Dr. Wright’s innovative lipedema surgery techniques are transforming lives by improving mobility and enhancing the quality of life for patients. He will be conducting a video demonstration of his surgical techniques in a Master Class for Lipedema treatment at this year’s 1st Annual Lipedema World Congress. 

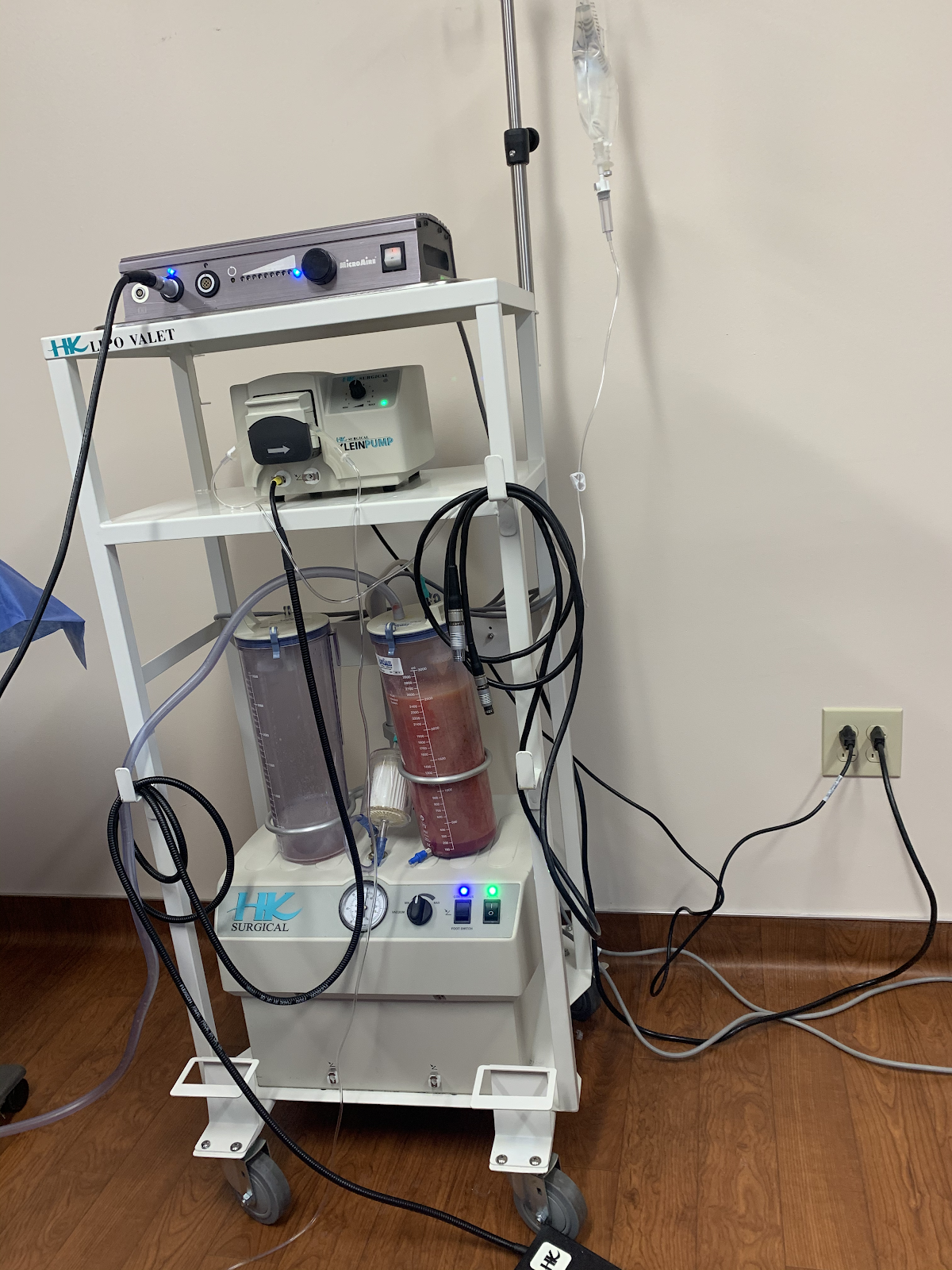
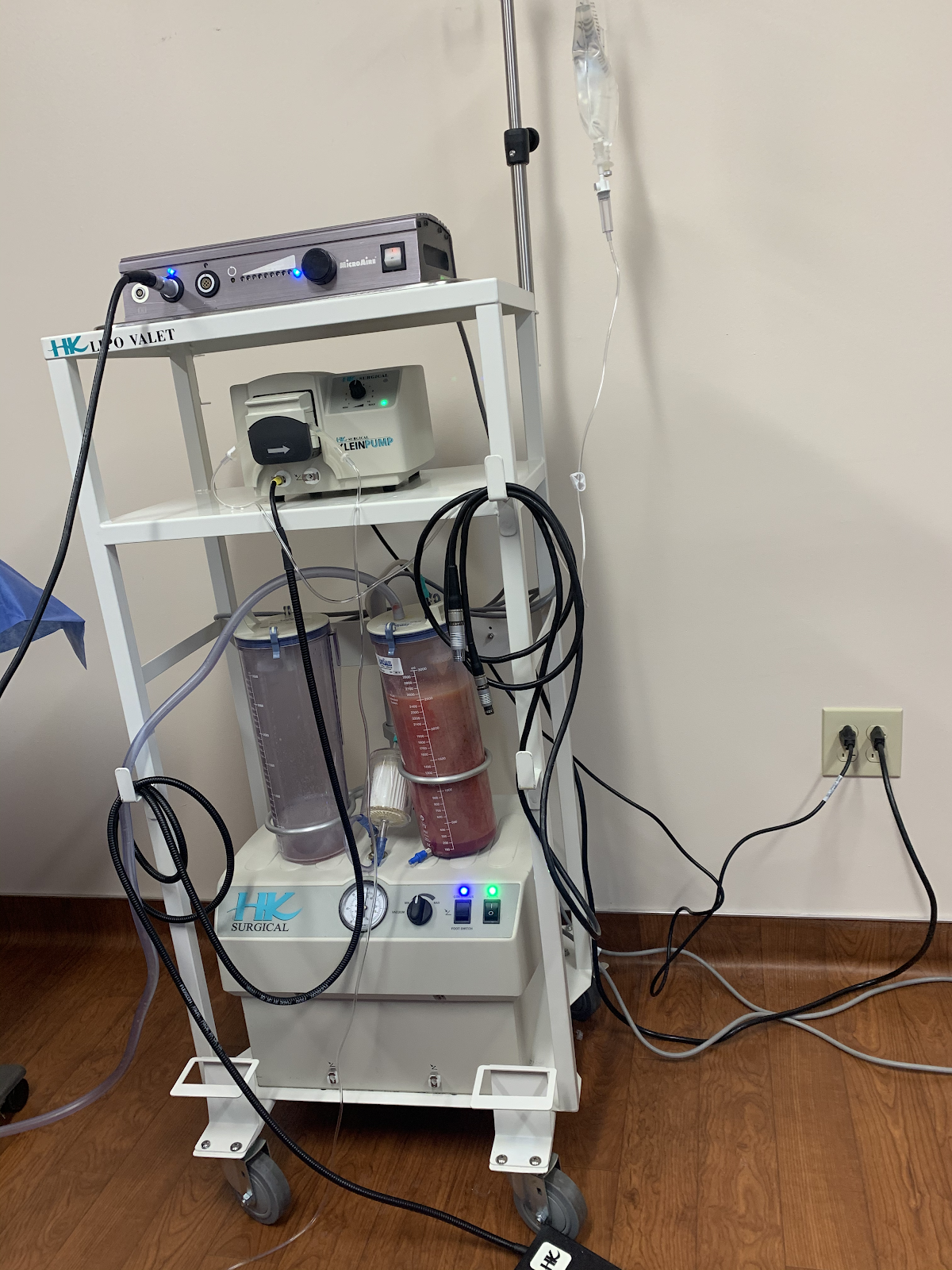
As a founding member of Lipedema World Alliance (LWA) and with expertise in this procedure, Dr. Wright will present the Tumescent Local Anesthesia (TLA) approach using power-assisted liposuction. In this course, he will describe his approach and techniques to give the best surgical outcomes and the greatest impact on mobility and quality of life long-term. His video demonstration and Master Class will be conducted on October 4, 2023, in Potsdam, Germany, with international participants from Spain, Italy, Austria, Germany, Norway, Lithuania, Sweden, Australia, India, Argentina, Brazil, USA, Iceland, Denmark, and Turkey. Below, we outline the topics and steps Dr. Wright will discuss.
Patients must first implement an anti-inflammatory diet and compression therapy. Their diets should emphasize low-refined carbs and avoiding processed foods, and medical-grade compression optimizes lymphatic function and tissue inflammation. These combined measures can decrease limb size, decrease pain, and lead to softening of the lipedema tissue ahead of surgery.
Before lipedema surgery, using high-frequency Ultrasound, the greater and smaller saphenous veins are mapped, and adjacent principal lymphatic collecting ducts are located. The watershed area around the principal superficial lymphatics in the legs is approached with extra care during surgery.
Tumescent fluid helps protect vascular and lymph vessels from injury, so the surgical area must be completely tumescent. Dr. Wright was trained in the Tumescent Technique by its inventor, Dr. Jeffery Klien. He follows The Klein Method and Dosing. General anesthesia adds the risk of general anesthetic medication. It can also lead to areas of inadequate tumescence because the general anesthesia blocks the ability to find areas that were incompletely tumescent.
Dr. Wright uses small (3mm) blunt cannulas to remove as much lipedema-affected adipose tissue as possible. This process works to debulk the area using longitudinal techniques.
The cannula is directed in longitudinal strokes, especially in the areas marked with lymphatic collectors, so it allows transecting of the lymphatic vessels. This requires frequent position changes, sometimes 8-12 different patient re-positions, to ensure he can remove the tissue using longitudinal cannula strokes.
After as much lipedema-affected tissue as possible has been removed with the suction cannula, he feels and massages the affected areas to check for any remaining fibrous lipedema nodules. If lipedema nodules are still present, then we manually loosen the nodules. If necessary, we manually extract them with an additional puncture of incision.
The patient is then placed in medical-grade compression to be worn for 24 hours a day for the first month.
Early-stage Lipedema (Stage 1) has small nodules the size of small seeds or peas, which often appear pearl-size. Middle-stage Lipedema (Stage 2) has larger nodules that feel the size of walnuts or gumballs. The presence of lobules characterizes the later stage, Lipedema (Stage 3). The nodules in Stage may be the same size as those in Stage 2, or they may be larger up to the size of a plum.
In the earlier stages of Lipedema (Stage 1 and most patients in Stage 2), the subcutaneous nodules are removed with lipedema reduction surgery, which involves modification of cosmetic liposuction using tools and techniques that minimize harm to the lymphatics. In lipedema patients with larger or more adherent nodules, the nodules have to be manually extracted.
In these cases, a small incision is made over the nodules that resist removal with a suction cannula and are gently milked out of the skin. Surgeons don’t want to cause any more trauma than is absolutely necessary. However, there are instances where this method is the only way to get larger, more adherent nodules removed. Dr. Wright has several videos of the extraction process you can view here.
The procedure typically takes several hours to complete, depending on the extent of the lipedema.
Patients may experience some discomfort and swelling in the days following the procedure, but this can be managed with pain medication and other treatments.
Most patients can return to work and other activities within a week or two, although this may vary depending on the extent of the liposuction and individual healing rates.
By reducing the amount of subcutaneous fat tissue, you can reduce any pain associated with lipedema. Lipedema reduction surgery, sometimes called Lymph sparing liposuction, will help you increase mobility without having the pain you have been feeling with lipedema since it started. This is huge for women with lipedema, especially because the pain and bruising is the leading symptom of seeking treatment. Women report a significant improvement in their ability to move around more freely, exercise more regularly, and enjoy day-to-day activities that were previously off-limits. Bumping into a chair or a corner no longer causes large bruises, playing with the family dog doesn’t cause pain when they jump, and everyday activities are no longer considered out of reach.


