An estimated 17 million women in the U.S. and nearly 370 million women across the globe suffer from a condition known as Lipedema. What is regularly associated with rapid and uncontrollable weight gain in its initial stages can spiral out of control if left undiagnosed. As experts continue researching the causes and best treatment options for women with Lipedema, tumescent liposuction or lipedema reduction surgery remains the only way to reset the progressive disease and provide women with increased mobility and reprieve from daily pain.


Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Lipedema is often misdiagnosed and dismissed by medical professionals as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
Women suffering from Lipedema often report the disease associated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.


Ultimately, effective treatment will require surgical intervention to alleviate the appearance and pain of symptoms. Liposuction performed on the affected limbs is generally the most effective treatment. Removing fat deposits that are diseased helps reduce swelling of the limbs and alleviates the pain that holds patients back from everyday activities.
This surgical treatment can provide a variety of benefits and relieve the symptoms you are experiencing from lipedema. Dealing with lipedema can be difficult, especially if you are just now starting to take control of it.
Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the growth of more fat cells, which can overwhelm the lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and making an already stressed system worse. Using blunt cannulas and generous and special surgical techniques, studies have shown that lymphatic function can improve after this type of liposuction in women with Lipedema. The goal of lipedema reduction surgery is to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a “debulking” surgery, not a cosmetic surgery.Why is Lymph Sparing Liposuction Preferred for Lipedema Patients?
One of the most beneficial aspects of lymph-sparing liposuction is that the treatment does not rely on general anesthesia. While general anesthesia is used for various treatments, it is generally not recommended for individuals with lipedema. Instead, lymph-sparing liposuction uses tumescent anesthesia to avoid these unwanted complications. General anesthesia can cause severe complications and even death in up to 0.3% of liposuction treatments. Relying on tumescent anesthesia ensures the anesthetic fluid has been distributed throughout the tissue, and it has had time for all the fat tissue to gel. Patients are conscious for the duration of treatment, while the tumescent liquid acts as a local anesthetic to the treatment area. Patients may take pain pills ahead of time to help with discomfort and sometimes use laughing gas. However, through the process, patients feel little pain and, if anything, pressure in the area being treated.


Perhaps the most noticeable benefit to lymph-sparing liposuction is how it can reduce the amount of subcutaneous fat tissue in the body. Lipedema reduction surgery not only significantly reduces fat tissue but also removes fibrous tissue, making the limbs lighter, smaller, less tender, and smoother. Following your physician’s guidelines is critical to reduce swelling and inflammation before the treatment. This is done by wearing compression garments and wraps along with receiving manual lymph drainage for several weeks following lipedema surgery and beyond. Patients wear medical-grade compression clothing for at least eight weeks, and manual lymph drainage and massage are typically recommended as an ongoing and regular treatment.
Your tissue will be decongested, allowing your liposuction treatment to be as successful as possible. Some slight swelling and bruising may return immediately following the procedure, but this is expected and should subside over time. Some patients also report numbness as their nerves in the treated areas respond to treatment. Numbness may last for several months and up to one year, but compared to the reduction in fat tissue, patients still see this as a huge improvement. Compression is critical to be maintained after the lipedema surgery as well, as the lymphatics are re-established. The lymphatic function is often improved.
By reducing the amount of subcutaneous fat tissue, you can reduce any pain associated with lipedema. Lipedema reduction surgery, which is sometimes referred to as Lymph sparing liposuction, will be able to help you increase mobility without having the pain you have been feeling with lipedema since it started. This is huge for women with lipedema, especially because the pain and bruising is the leading symptom of seeking treatment. Women report a significant improvement in their ability to move around more freely, exercise more regularly, and enjoy day-to-day activities that were previously off-limits. Bumping into a chair or a corner no longer causes large bruises, playing with the family dog doesn’t cause pain when they jump, and everyday activities are no longer considered out of reach.
Significant blood loss is the most commonly reported side effect of lipedema surgery. Women with lipedema very often have large varicosities and studies have shown enlarged networks of veins in the legs of women with lipedema. Liposuction can cause significant blood loss if these veins are not treated before surgery. Even with proper preoperative treatment of dilated and varicose veins and good tumescent technique in women with lipedema, if the surgery is large enough, there can still be significant blood loss. In some cases even a blood transfusion has been needed in the postoperative period. The next most common complication of lipedema reduction surgery or lipedema liposuction is blood clots. Women with lipedema are, on average, heavier than women without lipedema making the risk of blood clots with the surgery greater. The risk of blood clots and other thrombotic complications can be greatly reduced with postoperative blood thinners. Careful surgeons should risk stratify their patients for possible blood clot complications and put them on prophylactic postoperative blood thinners. Infection is always a risk of any surgery including lipedema surgery. There has been a report of fat embolism with lipedema surgery. Death has to be included as a possible outcome. We are not aware of any deaths from lipedema surgery, but of course it is possible that any surgery can, in very rare circumstances, result in death. Finally, lymphatic injury is a real risk of liposuction and is a special concern for women with lipedema. Smaller cannulas are also used to keep down the risk of trauma to the body and an already compromised lymphatic system. With care and proper surgical technique lymphatic injury need not occur. In fact in skilled surgical hands lipedema reduction surgery may actually improve lymphatic function.
While the recovery can get painful, especially in more heavily used areas such as the arms and calves, patients will report that the payoff is well worth it. Lipedema fat more often accumulates around the lower body, including the thighs and buttocks. Women will often see the majority of their Lipedema fat in these areas. However, they can also commonly find Lipedema fat accumulation around the inner knee and backside of their leg. After the removal of lipedema tissue in these areas, patients are not only more mobile and can get around more easily, but they experience far less pain in their daily lives.


