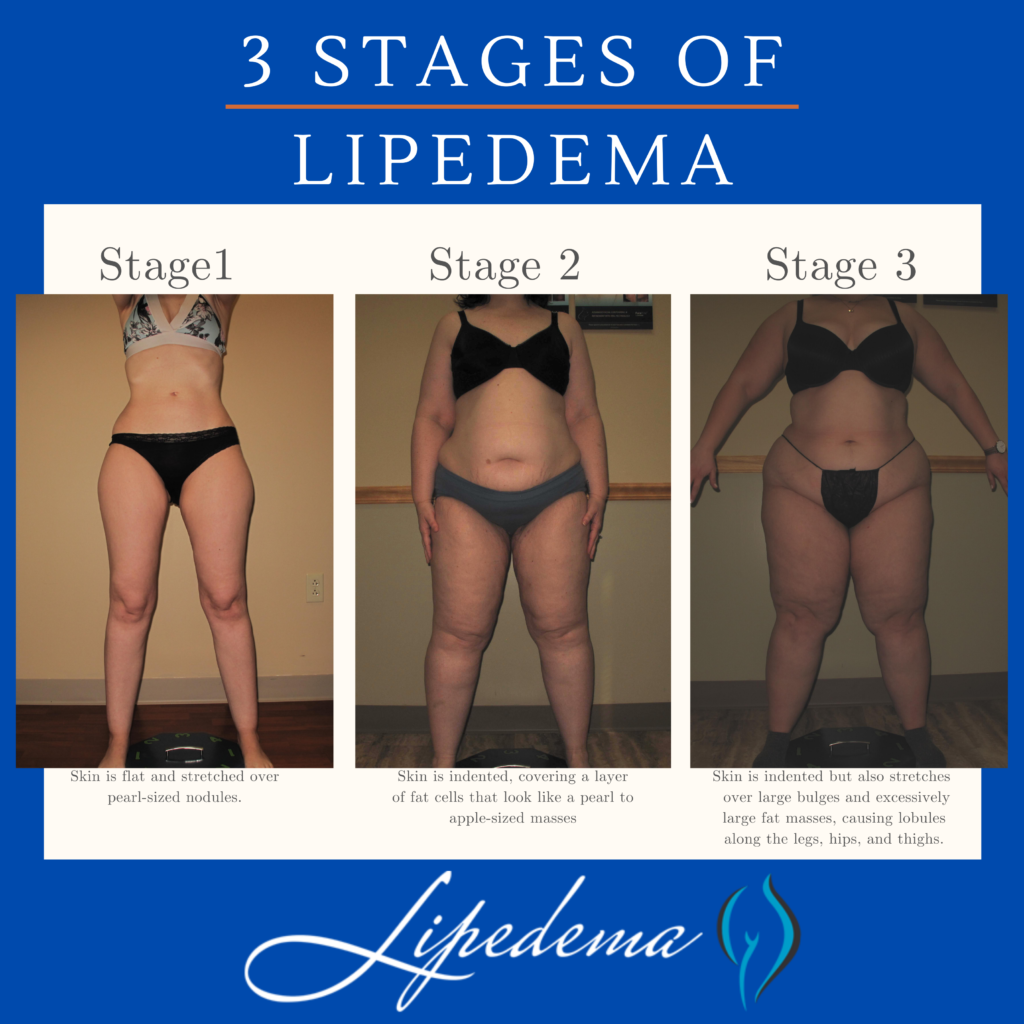
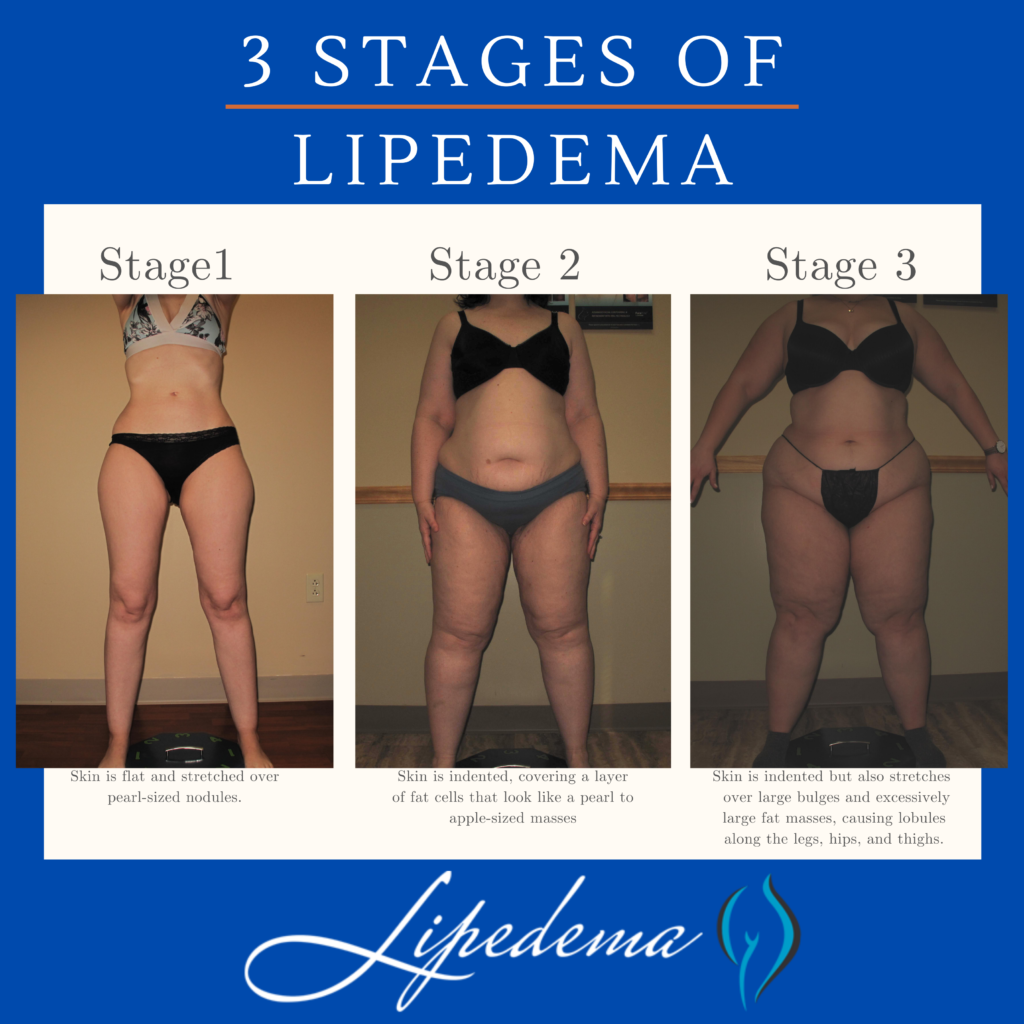
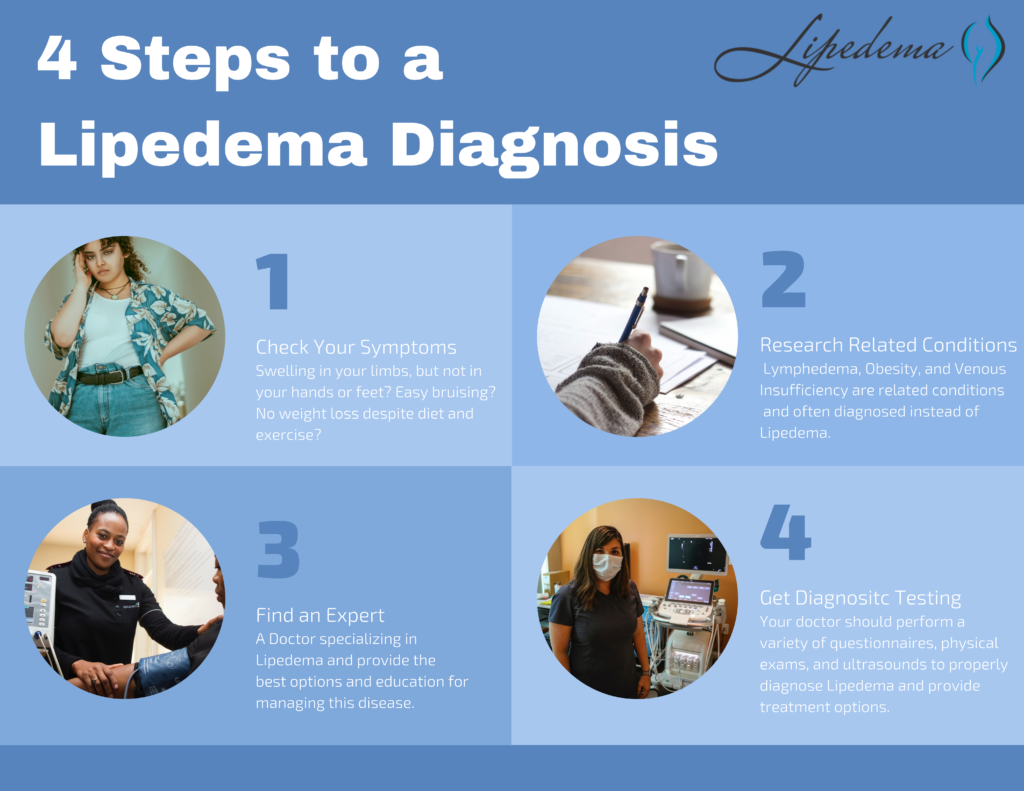
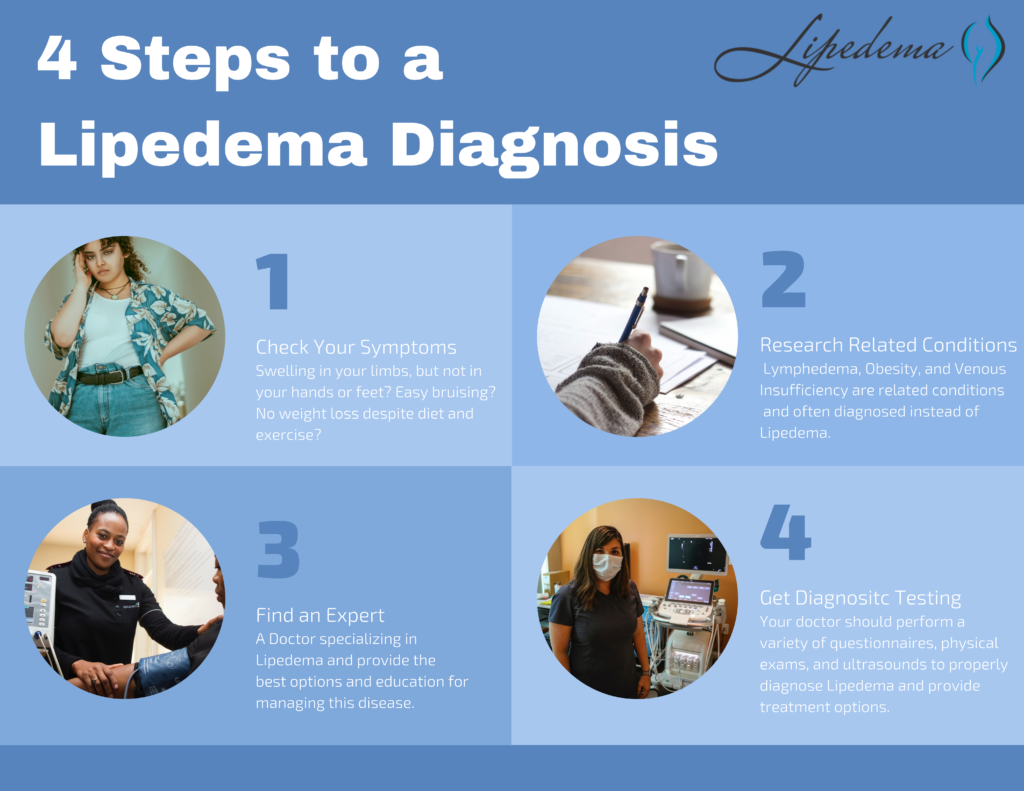
If one of these stages sounds like you, and you checked off multiple items on the list above, you may have Lipedema, but it’s impossible to say for sure. The only way to know for sure is to get a proper Lipedema diagnosis, which in itself is an important process.
The diagnosis of Lipedema is made based on a clinical evaluation from a physician with specific knowledge and experience of the disease in combination with supporting tests that rule out other diagnoses. For this reason, it’s no surprise that Lipedema is a poorly recognized and under-appreciated disease in the United States – it takes an expert to recognize it, and finding an expert is tough if you’ve just learned about it yourself! The recognition of characteristic features of Lipedema and the elimination of other conditions that can be confused with Lipedema is the key to the proper diagnosis. We know it can be overwhelming, but knowing as much as possible