If you’re one of the millions of people living with lipedema, you know all too well the pain and discomfort of the condition. One of the most challenging aspects of lipedema is its effect on your knees, which can become swollen, painful, and difficult to move. But there is hope. Lipedema lipo is a safe, effective procedure that can help improve knee function and alleviate the symptoms of lipedema. By removing excess fat from the affected areas, this liposuction can reduce inflammation and pressure on the knees, allowing you to move more freely and with less pain. Best of all, the benefits of lipedema liposuction are long-lasting, giving you the relief you need to live your best life. So if you’re ready to discover the benefits of lipedema liposuction for improved knee function, read on to learn more!
Lipedema is a fat disorder that mainly affects women and causes enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Medical professionals often misdiagnose and dismiss lipedema as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
Women suffering from Lipedema often report the disease associated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.
Ultimately, effective treatment will require surgical intervention to alleviate the appearance and pain of symptoms. Liposuction performed on the affected limbs is generally the most effective treatment. Removing diseased fat deposits helps reduce swelling of the limbs and alleviates the pain that holds patients back from everyday activities.
This surgical treatment can provide various benefits and relieve the symptoms you are experiencing from lipedema. Dealing with lipedema can be difficult, especially if you are just now starting to take control of it.
Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the growth of more fat cells, which can overwhelm the lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and worsening an already stressed system. Studies have shown that lymphatic function can improve after this type of liposuction in women with Lipedema using blunt cannulas, generous tumescent anesthesia and special surgical techniques. Lipedema reduction surgery aims to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a “debulking” surgery, not a cosmetic surgery.
One of the most beneficial aspects of lymph-sparing liposuction is that the treatment does not rely on general anesthesia. While general anesthesia is used for various treatments, it is generally not recommended for individuals with lipedema. Instead, lymph-sparing liposuction uses tumescent anesthesia to avoid these unwanted complications. General anesthesia can cause severe complications and even death in up to 0.3% of liposuction treatments. Relying on tumescent anesthesia ensures the anesthetic fluid has been distributed throughout the tissue and it has had time for all the fat tissue to gel. Patients are conscious for the duration of treatment, while the tumescent liquid acts as a local anesthetic to the treatment area. Patients may take pain pills ahead of time to help with discomfort and sometimes use laughing gas. However, through the process, patients feel little pain and, if anything, pressure in the area being treated.
Perhaps the most noticeable benefit to lymph-sparing liposuction is how it can reduce the amount of subcutaneous fat tissue in the body. Lipedema reduction surgery significantly reduces fat tissue and removes fibrous tissue, making the limbs lighter, smaller, less tender, and smoother. Following your physician’s guidelines is critical to reducing swelling and inflammation before the treatment. This is done by wearing compression garments and wraps and receiving manual lymph drainage for several weeks following lipedema surgery and beyond. Patients wear medical-grade compression clothing for at least eight weeks, and manual lymph drainage and massage are typically recommended as an ongoing and regular treatment.
Your tissue will be decongested, making your liposuction treatment as successful as possible. Some slight swelling and bruising may return immediately following the procedure, but this is expected and should subside over time. Some patients also report numbness as their nerves in the treated areas respond to treatment. Numbness may last for several months and up to one year, but compared to the reduction in fat tissue; patients still see this as a huge improvement. Compression is also critical to be maintained after the lipedema surgery, as the lymphatics are re-established. The lymphatic function is often improved.
By reducing the amount of subcutaneous fat tissue, you can reduce any pain associated with lipedema. Lipedema reduction surgery, sometimes referred to as Lymph sparing liposuction, will help you increase mobility without having the pain you have been feeling with lipedema since it started. This is huge for women with lipedema, especially because the pain and bruising is the leading symptom of seeking treatment. Women report a significant improvement in their ability to move around more freely, exercise more regularly, and enjoy day-to-day activities that were previously off-limits. Bumping into a chair or a corner no longer causes large bruises, playing with the family dog doesn’t cause pain when they jump, and everyday activities are no longer considered out of reach.
The disproportionate fat accumulation in Lipedema causes mechanical imbalances that result in significant orthopedic problems. Knee joint degeneration is the most common arthritic condition of lipedema patients and is often disabling.
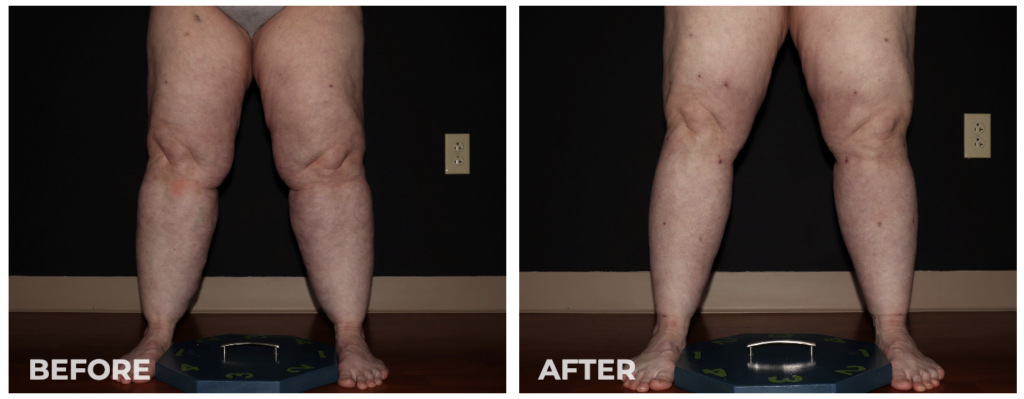
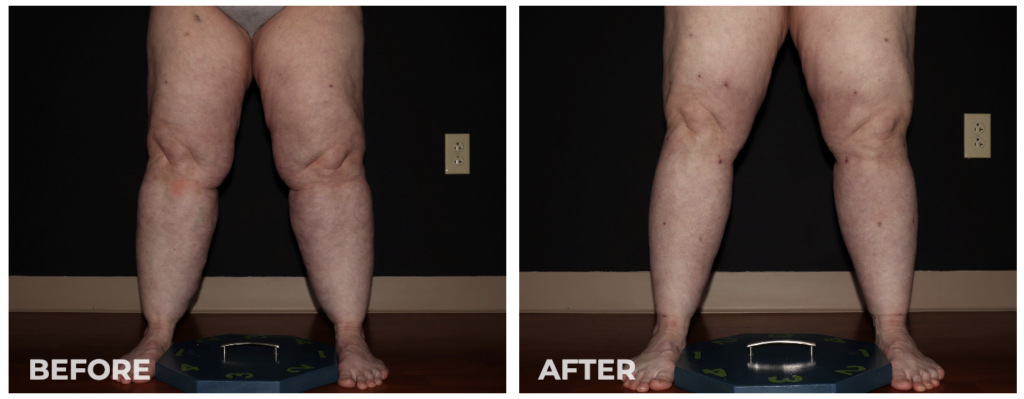
In our experience over the last five years, we’ve documented knee mechanics, including the range of motion, flection, gate, q-angle, and knee joint angulation (varus or valgus) in the joint. We found that lipedema reduction surgeries have improved knee flection by 8 degrees. That can make the difference between somebody climbing stairs, getting in and out of a tub, or getting in and out of chairs. This can be a huge difference! We’ve also seen about 8 degrees in valgus knee rotation, evening the pressure on the knee joint. As a result, this allows knee joints to last longer, avoiding arthritis that can result from rotation. Overall, 84% of patients who undergo lipedema reduction surgery over the 4-5 years had improvement in their gate and mobility leading to more accessible and enjoyable lives.
The procedure typically takes several hours to complete, depending on the extent of the lipedema.
Patients may experience some discomfort and swelling in the days following the procedure, but this can be managed with pain medication and other treatments.
Most patients can return to work and other activities within a week or two, although this may vary depending on the extent of the liposuction and individual healing rates.
If you are considering lipedema liposuction, finding a qualified and experienced surgeon specializing in this procedure is important. Look for a surgeon with a proven track record of success with lipedema patients and who prioritizes patient safety and comfort.
You can research surgeons online, read reviews from previous patients, and schedule consultations to discuss your options and ask any questions you may have. With the right surgeon, you can enjoy the benefits of lipedema liposuction for improved knee function and overall quality of life.
Living with lipedema can be a challenging experience, but there is hope. Lipedema liposuction is a safe and effective procedure that can help improve knee function and alleviate the symptoms of lipedema. Whether you are struggling with pain, swelling, stiffness, or reduced mobility, lipedema liposuction can provide a long-lasting solution that allows you to live your best life. To learn more about this procedure and whether it is right for you, consult a qualified lipedema liposuction surgeon today.
Back pain is a common problem that affects many people. But for those who suffer from lipedema, it can be much more than just an annoyance. Lipedema is a chronic condition that causes painful swelling in the legs and buttocks. Fortunately, there is a life-changing solution – lipedema surgery.
In this article, we will explore what lipedema is, its symptoms, causes, diagnosis, and treatment. We will also discuss the different types of lipedema surgery and the benefits of undergoing this procedure. Plus, we’ll look at the recovery process and the success stories of those who have gone through it themselves.