This procedure allows for a more active and healthy lifestyle, which many patients have experienced for years (and in some instances, it’s been decades). If paired with proper compression therapy, a healthy diet, tons of water for hydration, and responsible maintenance, women with lipedema are afforded a much higher quality of life and more enjoyable day-to-day. The reduction of irregular and heavy fat can improve joint function, making everyday tasks such as walking, climbing stairs, tying shoes, or even getting up from a chair much easier than before. Normal tasks that many take for granted are daunting and painful for women with lipedema, and lymph-sparing liposuction can help reset the clock by several years to help.
While lymph-sparing liposuction for lipedema is generally safe in healthy individuals, risks such as infection, bleeding, and trauma to the area may occur. Post-operative swelling in the limbs after surgery, which occurs with any liposuction procedure, is more prolonged in individuals with lipedema. The swelling typically worsens for a few months before it gets better, and the full benefit may not be realized for six months to a year. However, overall, most patients with lipedema experience significant improvement of many or all of their symptoms, with varying individual results. It’s not uncommon for Dr. Wright and his team to complete the procedure, and their patient notices a change before they leave the office, especially when large amounts of fat tissue are removed.
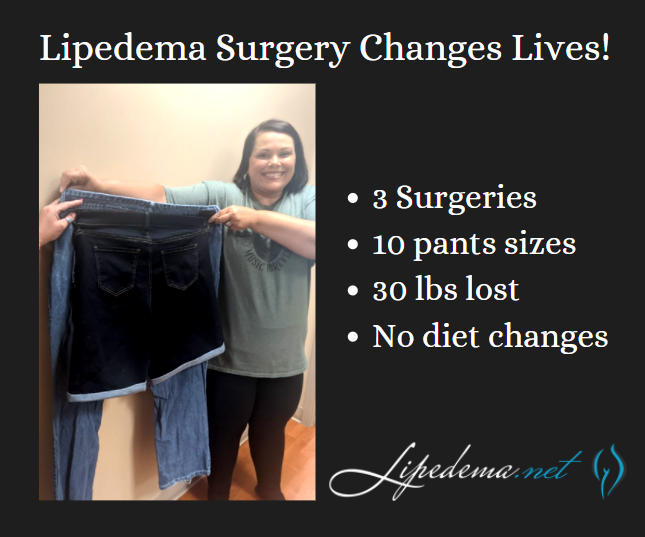
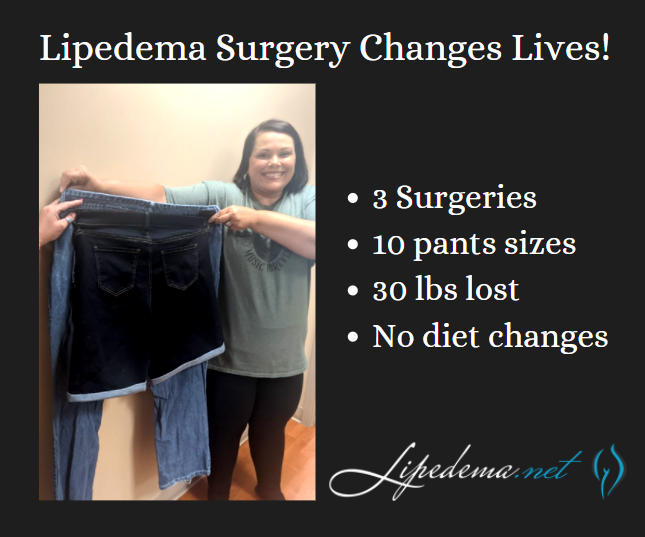
Although some people who have lipedema in one specific area may need only one procedure, most people undergo multiple lymph-sparing liposuction procedures to address all the different areas affected by lipedema. The multiple liposuction procedures must be staged or separated to be done safely. The timing of the procedures depends on multiple factors, including the clinical stage of lipedema in the patient, the amount of fat being removed, the patient’s health and mobility, and other logistical factors. Generally, each procedure should be spaced out by at least three months to allow for proper recovery.
After the lipedema surgery, patients go home the same day but should be sent home already in their compression garments. The first afternoon after surgery should be spent resting, and it’s likely patients are extremely drowsy from the procedure and medications. The following day post-op check-in should be completed before returning home. Patients will be sore and will continue to experience drainage of tumescent fluids. Padding around the incision points is required for several weeks. Compression garments are worn around the lock for the first several weeks, then worn during the daytime hours only before eventually tapering off after 12 weeks.
As you can see, lymph-sparing liposuction has plenty of exciting benefits. This procedure can make living easier with unwanted symptoms such as difficulty with mobility, pain, and tenderness. Physicians like Dr. Wright can provide you with the needed treatment to reduce your lipedema symptoms. Contact us today!
Before tackling the issues and symptoms associated with lipedema, it is important to assess your vein health by working closely with a vein specialist. Vein issues and lipedema, both can cause painful, heavy legs, and tenderness, so it can be difficult to know if your symptoms are related to veins or solely to lipedema. An experienced vein specialist can get you on the right path to a diagnosis and treatment plan.
Many women with lipedema require lifelong use of compression garments, so the advantages of treating vein issues are somewhat limited. Plus, unfortunately, edema in the legs of lipedema patients generally does not significantly improve after vein treatment. However, lipedema reduction surgery can at least temporarily treat venous insufficiency. Vein issues and issues with the lymphatic system are connected.


Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. Sufferers living with lipedema experience easy bruising and tenderness, pain in the affected areas, and significant disability in daily life. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back. Little is known about the disorder, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema reduction surgery is a spin-off of liposuction focused on the reduction of lipedema tissues including fibrous tissue, fat, and extracellular contents. It is possible for lymphatics to be injured by a suction cannula during lipedema reduction surgery and/or cosmetic liposuction. Some argue whether this is possible, but studies show it can, and unfortunately, may happen for some. So, it is important if you have lipedema, or suspect you may have lipedema that you get a proper diagnosis and work closely with skilled surgeons well-versed in lipedema, lymphatics and lymphedema for the best possible outcomes and treatment plan before you proceed with any type of liposuction.
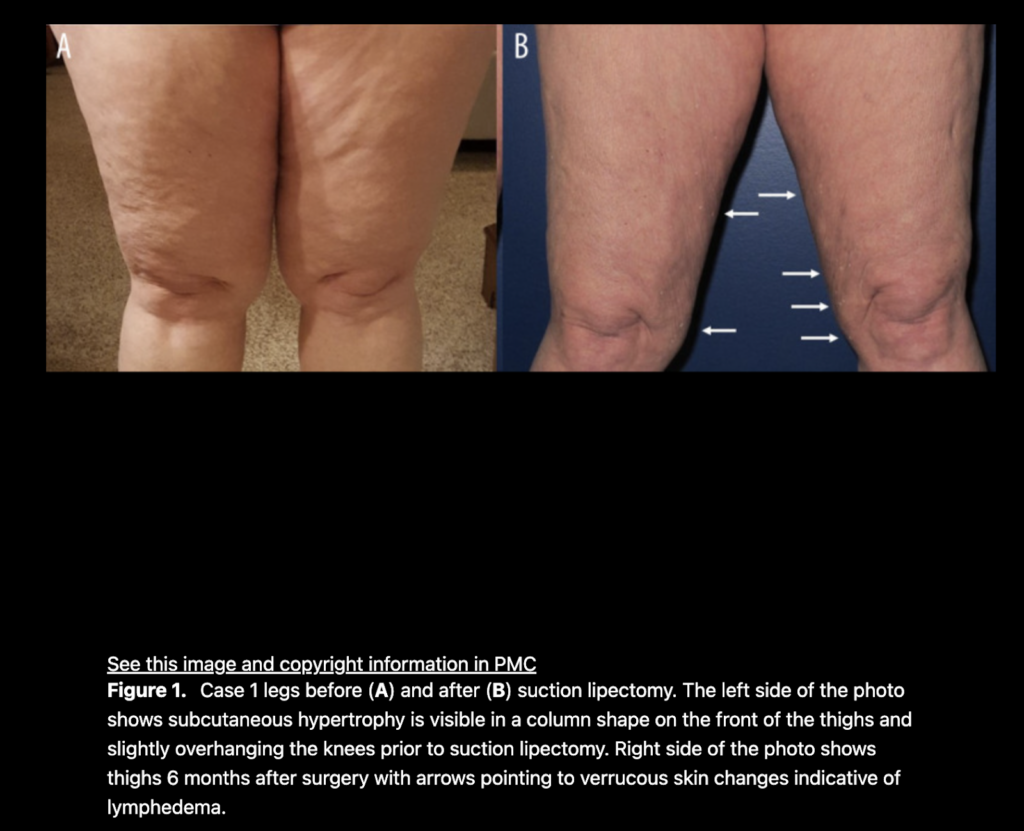
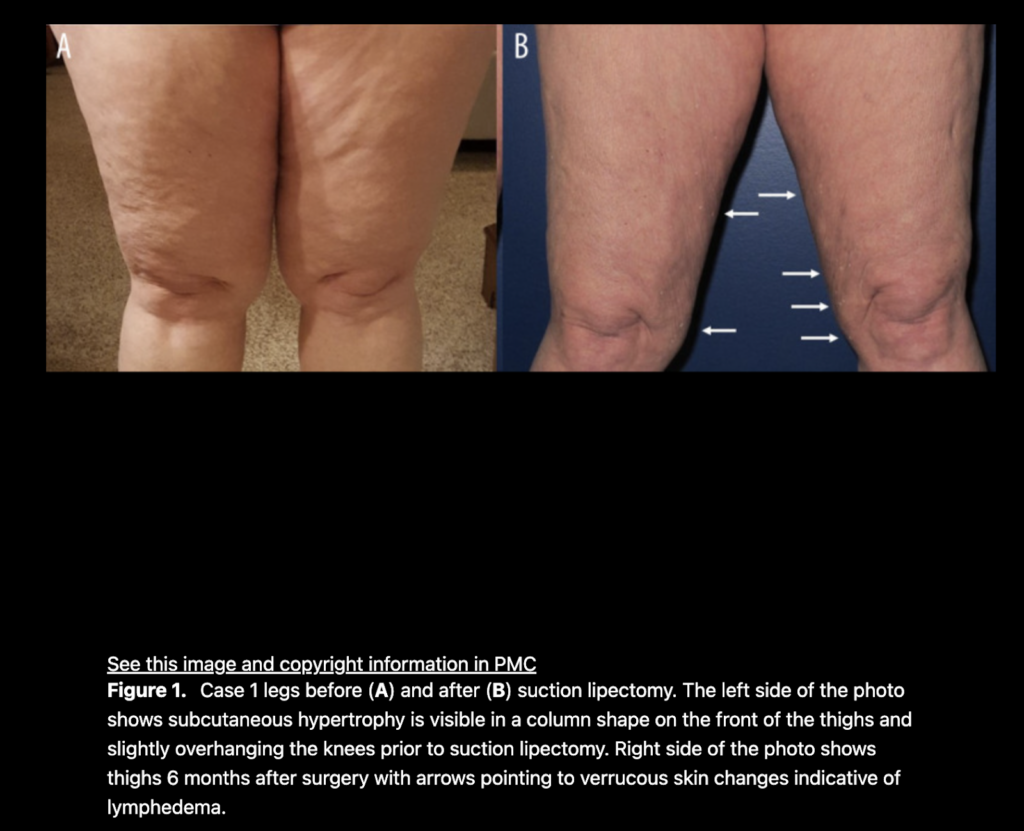
According to a study by Wright and Herbst, in patients with normal lymphatic function, and no severe injury to the lymphatic collectors, the lymphatic system almost always recovers and returns to a normal state. Suction lipectomy with small blunt cannulas and surgical techniques that focus on avoiding lymphatic damage have been reported to halt lipedema progression. A modification of suction lipectomy can result in alleviating or at least improving the swelling, leg heaviness and fatigue, the need for limb compression, and the need for lymphatic massage in women with lipedema. In patients with an impaired lymphatic function such as chronic lymphedema (or lipedema), careful suction lipectomy using techniques to avoid lymphatic injury can result in improved lymphatic function and a decreased rate of secondary infection or cellulitis in the affected limbs.
