Fall has arrived and with the cold weather looming you may be wondering what you can eat that can be both fulfilling and anti-inflammatory for your lipedema care. It’s easy to learn what you should and shouldn’t eat but sometimes hard to stick to it without the background knowledge of why. Knowing the why can help you make the best decisions for yourself and maybe incorporate some things that you may not have thought of before.
It is recommended to follow the RAD diet (or Rare Adipose Disorder diet). The RAD diet is basically a modified Mediterranean diet that helps maintain a low glycemic index. The goal is to keep your insulin levels low by avoiding refined or processed starches and sugars that are found in pasta, rice, bread, corn, and potatoes. Avoiding processed carbs and processed food, in general, will help keep your inflammation at bay and in turn reduce your lipedema symptoms. Along with reducing starches, avoiding gluten(found in wheat, rye, and barley) all together may be necessary to limit flare-ups.
For a healthy lipedema care meal plan, you will want a nutrition plan that is high in omega 3’s. Mainstream health organizations recommend a minimum of 250-300 mg of omega-3s per day, the FDA recommends not to exceed 3000 mg of omega-3, but European Food Safety Authority (EFSA) says up to 5000 mg of omega-3s per day is safe.
Omega-3s reduce the production of some substances (eicosanoids and cytokines) released during an inflammatory response in the body, reducing inflammation will help reduce lipedema flare-ups. Some added bonuses of increasing your omega-3 consumption are; it may help fight auto-immune diseases, decrease symptoms of anxiety and depression, improve eye health, promote brain health during pregnancy, improve risk factors of heart disease, reduce symptoms of metabolic syndrome, improve mental disorders, fight age-related mental decline, reduce fat in your liver, improve bone and joint health, alleviate menstrual pain, and improve sleep.


Obviously incorporating more omega-3s into your diet will reduce inflammation and other symptoms that may arise from lipedema but what foods and supplements are best? Fish is high in omega-3s such as Mackerel (4,107mg per serving), salmon (4,123 mg per serving), herring (946mg per serving), oysters (370mg per serving-about 6 raw oysters), sardines(2,205mg per serving), anchovies(951 mg per serving), caviar(1,086 mg per serving). Now if you’re not crazy about fish, there are other options, flaxseeds, chia seeds, walnuts, and soybeans all have a similar amount of omega-3s per serving to their fish counterparts.
**It should be noted that soybeans are high in omega-6s which can cause inflammation so you may want to leave the soybeans out of your diet.
Along with omega-3s, there should be a heavy focus on fiber in your diet plan. It is recommended that men get 38 grams of fiber a day and women 25 grams of fiber per day. Fiber can be split into soluble fiber(metabolized by good bacteria in the gut, water-soluble) and insoluble fiber(does not dissolve in water). Fiber feeds the good gut bacteria and works with our bodies in symbiosis by breaking down what we cannot on our own. By consuming fiber, we are feeding our gut bacteria “prebiotics” which the bacteria break down to produce necessary nutrients, short-chain fatty acids. Short-chain fatty acids feed the cells in the colon which can reduce gut inflammation. Fiber is also a necessary element to help you feel full and stay full longer! Also, it slows down digestion by absorbing water and in turn, increases the number of vitamins and nutrients the body can absorb.
Omega-3s and fiber are incredibly important to reduce lipedema inflammation but what does that mean for what you should eat? Think of the standard food pyramid, instead of the high consumption of grains, it’s recommended to consume high levels of low-carb vegetables, herbs, and spices, such as cabbage, eggplant, carrots, cauliflower, Bok choy, peppers, broccoli, cucumbers, asparagus, etc. Here are some herbs for an extra boost of anti-inflammatory action: ginger, garlic, turmeric(with black pepper for absorption), cardamom, green tea, rosemary, and cinnamon.


Next on the pyramid, you should consume a smaller amount of healthy fats like nuts- Peanuts, almonds, Brazil nuts, macadamia nuts, hazelnuts, pecans, avocados, coconut oil, and olive oil. Brazil nuts in particular have a large amount of selenium, a necessary nutrient that helps reduce the painful swelling that lipedema causes. It should be noted that only two brazil nuts a day can make a difference!
The next part of our pyramid is healthy protein. We’ve touched on a few fish for your omega-3s but you could also include eggs, chicken, turkey, tofu, shrimp, and tuna. Protein is another important component to help you feel full and stay full longer which helps reduce cravings.