Lipedema is a condition that primarily affects women and is characterized by painful swelling of the legs and buttocks. It is known as a “painful fat disorder” because it causes fat to accumulate in the lower body, leading to discomfort and difficulty moving.
Lipedema can be difficult to diagnose because its symptoms are often similar to other conditions, such as obesity and lymphedema. Additionally, the cause of lipedema is still unknown, although it is believed to be a genetic disorder triggered by hormonal changes.
The most common symptom of lipedema is swelling of the legs and buttocks, and oftentimes the arms and abdomen. This swelling is usually symmetrical and occurs mainly in the lower parts of the body. It can also cause a feeling of tightness in the affected area, as well as aching, burning, and tenderness. The skin in the affected area may also appear dimpled, and the affected person may experience difficulty walking and standing for long periods.
In addition to physical symptoms, people with lipedema may also experience psychological symptoms such as low self-esteem and depression.
Lipedema can be difficult to diagnose because its symptoms are often similar to other conditions, such as obesity and lymphedema. To diagnose lipedema, your doctor will do a physical exam and ask about your medical history. They may also order tests, such as an ultrasound or MRI, to get a better look at the affected area.
Once lipedema is diagnosed, treatment may include lifestyle changes, such as diet and exercise, to reduce swelling and pain. Compression garments can also be used to help reduce swelling. In more severe cases, liposuction or liposculpture may be recommended to remove the excess fat.
A lot of women with lipedema have back pain because the “shelf” of weight accumulated on the lower back distorts the spine. The distortion from the fat lobule over the shelf will be sore if patients are on their feet or sitting for long periods. Many patients have chronic lower back pain without any relief because the constant existence of heavy lipedema tissue causes it.