There are well-documented changes in the lymphatics of women with lipedema. The lymphatics are dilated and tortuous. Here are the differences between lipedema and lymphedema:
Protective measures to lessen risk of lymphatic injury include:
The short answer is this issue is hard to study as it is not possible to examine on live patients. There is one study by Hoffman which showed a longitudinal cannula technique and tumescent solution caused less injury to the lymphatics post-mortem. There is some evidence that the preoperative mapping of venous and lymphatic structures can lower the risk of lymphatic injury. While there is clear evidence lymphatic injury can occur, there is no definitive proof of what surgical techniques can prevent lymphatic injury from liposuction or lipedema reduction surgery. Lymphatic injury complications are poorly recognized after suction lipectomy surgeries and therefore are less likely to be reported in the literature for both lymphedema and lipedema.
—
References
Crescenzi R, Marton A, Donahue PMC, Tissue sodium content is elevated in the skin and subcutaneous adipose tissue in women with lipedema: Obesity (Silver Spring), 2018; 26(2); 310-17.
Hoffmann JN, Fertmann JP, Baumeister RG, Putz R, Frick A. Tumescent and dry liposuction of lower extremities: differences in lymph vessel injury. Plast Reconstr Surg. 2004 Feb;113(2):718-24; discussion 725-6. doi: 10.1097/01.PRS.0000101506.84361.C9. PMID: 14758241.
Iker E, Mayfield CK, Gould DJ, Patel KM, Characterizing lower extremity lymphedema and lipedema with cutaneous ultrasonography and an objective computer-assisted measurement of dermal echogenicity: Lymphat Res Biol, 2019; 7(10); 525-30.
Peprah K, MacDougall D: Liposuction for the treatment of lipedema: A review of clinical effectiveness and guidelines, 2019, Ottawa (ON), Canadian Agency for Drugs and Technologies in Health.
Rasmussen 2022. Lymphatic function and anatomy in early stages of lipedema
It also well reported that higher stages of lipedema are associated with impaired lymphatic functioning. ,7–9].
The Diagnosis and Treatment of Peripheral Lymphedema: 2016 Consensus Document of the International Society of Lymphology: Lymphology, 2016; 49(4); 170-84.
Wright TF, Herbst KL. A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema. Am J Case Rep. 2022 Jul 11;23:e935016. doi: 10.12659/AJCR.935016. PMID: 35811389; PMCID: PMC9284075.\
Chronic Venous Insufficiency (CVI)
June is Lipedema Awareness month, one in which the Lipedema community focuses (even more than usual) on how to reach women who have lived with this painful and distressing disease. While we’ve seen great strides in awareness, insurance coverage, and slightly greater recognition of this disease in the medical community, we continue to fight an uphill battle as women are underdiagnosed or completely dismissed when discussing their struggles and side effects with their providers. As a result, our team has put together some of the most important and impactful information for all of you, and we’re kicking off the month with a webinar from a team of lipedema experts.
Join us on Tuesday, June 7th, 2022 at 8 pm ET to listen to our panel discuss Recognizing Lipedema and Treatment Options. This is a FREE event!
Register here, or listen to the recording following the webinar at tactilemedical.com/education.
Drs. Steve Dean, Thomas Wright, and Tony Gasparis with Julie Green, OTR/L CLT-LANA, WCC, CLWT discuss lipedema – the pathophysiology, association with vein disease, conservative treatments, and surgical options available for patients.


Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the collection of fat cells, which can cause the obstruction of lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and making an already stressed system worse. Using blunt cannulas generous and special surgical techniques, studies have shown that lymphatic function can actually improve after this type of liposuction in women with Lipedema. The goal of lipedema reduction surgery is to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a debulking surgery, not a cosmetic surgery.
There are two specialized liposuction techniques that have been shown in studies to benefit individuals with lipedema: water-assisted and tumescent liposuction. In addition to the surgical equipment used, it is important to choose a surgeon with experience and one that is cautious when performing lipedema surgery. These factors can have an important influence on protecting lymphatic flow and function.
Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.


Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper Lipedema diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
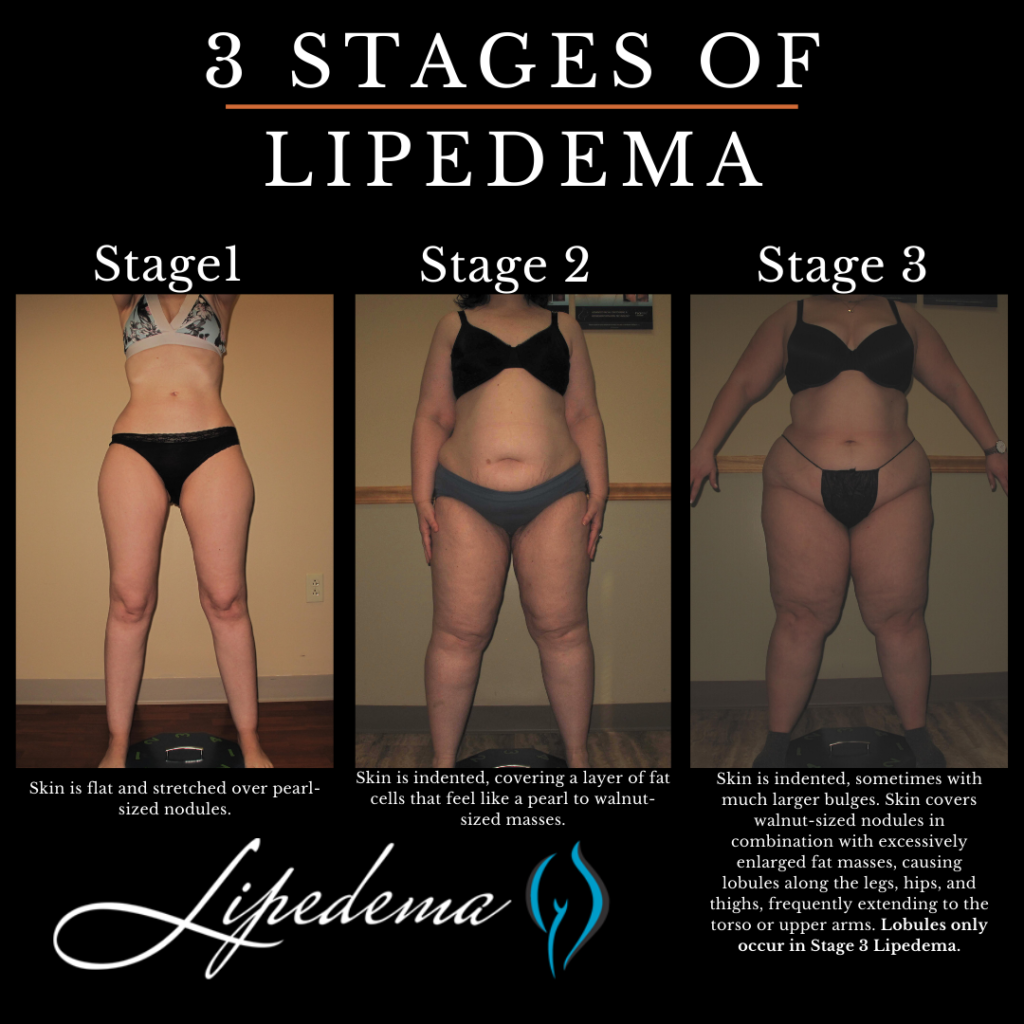
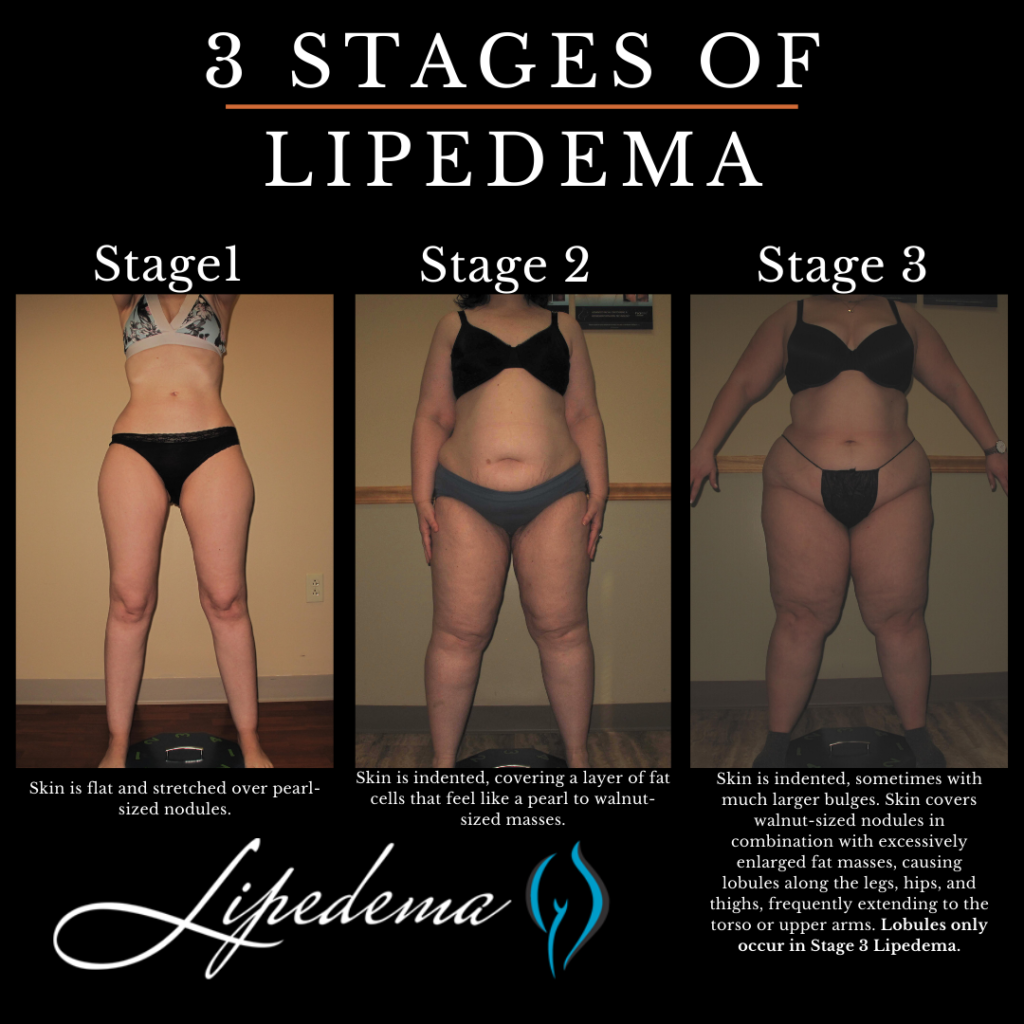
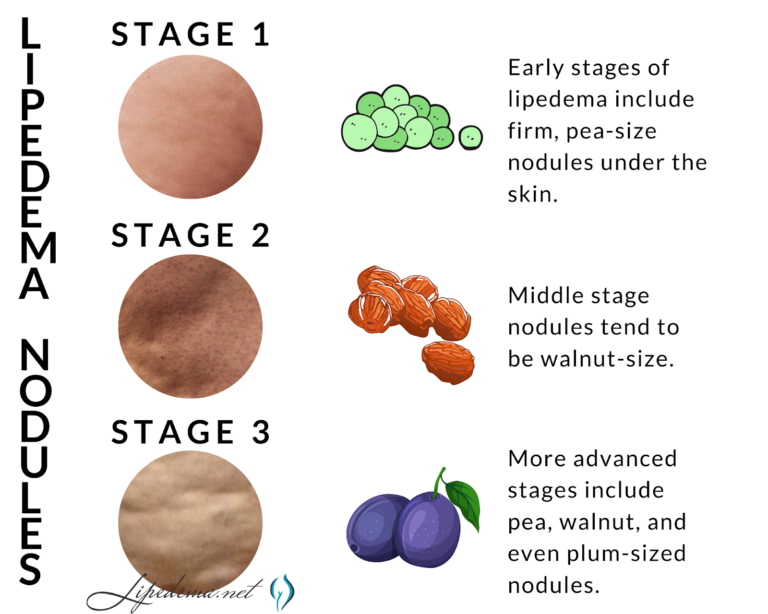
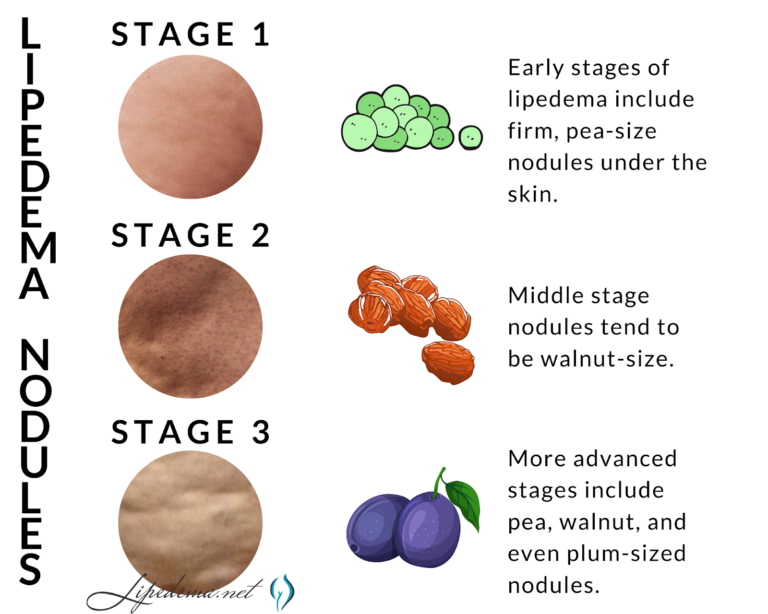
Overall, Lipedema appears in a series of three stages. Do any of these sound like you?
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.


| Photo credit: Linda Anne Kahn at Integrative Treatment of Lipedema |
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them.
When is the best time to get lipedema surgery?
There are two categories of treatment, surgical and non-surgical. Insurance providers require patients first try non-surgical treatment options before they’ll consider approving lipedema surgery, and Lipedema providers should be able to walk patients through this. While Lymph-sparing liposuction is the only treatment option that can provide permanent results by removing the lipedema fat, non-surgical options can help slow progression and are also necessary post-surgery (so it’s still important to practice them!).
To the dismay of patients, wearing medical-grade, tight compression garments 24-hours per day, seven days per week, is the key to improving circulation for the lymphatic system, making this a go-to prescription from Lipedema experts. Compression garments come in a variety of strengths and will be prescribed based on the stage and type of affected areas. The tighter the compression, the better.