Lastly, we have lower-carb fruits, beans and legumes, and moderate-carb vegetables. Some lower-carb fruits include berries, melons, kiwis, mangos, and raisins. It is best to try to eat the rainbow! Each color has different nutrients and antioxidants necessary for a long-term healthy body and it’s much easier to track the colors you’re eating versus every nutrient each fruit/vegetable has in it.
Patients with lipedema often have low levels of vitamin D3 so supplementing with four times the daily recommended dose of vitamin D is helpful along with Diosmin, and selenium if you are not able to eat brazil nuts. Fish and krill oil are great supplements to take on days you are not consuming high amounts of omega-3s
Now that we’ve covered food, what else can you do to keep lipedema symptoms aways? There are multiple ways to keep your lymphatic fluids flowing such as yoga, dry brushing, massage, and compression garments.


Yoga is all around great for your whole body by lengthening, strengthening, and deep breathing, it can improve your health and mental wellbeing. Lymphatic yoga is even better for lipedema! Lymphatic Yoga can help move the stagnant fluid in the lymph system through the body and to the heart. Dynamic yoga such as sun salutations is great because it keeps you moving from one pose to another and encourages the movement of fluids. Any inversion poses and backbends will help fight gravity that keeps fluids in the lower part of your body from moving to the upper parts. Twists help with stimulating organs and stretching the spine.


The lymphatic system lies just below the surface of the skin so dry brushing has been shown to stimulate the lymph system and help move venous blood. Dry brushing should be done with long firm strokes towards the heart. Start from your feet to the legs and groin and then hand to your armpits. An added bonus is your skin will be exfoliated and feel amazing!
Lymphatic massage is a great way to reduce swelling and improve lymphatic circulation. You can go to a professional massage therapist who specializes in lymphatic massage or you can learn how to do it on yourself at home! When performing these techniques you should make sure you are relaxed, don’t perform this if it is too painful, and it should only affect your skin, so deep pressure is not needed.


Start by connecting to your deep breaths, slowly inhaling from your nose and out through the mouth. Try to make these breaths as long as possible with a pause between each breath. Like the dry brushing, you start from your feet and pull the skin up towards your heart with light pressure, so the skin stretches. Continue this all around the ankles, then calves and thighs.
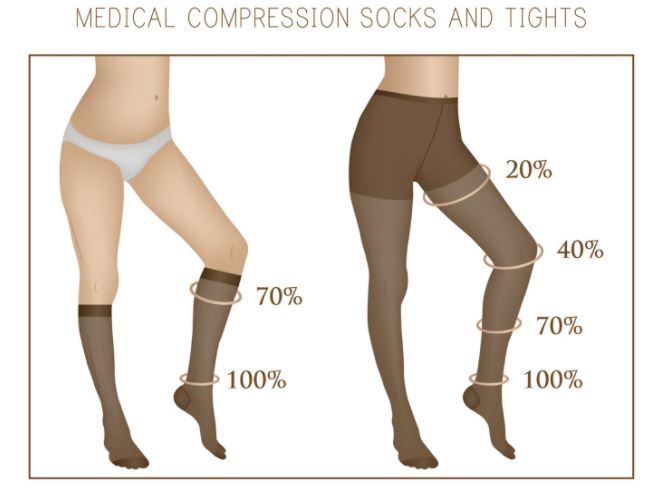
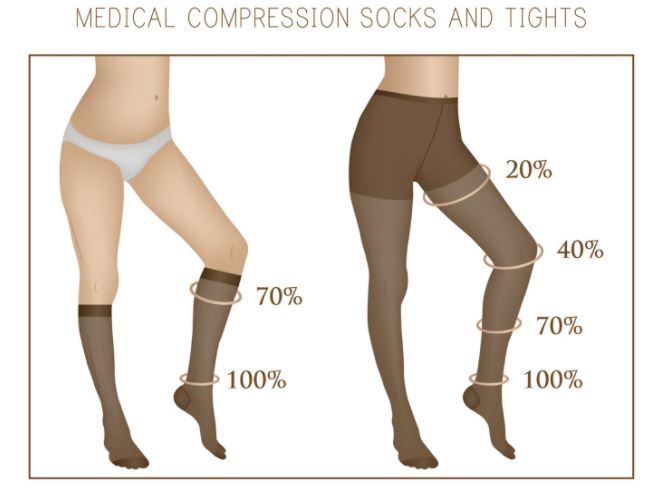
Last but not least, you can use compression garments! Luckily it will be getting colder so it won’t feel so hot and restricting to adding in an extra layer of clothes. It is best to use medical-grade garments because fluid flows from higher pressure to lower pressure and medical-grade compression garments have graduated compression. The compression at the lower part of the garment will force lymphatic fluid from the lower part of your body up through your body back towards your heart. Again, we’re fighting gravity so compression garments will need to be tighter for the legs versus your arms.