Within a day or two after the tissue removal, patients report experiencing relief never experienced before. Unlike a pulled back muscle or a pinched nerve, surgery and the removal of this area’s fatty tissue and fluid is the only way to get relief.
Lipedema surgery is a life-changing solution for those suffering from lipedema of all types and stages, and especially with chronic secondary issues like back pain. This surgery involves the removal of excess fat from the affected area through liposuction or liposculpture. This surgery can help reduce the swelling, discomfort, and pain associated with lipedema. It can also improve mobility, reduce the risk of infection, and improve self-esteem.
There are many benefits to undergoing lipedema surgery. It can help reduce the swelling and pain associated with lipedema and improve mobility. It can also reduce the risk of orthopedic complications and improve self-esteem. Additionally, lipedema surgery can help reduce the risk of developing lymphedema, which can be a severe complication of lipedema. For patients with back pain, the surgery can provide almost immediate relief and allow them to have the ability for daily tasks once again once impossible – as simple as getting a good night’s rest, or the ability to perform accessible exercises more comfortably, like yoga and deep, restorative stretches.


Lipedema surgery can be an effective treatment for those who have experienced significant weight loss. After weight loss, the skin in the affected area may be loose and saggy. Lipedema surgery can help to tighten and firm the skin and reduce the swelling and pain associated with lipedema.
Recovery from lipedema surgery can take several weeks. During this time, it is important to rest and avoid strenuous activities. Your doctor may also recommend compression garments to help reduce swelling and improve comfort.
Lipedema surgery is a life-changing solution for those suffering from lipedema. It can reduce the swelling and pain associated with lipedema and improve mobility. It can also reduce the risk of infection and improve self-esteem. If you are suffering from lipedema and are looking for a solution, contact Dr. Wright and Laser Lipo and Vein Center for help with lipedema and back pain.
An estimated 17 million women in the U.S. and nearly 370 million women across the globe suffer from a condition known as Lipedema. What is regularly associated with rapid and uncontrollable weight gain in its initial stages can spiral out of control if left undiagnosed. As experts continue researching the causes and best treatment options for women with Lipedema, tumescent liposuction or lipedema reduction surgery remains the only way to reset the progressive disease and provide women with increased mobility and reprieve from daily pain.


Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Lipedema is often misdiagnosed and dismissed by medical professionals as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
Women suffering from Lipedema often report the disease associated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.


Ultimately, effective treatment will require surgical intervention to alleviate the appearance and pain of symptoms. Liposuction performed on the affected limbs is generally the most effective treatment. Removing fat deposits that are diseased helps reduce swelling of the limbs and alleviates the pain that holds patients back from everyday activities.
This surgical treatment can provide a variety of benefits and relieve the symptoms you are experiencing from lipedema. Dealing with lipedema can be difficult, especially if you are just now starting to take control of it.
Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the growth of more fat cells, which can overwhelm the lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and making an already stressed system worse. Using blunt cannulas and generous and special surgical techniques, studies have shown that lymphatic function can improve after this type of liposuction in women with Lipedema. The goal of lipedema reduction surgery is to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a “debulking” surgery, not a cosmetic surgery.Why is Lymph Sparing Liposuction Preferred for Lipedema Patients?
One of the most beneficial aspects of lymph-sparing liposuction is that the treatment does not rely on general anesthesia. While general anesthesia is used for various treatments, it is generally not recommended for individuals with lipedema. Instead, lymph-sparing liposuction uses tumescent anesthesia to avoid these unwanted complications. General anesthesia can cause severe complications and even death in up to 0.3% of liposuction treatments. Relying on tumescent anesthesia ensures the anesthetic fluid has been distributed throughout the tissue, and it has had time for all the fat tissue to gel. Patients are conscious for the duration of treatment, while the tumescent liquid acts as a local anesthetic to the treatment area. Patients may take pain pills ahead of time to help with discomfort and sometimes use laughing gas. However, through the process, patients feel little pain and, if anything, pressure in the area being treated.