before speaking with your doctor or seeking out an expert is another tool in your pocket to ensure you receive the care you need. You can read more about related conditions here, but it’s important to know the main points to advocate for yourself.
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them. If you’re diagnosed with one of these conditions but you feel strongly that the diagnosis is incorrect, these summaries can help highlight why.
While Lipedema typically does not have to swell in the patient’s feet and hands, Lymphedema will always have swelling in these areas. Lipedema symmetrically affects both legs equally, but Lymphedema usually affects one leg or arm and leaves the other leg or arm unaffected. There may be overlap in these two diseases and treatments can be similar, but some patients only experience Lymphedema after their Lipedema progresses into later stages.
Obesity is much more common than Lipedema, and the most common misdiagnosis for it. While obesity is the accumulation of excess fat, stored centrally inside the abdomen or belly, Lipedema is the excess accumulation of fat out of proportion on the extremities, and typically not in the abdomen or belly. There may be overlap in these two conditions, too. In fact, sometimes obesity develops as a secondary condition due to the mobility problems caused by the Lipedema. So, not only is lipedema often misidentified as just obesity, but obesity can also complicate Lipedema, and be a symptom of it.
The symptoms of Lipedema and venous insufficiency are similar. They both cause heaviness, tenderness, fatigue, and swelling. They often both have discoloration in the shins, easy bruising, and prominent veins. In more advanced cases of venous insufficiency, not only does venous lymphedema develop, but a secondary Veno- Lipo- Lymphedema develops. With the overwhelmed lymph circulation, the ability to clear fatty acids from the affected tissue is compromised and a secondary fat accumulation occurs. In many cases, the best way to differentiate between lipedema and venous insufficiency and veno- lipo-lymphedema is to have a specialized standing venous Doppler ultrasound to check for venous reflux.


Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time for the final step – finding a Lipedema specialist and getting tested! Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema. Lipedema has many similarities to venous insufficiency (as explained above), so this can help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. Unfortunately, most hospital vascular labs complete Venous Doppler Ultrasounds with the patient lying down, While this is the typical way to find Deep Vein Thrombosis (DVT), it is definitely not a successful method to detect venous insufficiency. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
First – congratulations! We know the road to diagnosis is emotionally draining, physically painful, and it can feel lonely and discouraging. The time and research it takes to make it to this point are huge, and you should be proud of yourself and the courage it takes to be your own advocate. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.
After going through the diagnosis process and receiving a positive Lipedema diagnosis, most patients are relieved, overjoyed, and validated by their endless search. After years of living with the private struggle and knowledge that “something just isn’t right” in their body, putting a name to the issues is a huge win. And after an official diagnosis, there are many different treatment paths available to you! A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, it can give you an idea of what options may be available to you. Good luck!
Getting an initial diagnosis for Lipedema is typically time-consuming, challenging, and emotionally draining. Why? Because the misdiagnosis starts from a very early age and comes from those closest to us, and even from the patient themselves. Those of us suffering from Lipedema commonly hear phrases like, “You’re just big-boned,” or, “You have a pear shape, it’s just your body.” Family members are quick to suggest that larger bodies or a specific body shape run in the family, and there’s not much we can do about it. While the assertion is harmless, it may not be the full truth. And while it’s normal for many women to accumulate fat in their thighs, hips, and buttocks, when is it beyond the normal range? When is it more than just “curvy”?
The typical explanations we hear in adolescence accelerate in adulthood. After years of trying every diet and exercise routine under the sun, many seek medical advice in the hopes of an explanation. This time, the common phrases range from “Maybe you need to control your appetite and portion sizes,” to, “I know you say you’re working out and have a balanced diet, but the scale says otherwise.” By the time we learn about Lipedema and make our way a specialist, we’ve been dismissed by other professionals, exhausted by our endless efforts, and worn down by the journey.
The question that ultimately leads us to a Lipedema diagnosis is a simple one which we are asking from childhood; “My legs look fat – Is that normal?” The mainstream answers and commonly accepted explanations are what lead us to constant frustration. If calories we take into our body equal calories we burn off, we “shouldn’t” be gaining weight, right? If the calories we take into our body are fewer than the calories we are burning, we should lose weight. Right? If this equation rings true, then why are my legs so different?
To answer this question, we must first ask several more. First, let’s evaluate how our legs may physically look different than other overweight body types. Do you tend to gain weight around the “trunk” of your body? For example, if you fold your body in half at the hips, would your bottom half be significantly larger and out of proportion with the top half? It’s common for women with Lipedema to report vastly different clothing sizes between their upper and lower bodies, such as wearing a size M or L shirt, but a size XXL in pants. For me, I’ve always had an extremely slim waist, so much so that my swimsuit tops were an extra small, and my bottoms were an XL. As much as I wanted to wear a one-piece to cover up as much as possible, there simply was not a size that existed to fit my extreme pear-shaped body. The shape of your legs and how you carry weight is also telling. Do your legs appear thick and column-like, without much definition or shape around the knees? This was a key feature of my body that ultimately led to my personal discovery of Lipedema.
Next, evaluate the effects of your weight gain on your ankles and feet. Do your feet appear to gain weight similar to the rest of your legs? Or, does the weight gain stop at the ankle, and your feet remain relatively “normal” in size? This may cause a cuff-like effect around the ankle as if you had a rope tightened around the bottom of your legs. If you’re like me, you might not be able to wear certain types of boots or shoes, because they either accentuate your cankles or they aren’t able to fit over your calves.
With Lipedema fat, we experience fat accumulation in specific areas, which may help indicate if your weight gain is normal or not. If you’re gaining pockets of fat that are out of proportion to other areas, this may be a tip-off that you have Lipedema. This can be difficult to catch because patients are often in the third stage of Lipedema when it becomes clear that the gains are irregular across the body. Here a few other areas of the body that can help determine if your weight gain may be due to Lipedema:


In addition to the differences in physical appearance, women with Lipedema also commonly experience a range of painful symptoms. Do you bruise easily in the affected areas? For example, many patients report that they’ll get bruises from lightly bumping a chair, or may not know where their injuries came from at all. Additionally, do you feel pain from light touches to the affected areas? If your family pet jumps on you, or if your child grabs your leg, would this cause you pain? Typically, this bruising and sensitivity lead to an inability to remain physically active, further increasing weight gain.