Now you have all the options to keep your lipedema symptoms low over the winter months, from eating the rainbow to yoga, massage, and compression garments. It’s a difficult disease to battle but you’re not alone, and now you have a few extra tools that can help you along the way. Contact us today!
As of May 28, 2021, Dr. Wright and nearly two dozen other Lipedema experts led by Dr. Karen Herbst published 85 consensus statements making up the first ever Standard of Care Guidelines for Lipedema in the United States. Prior to it’s publication, other countries such as Germany, Spain, the United Kingdom and The Netherlands have documented and published Standards of Care for women with Lipedema, but the United States continued to lag behind it’s international colleagues. Ultimately, this resulted in American women with Lipedema being underdiagnosed, misdiagnosed, dismissed, and underserved. This publication is the first of many steps in the right direction to increasing awareness and proper treatment for women with this disease.


A standard Lipedema care typically refers to the formal guidelines that are generally accepted in the medical community for the treatment of a specific disease, condition, or ailment of some kind. These guidelines include important information including how to properly recognize and diagnose the condition in question, followed by the treatment process a medical provider should follow for patients with symptoms of the medical issue. The standard of care provides “best practices” developed by experts in the field who have come to a consensus of what is the most appropriate way to treat the condition at hand.
The importance of having a standard of Lipedema care in place can be best understood by highlighting what happens when a standard is not in place, as we’ve seen in Lipedema prior to today. Clinical practice guidelines are compiled by the National Guideline Clearinghouse, which provides medical providers the ability to stay up-to-date on what the standard of care is in areas of treatment. When Lipedema is not included in these national guidelines, there are no resources for physicians to refer to.
Without guidelines to the disease, symptoms checklists, or treatment plans, medical providers are unlikely to understand the disease or recognize it when they see it in their patients. Most women with Lipedema discover the disease on their own and bring it to their doctor to discuss a report being dismissed by their providers, who are unaware of the disease and have no medical expert guides as resources to refer to. This publication is a very important and exciting step to ending this cycle.
An estimated 11% of the world’s female population, and 16 million women in the United States alone, are affected by Lipedema, a chronic, progressive, and disruptive fat disorder. Also referred to as Lipoedema in European countries, this disorder has a variety of symptoms, ranging from generally irritating to aggressively painful. Patients suffer from swollen, sensitive areas, unsightly, bulging and indented skin, and a disproportionately larger lower body. Without answers or solutions, patients often also suffer from secondary obesity. By the time they make it to a Lipedema specialist, they report similar stories; their primary doctors had not heard of Lipedema or dismissed it as unfounded. These medical professionals’ lack of knowledge leads to improper diagnoses such as general obesity, prescribing diet and exercise as a cure, and sometimes extraordinarily invasive and dangerous weight-loss surgeries. The journey towards diagnosis and treatment takes both a mental and physical toll of those it touches, a problem that the Standard of Lipedema Care guidelines seek to alleviate.


The Standard of Care for Lipedema guideline explains the following in far greater depth and should be the go-to resource for everyone in the Lipedema community, from providers to patients and their families. Below are only a few examples of action items provided, and the full standard should be consulted here for a comprehensive guide to understanding Lipedema, diagnosing it, and treating it across patients.