Perhaps the most noticeable benefit to lymph-sparing liposuction is how it can reduce the amount of subcutaneous fat tissue in the body. Lipedema reduction surgery not only significantly reduces fat tissue but also removes fibrous tissue, making the limbs lighter, smaller, less tender, and smoother. Following your physician’s guidelines is critical to reduce swelling and inflammation before the treatment. This is done by wearing compression garments and wraps along with receiving manual lymph drainage for several weeks following lipedema surgery and beyond. Patients wear medical-grade compression clothing for at least eight weeks, and manual lymph drainage and massage are typically recommended as an ongoing and regular treatment.
Your tissue will be decongested, allowing your liposuction treatment to be as successful as possible. Some slight swelling and bruising may return immediately following the procedure, but this is expected and should subside over time. Some patients also report numbness as their nerves in the treated areas respond to treatment. Numbness may last for several months and up to one year, but compared to the reduction in fat tissue, patients still see this as a huge improvement. Compression is critical to be maintained after the lipedema surgery as well, as the lymphatics are re-established. The lymphatic function is often improved.
By reducing the amount of subcutaneous fat tissue, you can reduce any pain associated with lipedema. Lipedema reduction surgery, which is sometimes referred to as Lymph sparing liposuction, will be able to help you increase mobility without having the pain you have been feeling with lipedema since it started. This is huge for women with lipedema, especially because the pain and bruising is the leading symptom of seeking treatment. Women report a significant improvement in their ability to move around more freely, exercise more regularly, and enjoy day-to-day activities that were previously off-limits. Bumping into a chair or a corner no longer causes large bruises, playing with the family dog doesn’t cause pain when they jump, and everyday activities are no longer considered out of reach.
Significant blood loss is the most commonly reported side effect of lipedema surgery. Women with lipedema very often have large varicosities and studies have shown enlarged networks of veins in the legs of women with lipedema. Liposuction can cause significant blood loss if these veins are not treated before surgery. Even with proper preoperative treatment of dilated and varicose veins and good tumescent technique in women with lipedema, if the surgery is large enough, there can still be significant blood loss. In some cases even a blood transfusion has been needed in the postoperative period. The next most common complication of lipedema reduction surgery or lipedema liposuction is blood clots. Women with lipedema are, on average, heavier than women without lipedema making the risk of blood clots with the surgery greater. The risk of blood clots and other thrombotic complications can be greatly reduced with postoperative blood thinners. Careful surgeons should risk stratify their patients for possible blood clot complications and put them on prophylactic postoperative blood thinners. Infection is always a risk of any surgery including lipedema surgery. There has been a report of fat embolism with lipedema surgery. Death has to be included as a possible outcome. We are not aware of any deaths from lipedema surgery, but of course it is possible that any surgery can, in very rare circumstances, result in death. Finally, lymphatic injury is a real risk of liposuction and is a special concern for women with lipedema. Smaller cannulas are also used to keep down the risk of trauma to the body and an already compromised lymphatic system. With care and proper surgical technique lymphatic injury need not occur. In fact in skilled surgical hands lipedema reduction surgery may actually improve lymphatic function.
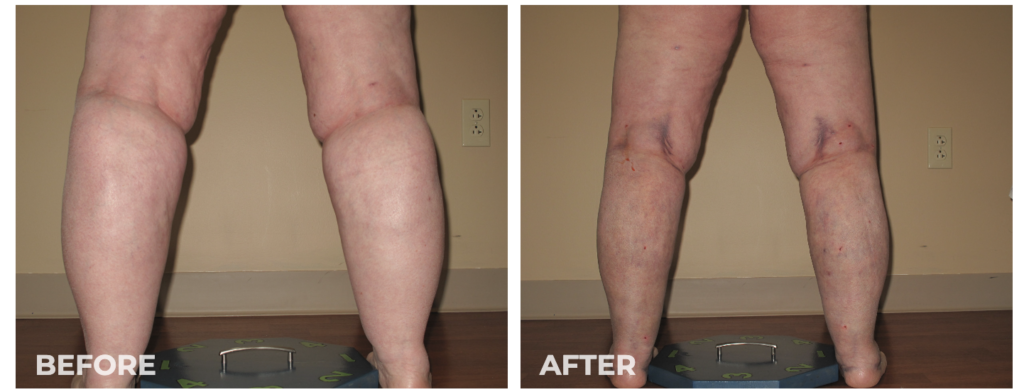
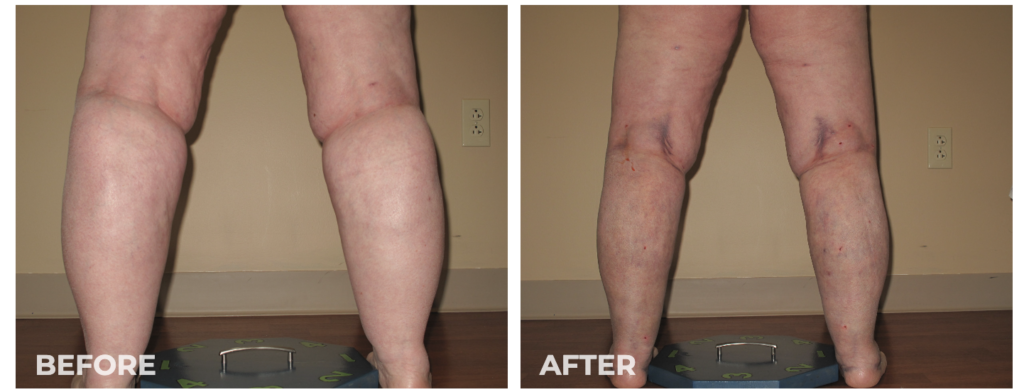
While the recovery can get painful, especially in more heavily used areas such as the arms and calves, patients will report that the payoff is well worth it. Lipedema fat more often accumulates around the lower body, including the thighs and buttocks. Women will often see the majority of their Lipedema fat in these areas. However, they can also commonly find Lipedema fat accumulation around the inner knee and backside of their leg. After the removal of lipedema tissue in these areas, patients are not only more mobile and can get around more easily, but they experience far less pain in their daily lives.


This procedure allows for a more active and healthy lifestyle, which many patients have experienced for years (and in some instances, it’s been decades). If paired with proper compression therapy, a healthy diet, tons of water for hydration, and responsible maintenance, women with lipedema are afforded a much higher quality of life and more enjoyable day-to-day. The reduction of irregular and heavy fat can improve joint function, making everyday tasks such as walking, climbing stairs, tying shoes, or even getting up from a chair much easier than before. Normal tasks that many take for granted are daunting and painful for women with lipedema, and lymph-sparing liposuction can help reset the clock by several years to help.
While lymph-sparing liposuction for lipedema is generally safe in healthy individuals, risks such as infection, bleeding, and trauma to the area may occur. Post-operative swelling in the limbs after surgery, which occurs with any liposuction procedure, is more prolonged in individuals with lipedema. The swelling typically worsens for a few months before it gets better, and the full benefit may not be realized for six months to a year. However, overall, most patients with lipedema experience significant improvement of many or all of their symptoms, with varying individual results. It’s not uncommon for Dr. Wright and his team to complete the procedure, and their patient notices a change before they leave the office, especially when large amounts of fat tissue are removed.
Although some people who have lipedema in one specific area may need only one procedure, most people undergo multiple lymph-sparing liposuction procedures to address all the different areas affected by lipedema. The multiple liposuction procedures must be staged or separated to be done safely. The timing of the procedures depends on multiple factors, including the clinical stage of lipedema in the patient, the amount of fat being removed, the patient’s health and mobility, and other logistical factors. Generally, each procedure should be spaced out by at least three months to allow for proper recovery.
After the lipedema surgery, patients go home the same day but should be sent home already in their compression garments. The first afternoon after surgery should be spent resting, and it’s likely patients are extremely drowsy from the procedure and medications. The following day post-op check-in should be completed before returning home. Patients will be sore and will continue to experience drainage of tumescent fluids. Padding around the incision points is required for several weeks. Compression garments are worn around the lock for the first several weeks, then worn during the daytime hours only before eventually tapering off after 12 weeks.
As you can see, lymph-sparing liposuction has plenty of exciting benefits. This procedure can make living easier with unwanted symptoms such as difficulty with mobility, pain, and tenderness. Physicians like Dr. Wright can provide you with the needed treatment to reduce your lipedema symptoms. Contact us today!
June is Lipedema Awareness month, one in which the Lipedema community focuses (even more than usual) on how to reach women who have lived with this painful and distressing disease. While we’ve seen great strides in awareness, insurance coverage, and slightly greater recognition of this disease in the medical community, we continue to fight an uphill battle as women are underdiagnosed or completely dismissed when discussing their struggles and side effects with their providers. As a result, our team has put together some of the most important and impactful information for all of you, and we’re kicking off the month with a webinar from a team of lipedema experts.
Join us on Tuesday, June 7th, 2022 at 8 pm ET to listen to our panel discuss Recognizing Lipedema and Treatment Options. This is a FREE event!
Register here, or listen to the recording following the webinar at tactilemedical.com/education.
Drs. Steve Dean, Thomas Wright, and Tony Gasparis with Julie Green, OTR/L CLT-LANA, WCC, CLWT discuss lipedema – the pathophysiology, association with vein disease, conservative treatments, and surgical options available for patients.


Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the collection of fat cells, which can cause the obstruction of lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and making an already stressed system worse. Using blunt cannulas generous and special surgical techniques, studies have shown that lymphatic function can actually improve after this type of liposuction in women with Lipedema. The goal of lipedema reduction surgery is to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a debulking surgery, not a cosmetic surgery.
There are two specialized liposuction techniques that have been shown in studies to benefit individuals with lipedema: water-assisted and tumescent liposuction. In addition to the surgical equipment used, it is important to choose a surgeon with experience and one that is cautious when performing lipedema surgery. These factors can have an important influence on protecting lymphatic flow and function.
Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.


Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper Lipedema diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
Overall, Lipedema appears in a series of three stages. Do any of these sound like you?
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.


| Photo credit: Linda Anne Kahn at Integrative Treatment of Lipedema |
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them.
When is the best time to get lipedema surgery?
There are two categories of treatment, surgical and non-surgical. Insurance providers require patients first try non-surgical treatment options before they’ll consider approving lipedema surgery, and Lipedema providers should be able to walk patients through this. While Lymph-sparing liposuction is the only treatment option that can provide permanent results by removing the lipedema fat, non-surgical options can help slow progression and are also necessary post-surgery (so it’s still important to practice them!).
To the dismay of patients, wearing medical-grade, tight compression garments 24-hours per day, seven days per week, is the key to improving circulation for the lymphatic system, making this a go-to prescription from Lipedema experts. Compression garments come in a variety of strengths and will be prescribed based on the stage and type of affected areas. The tighter the compression, the better.
A healthy and consistent lifestyle of clean eating and low-impact exercise to address obesity will also help with Lipedema. A diet focused on low-carb and low-sugar has proven successful. Low-impact exercise such as walking, water aerobics, yoga, or gymnastics has also reported success. Patients must avoid yo-yo dieting while also permanently losing or, at the very least, maintaining their weight. What works for one patient may not work for another. Diet and exercise recommendations and healthy practices are essential, but ultimately should be based on the individual with the understanding that weight gain is not an option.
Some patients opt-in to Manual Lymph Drainage massage (MLD), a gentle skin massage used to stimulate the circulation of the lymphatic system. While experts have yet to find significant evidence that MLD helps with Lipedema directly, some patients prefer it for its “hands-on” nature to addressing their symptoms.
For patients in the later stages of Lipedema, the pain and disruption to daily life are not permanently addressed with compression garments, diet, and exercise alone. Traditional liposuction that uses general anesthesia, radio frequencies, ultrasound, or lasers are possibly damaging to the lymphatic vessels, and as such are not an option for Lipedema patients, either. However, Lymph-sparing liposuction is safe, using surgical techniques that avoid lymphatic injury, and the use of local tumescent anesthesia reduces the risk of complications. Generally, the most painful areas should be treated first, starting high on the legs and then moving downward in future surgeries.
Perhaps the most noticeable benefit of lymph-sparing liposuction is how it is able to reduce the amount of subcutaneous fat tissue in the body. Lipedema reduction surgery not only significantly reduces fat tissue, but also removes fibrous tissue, making the limbs lighter, smaller, less tender, and smoother. It is critical to follow your physician’s guidelines to reduce any swelling and inflammation before the treatment. This is done by wearing compression garments and wraps along with receiving manual lymph drainage for several weeks following lipedema surgery and beyond. Patients wear medical-grade compression clothing for at least 8 weeks, and manual lymph drainage and massage are typically recommended as an ongoing and regular treatment.
Your tissue will be decongested, allowing your liposuction treatment to be as successful as possible. Some slight swelling and bruising may return immediately following the procedure, but this is expected and should subside over time. Some patients also report numbness as their nerves in the treated areas respond to treatment. Numbness may last for several months and up to one year, but when compared with the reduction in fat tissue, patients still see this as a huge improvement. Compression is critical to be maintained after the lipedema surgery as well, as the lymphatics are reestablished. The lymphatic function is often improved.
One of the most beneficial aspects of lymph-sparing liposuction is that the treatment does not rely on general anesthesia. While general anesthesia is used for a variety of treatments, it can cause complications for individuals with lipedema. In fact, it can cause complications in as high as 0.3% of liposuction treatments when used. Instead, lymph-sparing liposuction uses tumescent anesthesia to avoid these unwanted complications. In fact, general anesthesia can cause serious complications and even death in up to 0.3% of liposuction treatments when used. Patients are conscious for the duration of treatment, while the tumescent liquid acts as a local anesthetic in the treatment area. Patients take pain kills ahead of time to help with discomfort, and through the process feel little pain, and if anything, pressure in the area being treated.
Lipedema reduction surgery also makes sure to avoid any additional risks for the treatment. This type of liposuction procedure limits the amount of fat tissue that will be removed at once, and a follow-up appointment is scheduled for the day following the procedure to ensure the treatment and recovery are going as planned. While that may not seem like a benefit at first, it will actually make sure your body does not take any additional trauma than what is needed. The general amount of fat tissue that can be safely removed is around 5.0 liters. Smaller cannulas are also used to also keep down the risk of trauma to the body and an already compromised lymphatic system.
Even with all the challenges presented by lipedema, there are those who you can trust. Dr. Wright continues to strive for better education, research, and coverage for the lipedema community. Do not let these challenges bring you down even further; let Dr. Wright and his expert team help you to reduce the symptoms of lipedema and live your life fully! Dr. Wright can help find the right procedure to help manage your lipedema symptoms. Don’t let lipedema take over your life; contact us today!
An estimated 17-million women in the U.S. and nearly 370 million women across the globe suffer from a condition known as Lipedema. What is regularly associated with rapid and uncontrollable weight gain in its initial stages can quickly spiral out of control if left undiagnosed.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate in comparison to the rest of the body.