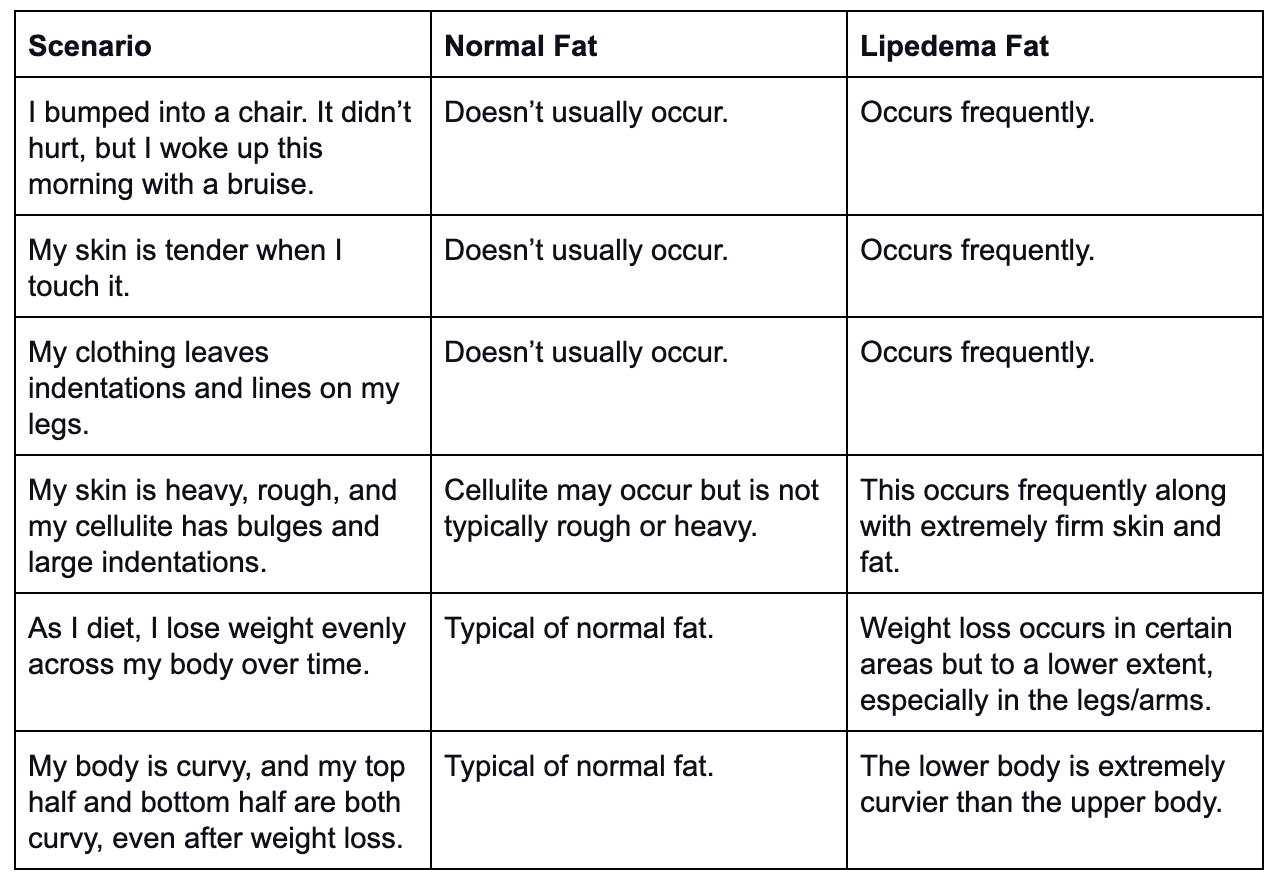
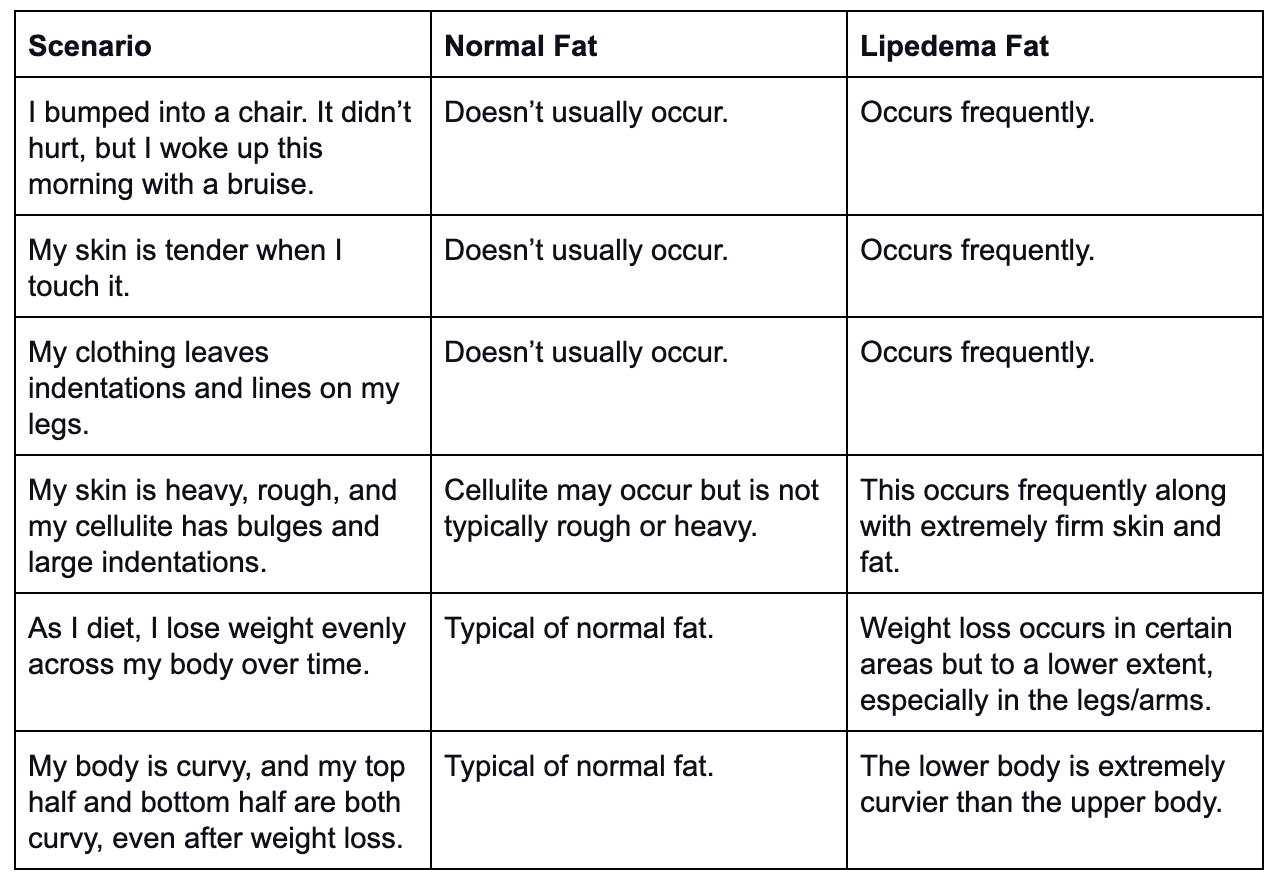
How do you determine what’s normal fat vs. Lipedema fat, and what’s a normal sensation versus an abnormality caused by Lipedema? This part can be difficult to determine, especially because many side effects aren’t detected until the later stages of Lipedema. So how can we catch this as early as possible? The table below offers a comparison of what’s widely experienced by women with Lipedema vs. what we usually see in normal fat or obesity.
Getting a proper diagnosis is both time-consuming and challenging. The lack of awareness both in the medical community and in society as a whole makes it difficult to know when it’s appropriate to seek medical attention. Even then, because of the lack of awareness, your doctor may not recognize the symptoms as Lipedema. They may not be aware of the disorder at all. To add insult to injury, if they do realize it, they may not be trained on how to diagnose it or what the next steps should be. It’s important to advocate for your health, know the signs and symptoms, and seek out expert guidance.
This disease is a subcutaneous fat storage disorder that is not widely recognized by the medical community (yet). This disorder mainly affects women, causes an enlargement of the legs due to deposits of fat under the skin, and typically gets worse over time, making diagnosis and treatment essential.
While there may be a genetic component to Lipedema, the exact cause is not yet known. And while other fat disorders can cause many of the symptoms mentioned here (such as Dercum’s and Madelung’s disease), the majority of the time, the result is almost always a Lipedema diagnosis. Today, we know that Lipedema leads to an excessive build-up of fat cells, primarily in the lower body (although it can affect the arms and abdomen), and it disproportionately creates pockets of fat. The negative appearance of these cells is compounded by the physical pain and sensitivity that comes along it. While patients are frustrated and discouraged by the negative appearance of their legs, chronic pain is what drives them to continue seeking answers.