A healthy and consistent lifestyle of clean eating and low-impact exercise to address obesity will also help with Lipedema. A diet focused on low-carb and low-sugar has proven successful. Low-impact exercise such as walking, water aerobics, yoga, or gymnastics has also reported success. Patients must avoid yo-yo dieting while also permanently losing or, at the very least, maintaining their weight. What works for one patient may not work for another. Diet and exercise recommendations and healthy practices are essential, but ultimately should be based on the individual with the understanding that weight gain is not an option.
Some patients opt-in to Manual Lymph Drainage massage (MLD), a gentle skin massage used to stimulate the circulation of the lymphatic system. While experts have yet to find significant evidence that MLD helps with Lipedema directly, some patients prefer it for its “hands-on” nature to addressing their symptoms.
For patients in the later stages of Lipedema, the pain and disruption to daily life are not permanently addressed with compression garments, diet, and exercise alone. Traditional liposuction that uses general anesthesia, radio frequencies, ultrasound, or lasers are possibly damaging to the lymphatic vessels, and as such are not an option for Lipedema patients, either. However, Lymph-sparing liposuction is safe, using surgical techniques that avoid lymphatic injury, and the use of local tumescent anesthesia reduces the risk of complications. Generally, the most painful areas should be treated first, starting high on the legs and then moving downward in future surgeries.
Perhaps the most noticeable benefit of lymph-sparing liposuction is how it is able to reduce the amount of subcutaneous fat tissue in the body. Lipedema reduction surgery not only significantly reduces fat tissue, but also removes fibrous tissue, making the limbs lighter, smaller, less tender, and smoother. It is critical to follow your physician’s guidelines to reduce any swelling and inflammation before the treatment. This is done by wearing compression garments and wraps along with receiving manual lymph drainage for several weeks following lipedema surgery and beyond. Patients wear medical-grade compression clothing for at least 8 weeks, and manual lymph drainage and massage are typically recommended as an ongoing and regular treatment.
Your tissue will be decongested, allowing your liposuction treatment to be as successful as possible. Some slight swelling and bruising may return immediately following the procedure, but this is expected and should subside over time. Some patients also report numbness as their nerves in the treated areas respond to treatment. Numbness may last for several months and up to one year, but when compared with the reduction in fat tissue, patients still see this as a huge improvement. Compression is critical to be maintained after the lipedema surgery as well, as the lymphatics are reestablished. The lymphatic function is often improved.
One of the most beneficial aspects of lymph-sparing liposuction is that the treatment does not rely on general anesthesia. While general anesthesia is used for a variety of treatments, it can cause complications for individuals with lipedema. In fact, it can cause complications in as high as 0.3% of liposuction treatments when used. Instead, lymph-sparing liposuction uses tumescent anesthesia to avoid these unwanted complications. In fact, general anesthesia can cause serious complications and even death in up to 0.3% of liposuction treatments when used. Patients are conscious for the duration of treatment, while the tumescent liquid acts as a local anesthetic in the treatment area. Patients take pain kills ahead of time to help with discomfort, and through the process feel little pain, and if anything, pressure in the area being treated.
Lipedema reduction surgery also makes sure to avoid any additional risks for the treatment. This type of liposuction procedure limits the amount of fat tissue that will be removed at once, and a follow-up appointment is scheduled for the day following the procedure to ensure the treatment and recovery are going as planned. While that may not seem like a benefit at first, it will actually make sure your body does not take any additional trauma than what is needed. The general amount of fat tissue that can be safely removed is around 5.0 liters. Smaller cannulas are also used to also keep down the risk of trauma to the body and an already compromised lymphatic system.
Even with all the challenges presented by lipedema, there are those who you can trust. Dr. Wright continues to strive for better education, research, and coverage for the lipedema community. Do not let these challenges bring you down even further; let Dr. Wright and his expert team help you to reduce the symptoms of lipedema and live your life fully! Dr. Wright can help find the right procedure to help manage your lipedema symptoms. Don’t let lipedema take over your life; contact us today!
Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat tissue, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells and adjoining connective tissue in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.
Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, discomfort and appearance of Lipedema nodules.
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like a pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized lipedema nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.
If one of these stages sounds like you, and you checked off multiple items on the list above, you may have Lipedema, but it’s impossible to say for sure. The only way to know for sure is to get a proper Lipedema diagnosis, which in itself is an important process.
In stage 3 lipedema, lobules develop in the skin. The presence of a lobule is one of the most important physical changes to occur in the skin that differentiates stage 2 and stage 3 lipedema. Originally described by Dr. Schmeller, a lobule is defined as a “hanging flap of skin,” also called an “extrusion of skin that protrudes or sticks out from the expected smooth contour of the skin.” Lobules can be seen from a distance. The lobules can occur in many areas on the body in lipedema patients, but the classic areas are just below the knees, or subpatellar lobules, lobules
Lipedema is categorized as lipomatosis, also known as a subcutaneous fat disease that is characterized by abnormal fibrosis of the subcutaneous fat tissue. Fibrosis (also known as fibrotic scarring), is a pathological wound healing in which connective tissue replaces normal tissue, eventually leading to the formation of permanent scar tissue. The fibrosis of Lipedema fat tissue gives it a hard, nodular feeling when touched.