Lipedema is often misdiagnosed and dismissed by medical professionals as simple obesity, leaving affected women to deal with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses. Ultimately, effective treatment will require cosmetic intervention in order to alleviate the appearance and pain of symptoms. Liposuction performed on the affected limbs is generally the most effective form of treatment. Removing fat deposits that are diseased not only helps reduce swelling of the limbs but alleviates the pain that holds patients back from everyday activities.
One of the top recommended treatments for dealing with lipedema is lymph sparing liposuction. This surgical treatment is able to provide a variety of benefits and relieve the symptoms you are experiencing from lipedema. Dealing with lipedema can be difficult, especially if you are just now starting to take control of it.
Women suffering from Lipedema often report the disease in association with painful symptoms that trigger difficulties dealing with everyday life activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling which can lead to further medical complications.
Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the collection of fat cells, which can cause the obstruction of lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and making an already stressed system worse. Using blunt cannulas generous and special surgical techniques, studies have shown that lymphatic function can actually improve after this type of liposuction in women with Lipedema. The goal of lipedema reduction surgery is to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a debulking surgery, not a cosmetic surgery.
There are two specialized liposuction techniques that have been shown in studies to benefit individuals with lipedema: water-assisted and tumescent liposuction. In addition to the surgical equipment used, it is important to choose a surgeon with experience and one that is cautious when performing lipedema surgery. These factors can have an important influence on protecting lymphatic flow and function.
One of the most beneficial aspects of lymph sparing liposuction is that the treatment does not rely on general anesthesia. While general anesthesia is used for a variety of treatments, it can cause complications for individuals with lipedema. In fact, it can cause complications in as high as 0.3% of liposuction treatments when used. Instead, lymph sparing liposuction uses tumescent anesthesia to avoid these unwanted complications. In fact, general anesthesia can cause serious complications even death in up to 0.3% of liposuction treatments when used. Patients are conscious for the duration of treatment, while the tumescent liquid acts as a local anesthetic to the treatment area. Patients take pain kills ahead of time to help with discomfort, and through the process feel little pain, and if anything, pressure in the area being treated.
Perhaps the most noticeable benefit to lymph sparing liposuction is how it is able to reduce the amount of subcutaneous fat tissue in the body. Lipedema reduction surgery not only significantly reduces fat tissue, but also removes fibrous tissue, making the limbs lighter, smaller, less tender, and smoother. It is critical to follow your physician’s guidelines to reduce any swelling and inflammation before the treatment. This is done by wearing compression garments and wraps along with receiving manual lymph drainage for several weeks following lipedema surgery and beyond. Patients wear medical-grade compression clothing for at least 8 weeks, and manual lymph drainage and massage are typically recommended as an ongoing and regular treatment.
Your tissue will be decongested, allowing your liposuction treatment to be as successful as possible. Some slight swelling and bruising may return immediately following the procedure, but this is expected and should subside over time. Some patients also report numbness as their nerves in the treated areas respond to treatment. Numbness may last for several months and up to one year, but when compared with the reduction in fat tissue, patients still see this as a huge improvement. Compression is critical to be maintained after the lipedema surgery as well, as the lymphatics are reestablished. The lymphatic function is often improved.


By reducing the amount of subcutaneous fat tissue, you can reduce any pain that is associated with lipedema. Lipedema reduction surgery, which is sometimes referred to as Lymph sparing liposuction, will be able to help you increase mobility without having the pain you have been feeling with lipedema since it started. This is huge for women with lipedema, especially because the pain and bruising is the leading symptom of seeking treatment. Women report a significant improvement in their ability to move around more freely, exercise more regularly and enjoy day-to-day activities that were previously off-limits. Bumping into a chair or a corner no longer causes large bruises, playing with the family dog doesn’t cause pain when they jump, and everyday activities are no longer considered out of reach.
Lipedema reduction surgery also makes sure to avoid any additional risks for the treatment. This type of liposuction procedure limits the amount of fat tissue that will be removed at once, and a follow-up appointment is scheduled for the day following the procedure to ensure the treatment and recovery are going as planned. While that may not seem like a benefit at first, it will actually make sure your body does not take any additional trauma than what is needed. The general amount of fat tissue that can be safely removed is around 5.0 liters. Smaller cannulas are also used to also keep down the risk of trauma to the body and an already compromised lymphatic system.


While the recovery can get painful, especially in more heavily used areas such as the arms and calves, patients will report that the payoff is well worth it. Lipedema fat more often accumulates around the lower body, including the thighs and buttocks. Women will often see the majority of their Lipedema fat in these areas. However, they can also commonly find Lipedema fat accumulation around the inner knee and backside of their leg. After the removal of lipedema tissue in these areas, patients are not only more mobile and can get around more easily, but they experience far less pain in their daily lives.
This procedure allows for a more active and healthy lifestyle, which many patients have experienced in years (and in some instances, it’s been decades). If paired with proper compression therapy, a healthy diet, tons of water for hydration, and responsible maintenance, women with lipedema are afforded a much higher quality of life and more enjoyable day-to-day. The reduction of irregular and heavy fat can improve joint function, making everyday tasks such as walking, climbing stairs, tying shoes, or even getting up from a chair much easier than before. Normal tasks that many take for granted are daunting and painful for women with lipedema, and lymph sparing liposuction can help reset the clock by several years to help provide a higher quality of life for those who have missed it for years.
While lymph sparing liposuction for lipedema is generally safe in healthy individuals, risks such as infection, bleeding, and trauma to the area may occur. Post-operative swelling in the limbs after surgery, which occurs with any liposuction procedure, is more prolonged in individuals with lipedema. The swelling typically worsens for a few months before it gets better, and the full benefit may not be realized for six months to a year. However, overall, most patients with lipedema experience significant improvement of many or all of their symptoms, with varying individual results. It’s not uncommon for Dr. Wright and his team to complete the procedure, and their patient notices a change before they leave the office, especially when large amounts of fat tissue are removed.
Although some people who have lipedema in one specific area may need only one procedure, most people undergo multiple lymph sparing liposuction procedures to address all the different areas affected by lipedema. The multiple liposuction procedures need to be staged, or separated, to be done safely. The timing of the procedures depends on multiple factors, including the clinical stage of lipedema in the patient, the amount of fat being removed, the patient’s health and mobility, and other logistical factors. Generally, each procedure should be spaced out by at least three months to allow for proper recovery. After the lipedema surgery, patients go home the same day but should be sent home already in their compression garments. The first afternoon after surgery should be spent resting, and it’s likely patients are extremely drowsy from the procedure and medications. The following day post-op check-in should be completed before returning home. Patients will be sore and will continue to experience drainage of tumescent fluids. Padding around the incision points is required for several weeks, and compression garments are worn around the lock for the first several weeks, then worn during the daytime hours only, before eventually tapering off after 12 weeks.
As you can see, there are plenty of exciting benefits to lymph-sparing liposuction. This procedure can make it easier to live with unwanted symptoms such as difficulty with mobility, pain, and tenderness. Physicians such as Dr. Wright can provide you with the needed treatment that it takes to reduce your lipedema symptoms. Contact us today!
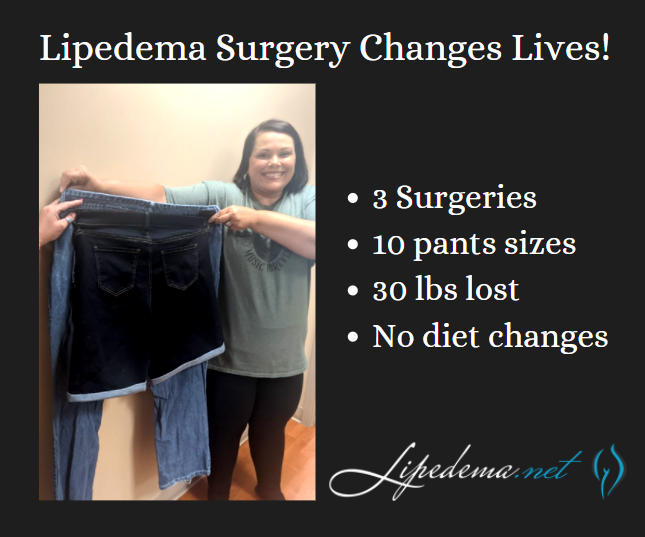
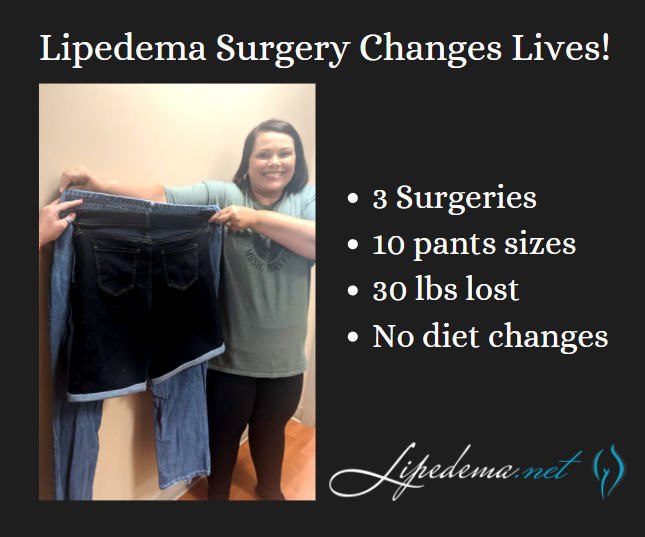
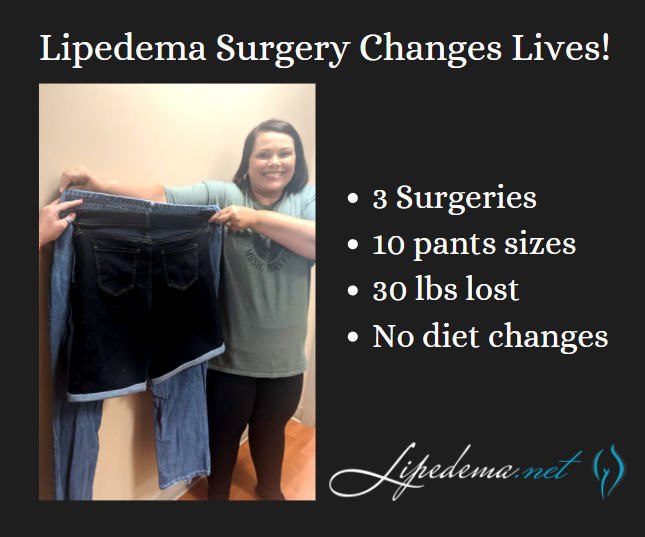
There’s nothing more satisfying and exciting for Dr. Wright and his team at Laser Lipo & Vein Center than celebrating patient wins! One of our favorite patients, Rita, spent her time in quarantine focused on getting through her lipedema surgeries, recovering safely at home, and both she and our team couldn’t be happier with her results! Rita’s experience is proof that Lipedema surgery can transform patient experiences as they walk through life (literally!) from pain and immobility to pain-free progress!
Rita has undergone three Lipedema surgeries on her legs and has seen dramatically positive results. She’s continued to follow a generally healthy diet both before and after her surgeries but did not implement any form of diet changes, so these results are primarily the outcome of her lipedema surgeries! She’s gone from a size 24 to a size 14 in jean size, lost 30 pounds, and is now more easily active and mobile day-in and day-out.
There are so many day-to-day activities that those without Lipedema wouldn’t think twice about, but patients with Lipedema struggle with and dread. Post-surgery, Rita has reported back to our office that after losing 10 pants sizes and removing the irregular lipedema fat in her lower body, she has no problems fitting into those frustrating chairs with arms on either side, she has enjoyed walking around the amusement park with her 10-year-old daughter without having to take breaks, and overall has enjoyed her active lifestyle, without the pain that used to accompany it!