Sufferers experience easy bruising and tenderness, and pain in the affected areas. Patients overwhelmingly report being misdiagnosed by their families and doctors as being obese. Unfortunately, Lipedema fat is far more stubborn than regular fat, and will not respond to diet or exercise. Those with this disorder may workout regularly and practice healthy and balanced nutrition but will continue to gain weight. Or worse, they experience weight loss as the normal fat is lost, yet the painful, Lipedema fat remains. Commonly, the lack of effectiveness from a regular diet and exercise program is what prompts patients to recognize something isn’t right in their bodies. Even still, patients are often at odds with their doctors and are provided with solutions that do not address their underlying condition, ongoing pain, and consistent frustration. Unfortunately, it’s not uncommon for individuals with Lipedema to have more awareness of the disease and its treatment than the doctors and nurses who they encounter in their search for diagnosis and treatment.
How common is lipedema? Find out here.
In 2019, I started training for a half-marathon and was running an average of 40 miles per week. During this time, I noticed that my upper body, arms, and face started to drop weight, but a strange fluid and fat mix around my thighs and knees just wouldn’t budge, no matter how healthy and active I was. My legs felt heavy and painful to move, and the only relief I found was wearing two pairs of workout pants to keep my legs as tight as possible. This was the turning point for me; How much more could I possibly do to get my body where it needed to be? After completing the half-marathon in April 2019, I started to aggressively look for answers. I was googling things like, “Why can’t I lose weight around my knees?” and “Why are my legs tender when I barely touch them?” I’ll never forget the moment I found a Reddit forum about Lipedema and how many are affected. This was the moment that changed my entire life.