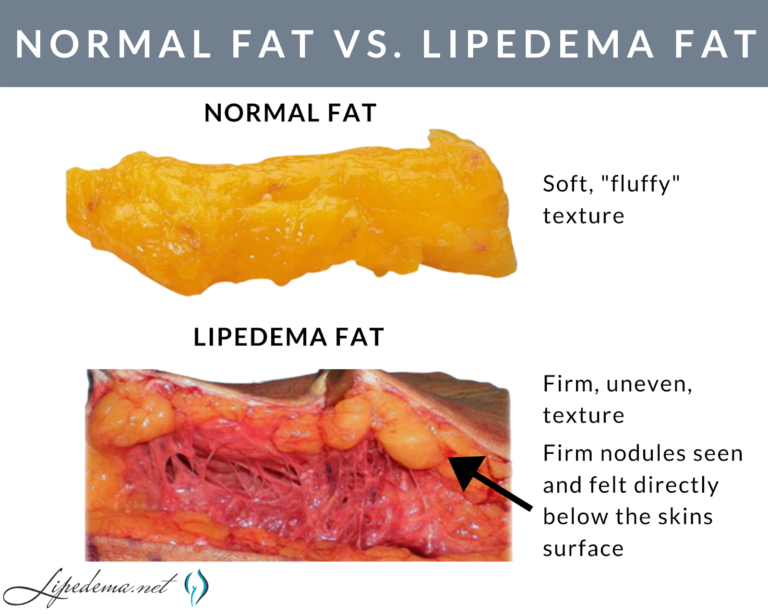
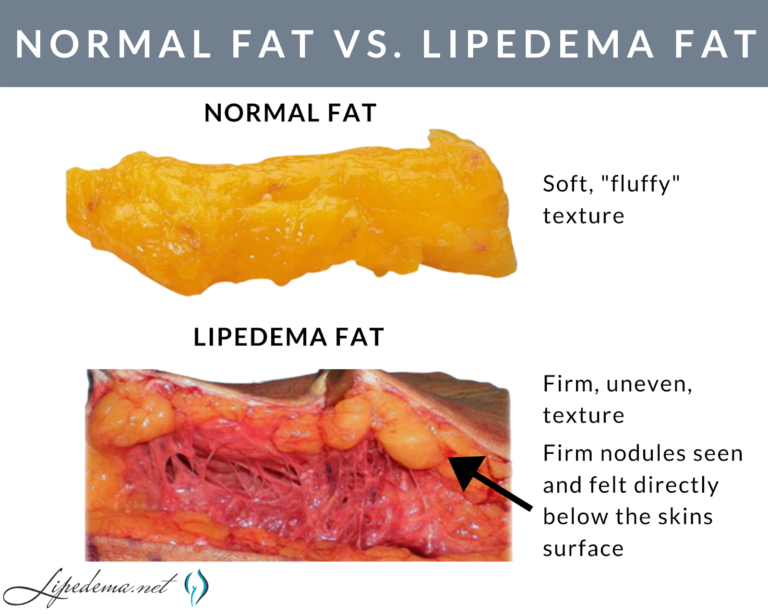
Lipedema nodules are felt and not usually seen. In lipedema, the skin surface is soft, but just below the surface, the nodules can be felt as harder areas. Early-stage Lipedema (Stage 1) has small nodules the size of small seeds or peas, which often appear pearl-size. Middle-stage Lipedema (Stage 2) has larger nodules that feel the size of walnuts or gumballs. Later stage Lipedema (Stage 3) is characterized by the presence of lobules. The nodules in Stage may be the same size as the nodules in Stage 2, or they may be larger nodules up to the size of a plum.
The Lipedema nodules felt on the skin are important criteria for diagnosing Lipedema. Nodular or bumpy subcutaneous fat occurs with other conditions or diseases such as cellulite or obesity and other fat disorders, however, subcutaneous nodules must be present to diagnose lipedema. These nodules represent excess and slightly disorganized fibrosis of the subcutaneous tissue. Inflammation of the adipose tissue in lipedema is likely the cause of this fibrosis.
In these cases, fibrosis tissue in Lipedema patients swirls around the adipose tissue, but it usually won’t completely encapsulate it. If the adipose tissue is completely encapsulated by fibrous tissue, eventually it leads to a lipoma. Women with lipedema have an increased number of lipomas, but most of the bumps felt on the skin are nodules, rather than lipomas.
There are other lipomatosis diseases that cause similar side effects as Lipedema to be aware of through the diagnosis process. Dercum’s disease, for example, is characterized by multiple painful subcutaneous lipomas. Madelung’s Disease also has subcutaneous nodules (but not many lipomas), however, these cases occur more in the upper half of the body. Overall, subcutaneous nodules are present in all patients with lipedema but they also occur in other subcutaneous fat diseases or lipomatosis.
In the earlier stages of Lipedema (Stage 1 and most patients in Stage 2), the subcutaneous nodules are removed with lipedema reduction surgery, which involves modification of cosmetic liposuction using tools and techniques which minimize harm to the lymphatics. In lipedema patients with larger or more adherent nodules, the nodules have to be manually extracted.
In these cases, a small incision is made over the nodules that resist removal with a suction cannula and are gently milked out of the skin. Obviously, surgeons don’t want to cause any more trauma than is absolutely necessary, however, there are instances where this method is the only way to get larger, more adherent nodules removed. Dr. Wright has several videos of the extraction process you can view here.
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
Note: There is no single test to diagnose Lipedema. Tests, however, are important to rule out a related disorder.
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema and to locate potential nodules. Lipedema has many similarities to venous insufficiency, so this can also help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time for the final step – finding a Lipedema specialist who can perform one of the diagnostic methods above. Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about the non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, it can give you an idea of what options may be available to you. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.