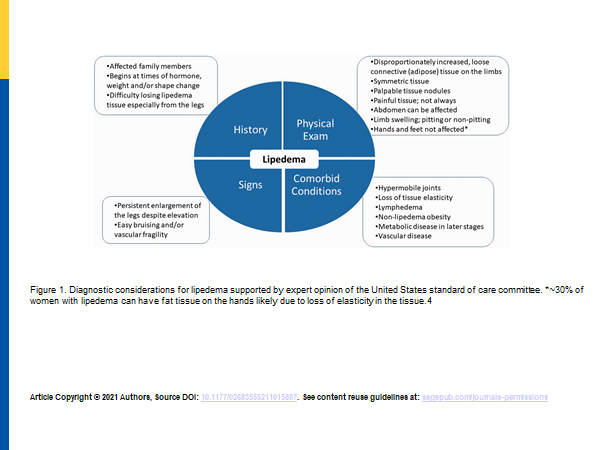
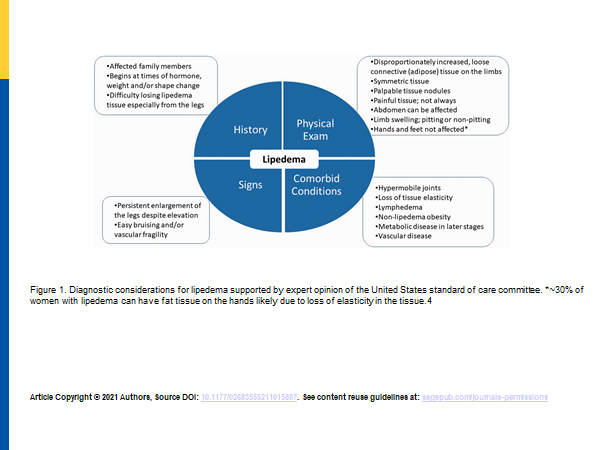
TABLE 1: Classification of lipedema severity according to Stößenreuther (2001).
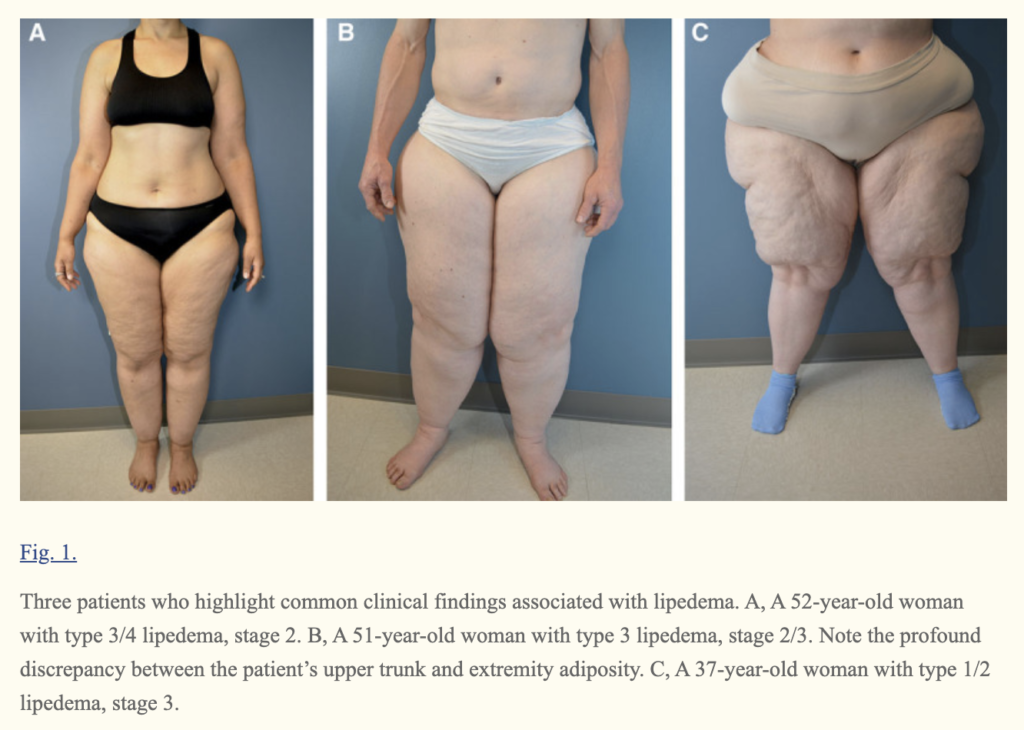
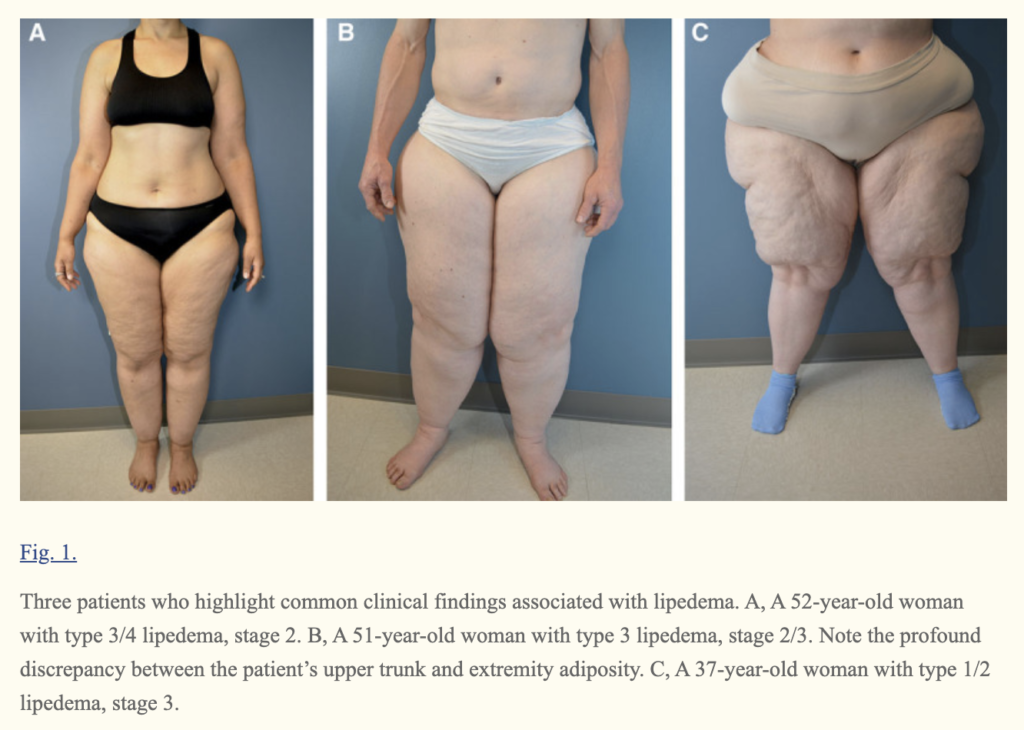
| STAGE | SKIN SURFACE | SUBCUTANEOUS ADIPOSE TISSUE |
| STAGE 1 | NORMAL | SMALL NODULES |
| STAGE 2 | UNEVEN | BIGGER NODULES |
| STAGE 3 | LOBULAR DEFORMATION | LARGE NODULES & DEFORMITIES |
TABLE 2: Types of lipedema, used to describe the location of lipedema fat
| TYPE | LOCATION |
| TYPE I | BUTTOCKS, HIPS (“SADDLEBAGS”) |
| TYPE II | BUTTOCKS TO KNEES, WITH FOLDS OF FAT AROUND THE INNER KNEE |
| TYPE III | BUTTOCKS TO ANKLES |
| TYPE IV | ARMS |
| TYPE V | LOWER LEGS |
Common complications of lipedema including lymphedema non lipedema obesity venous disease and hypermobile joints were described.
Put Criteria for EDS hs . Beighton Criteria.
Table 2: Beighton’s joint hypermobility score.
| The ability to | Right | Left | |
| (1) Passively dorsiflex the fifth metacarpophalangeal joint to ≥90◦ | 1 | 1 | |
| (2) Oppose the thumb to the volar aspect of the ipsilateral forearm | 1 | 1 | |
| (3) Hyperextend the elbow to ≥10◦ | 1 | 1 | |
| (4) Hyperextend the knee to ≥10◦ | 1 | 1 | |
| (5) Place hands flat on the floor without bending the knees | 1 | ||
| Total possible score | 9 |
One point can be gained for each side for maneuvers 1–4 so that the hypermobility score will have a maximum of 9 points if all are positive. (12) 12. Vounotrypidis P, Efremidou E, Zezos P, et al. Prevalence of joint hypermobility and patterns of articular manifestations in patients with inflammatory bowel disease. Gastroenterol Res Pract. 2009;2009:924138. doi:10.1155/2009/92413
References:
Standard of care for lipedema in the United States
https://pubmed.ncbi.nlm.nih.gov/