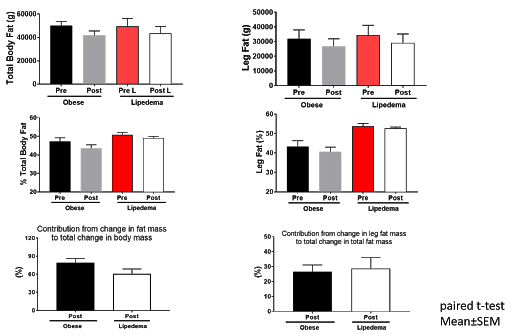
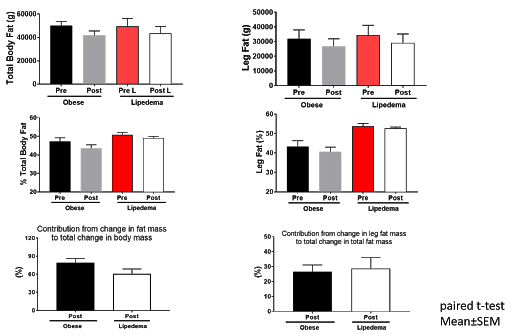
To further explore this frustrating aspect of Lipedema, a Washington University School of Medicine study evaluated the effect of diet-induced weight loss on body composition on both normally overweight patients and those who were overweight due to Lipedema. All participants were first properly diagnosed with Lipedema on their legs by ruling out other causes of legs swelling, such venous insufficiency. The study subjects received both a body composition scan with DEXA [Dual Absorption Xray] and an MRI to ensure an accurate baseline body composition evaluation. Each participant met with dietitians to create personalized healthy meal plans designed to achieve an 8-10% weight loss goal over the course of 6-8 months. All meals were prepared in the medical school metabolic kitchen and calories accurately counted. Afterward weight loss was achieved, each patient received the same body scan and MRI to determine how their body composition responded.
Each participant’s meal plan reduced their daily calories by 25% and included gluten, dairy, and egg-free meals as needed. They met with their dietitian weekly to record progress and pick-up food for the following week. The control group in this study went through the same process, however, they were diagnosed as obese and not with Lipedema, yet their BMI and age mirrored those in the Lipedema group.
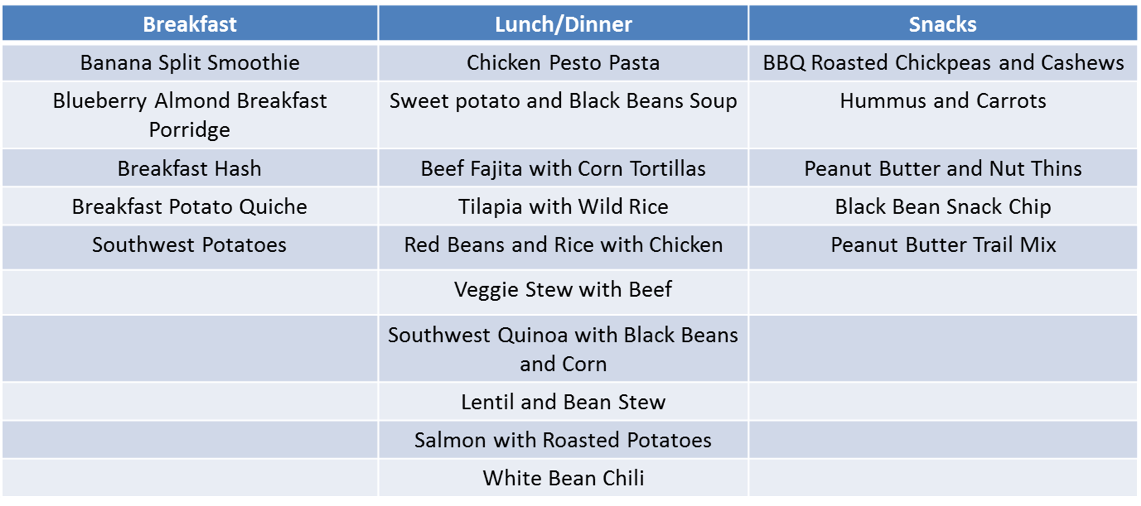
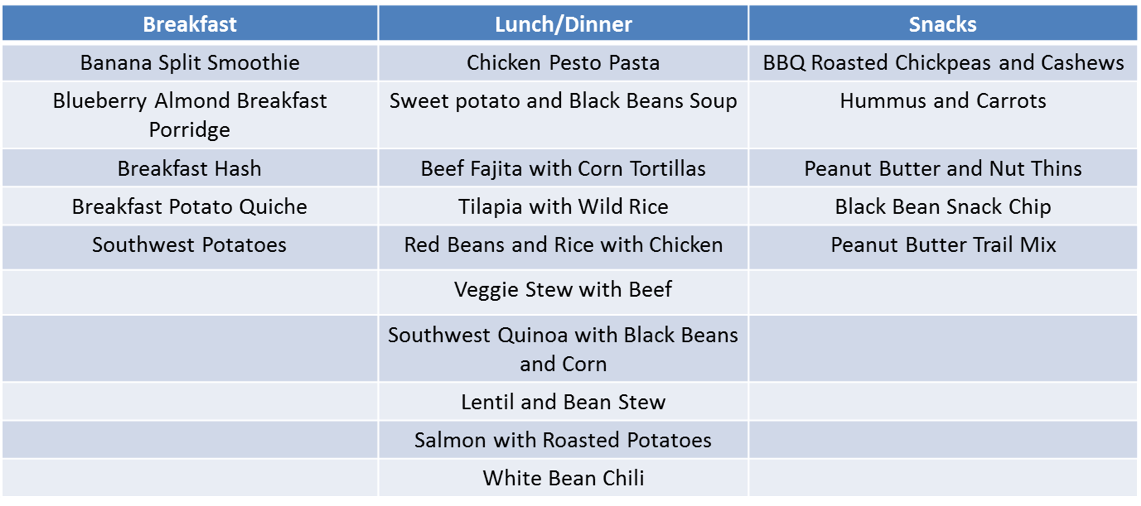
For those of us struggling with Lipedema, the results of the study come to no surprise. While the group who had Lipedema was able to lose weight and decrease their body fat percentage, the decrease in percent body fat was lower for individuals with lipedema than those with classic obesity. Additionally, the post-weight loss body composition scans showed that the participants with Lipedema did not experience a significant loss of fat in their legs. So, while they did lose weight, their legs remained mostly the same. Those with classic obesity experienced higher weight loss, a greater decrease in their percent of body fat, and significant weight loss in their legs. Please note these 10% weight loss results are hard to translate into the real world. Unfortunately, in the real world we don’t have the luxury of someone preparing all of meals, counting calories, and coaching us weekly or more if needed along the way.
The only way I can fully explain learning about Lipedema is to explain it like a lightning bolt. In an instant, every moment of frustration, embarrassment, physical and emotional pain, and shame from my doctors were replaced with clarity – everything made sense now. I no longer was ashamed that I couldn’t figure out how to get my body to look like everyone else’s. Even before I found a specialist, I felt hopeful and excited for the first time in my life. Maybe I wasn’t a failure, I wasn’t crazy, and I wasn’t obese. Maybe I wasn’t alone in my struggle, and I could find something that would actually help! Fast forward exactly one year, and I’ve had two surgeries on my thighs, with plans to get three more. My thighs are nearly pain-free, I can go for long walks without feeling heavy and swollen, and I can play with my dog without getting bruised from her jumps. I’m experiencing life like I haven’t ever before. And the better I feel, the more I’m recognizing how much pain I was in for my entire life.
If you think you might have Lipedema, the first step is to see a doctor for a diagnosis. You can read more about the physical exam and necessary tests to determine if your provider can help you through this here. An ongoing treatment plan should be discussed with a medical professional, but you can read more about surgical options here, and non-surgical ways to live with Lipedema here. While there’s no cure for this disorder, a diagnosis is the first step to better understanding your body and, most importantly, that this is not your fault. The answer to your question, “Why are my legs so different?” is not that it runs in the family or that you aren’t doing your best. The answer is that you have Lipedema, and we’re here to help you through it.
When it comes to lipedema, there are plenty of unfortunate stories regarding individuals looking for a proper diagnosis who are told they are only obese. There is a clear difference between regular fat and lipedema body fat tissue that accumulates with lipedema that can be observed by the trained eye. Lipedema is associated with a buildup of subcutaneous adipose fat tissue; adipose tissue is used for long term energy storage. Our organs, such as the liver and kidneys, require fat tissue for proper metabolic functioning. Another form of adipose fat tissue, called visceral fat, is very active and is sensitive to calorie balance changes. The third type of adipose fat tissue is called subcutaneous fat tissue and is found between your skin and muscle tissue. This fat tissue is not sensitive to metabolic changes. Even less active in regards to metabolism is hormone-dependent subcutaneous fat tissue that develops in females around the age of puberty. It provides the female body’s shape and is influenced by estrogen and progesterone.
As mentioned, untrained doctors may not recognize your condition as lipedema and instead think it is simply obesity. Individuals with lipedema are able to lose overall weight and decrease the total fat percentage in the body. However, this change is significantly less than in those who are simply obese. The difference in weight loss is statistically different between those with and without lipedema. For example, fat tissue found in the leg will not significantly decrease with diet and exercise in those with lipedema as opposed to someone with obesity.
Another difference between individuals with lipedema and those who are obese is the level of plasma glucose. Individuals with lipedema have a slightly lower fasting blood sugar level than those with identical BMI obesity. In addition, patients diagnosed with lipedema have lower blood sugars after consuming high glucose drinks than those with matched BMI obesity. The blood sugar difference only increases as weight loss is slowly achieved.
Lipedema is associated with the hormone-dependent subcutaneous fat tissue. This greatly impact the arms and legs and can spread further through the body. It is currently unknown why it impacts certain areas of the body and not others. This type of fat tissue is almost nonresponsive to weight management. Other fat deposits in the body will be impacted by weight loss instead of the hormone-dependent subcutaneous fat tissue in the body.