Lipedema is a subcutaneous fat disease that primarily affects women. When we reference the “subcutaneous” tissue and fat, we’re referencing the layer of tissue directly under the skin.
Shockingly, Lipedema affects an estimated 17 million women across the globe. This disease affects a huge number of women, the majority of whom are still walking through their world in a lot of physical and mental pain. Lipedema is a disease that leads to the excessive build-up of fat cells, primarily in the arms and legs. Women suffering from it often have “pockets” of fat on their limbs that appear disproportionate in comparison to the rest of their bodies. This disease causes an enlargement of the legs due to deposits of fat under the skin, and typically gets worse over time, making diagnosis and treatment essential.
It’s common for women with Lipedema to have a small upper body, while their lower body is disproportionately larger (kind of like an extreme pear-shaped body). Pockets of fat develop in the affected areas and appear to bulge in and out of the top layer of the skin. This is often mischaracterized as cellulite, rather than painful lipomas.
These pockets of Lipedema fat are accompanied by painful symptoms, such as excessive swelling, pain to the touch, numbness, and very easy bruising. If my dog jumped up on my legs, it was excruciating. Everyday occurrences that most people don’t think twice about, like accidentally bumping into a table or chair, can cause deep, painful bruises.


As Lipedema progresses over time, these symptoms will continue to get worse as more Lipedema fat accumulates, and many women report that they are less and less mobile or active as time goes on. As a result, these women are stuck in a terrible cycle; they are less mobile, so they often gain weight, then it’s even more difficult and painful to be active, and the cycle goes on and on.
While many women also see weight gain in their arms, it’s common that the following areas are greatly affected:


We know that Lipedema is inherited in about 60% of women, and early studies show a genetic component is definitely at play (read more about that here!) and is the result of a malfunction of the Lymphatic System. The lymphatic system is a network of tissues and organs that help rid the body of toxins, waste, and other unwanted materials. This system transports lymph fluid throughout the body and is important for maintaining a healthy immune system. This disease affects the lymphatic system’s tiny vessels (microvessels) that cause a build-up of excess fluid around the body’s tissue cells. These tissue cells (located in the subcutaneous layers we discussed above) are then full of excess fluid, causing the swelling, soreness, bruising, and pain that many women with Lipedema report.
As researchers continue to gain understanding and genetic proof of Lipedema and differentiate it genetically from other diseases that they’re commonly misdiagnosed with, it will only become easier for women with Lipedema to get a proper diagnosis. Then, as the disease is more widely known and understood, treatments will become better and better, it will be more difficult for insurance providers to refuse coverage for treatments. Hopefully from there, more doctors will be trained in treating women with Lipedema properly, so treatments will become more accessible across the country! Read more about the first-ever Standard of Care Guidelines for Lipedema here!
There are two categories of treatment, surgical and non-surgical. Insurance providers require patients first try non-surgical treatment options before they’ll consider approving lipedema surgery, and Lipedema providers should be able to walk patients through this. While Lymph-sparing liposuction is the only treatment option that can provide permanent results by removing the lipedema fat, non-surgical options can help slow progression and are also necessary post-surgery (so it’s still important to practice them!).
To the dismay of patients, wearing medical-grade, tight compression garments 24-hours per day, seven days per week, is the key to improve circulation for the lymphatic system, making this a go-to prescription from Lipedema experts. Compression garments come in a variety of strengths and will be prescribed based on the stage and type of affected areas. The tighter the compression, the better.
A healthy and consistent lifestyle of clean eating and low-impact exercise to address obesity will also help with Lipedema. A diet focused on low-carb and low-sugar has proven successful. Low-impact exercise such as walking, water aerobics, yoga, or gymnastics has also reported success. Patients must avoid yo-yo dieting while also permanently losing or, at the very least, maintaining their weight. What works for one patient may not work for another. Diet and exercise recommendations and healthy practices are essential, but ultimately should be based on the individual with the understanding that weight gain is not an option.
Some patients opt-in to Manual Lymph Drainage massage (MLD), a gentle skin massage used to stimulate the circulation of the lymphatic system. While experts have yet to find significant evidence that MLD helps with Lipedema directly, some patients prefer it for its “hands-on” nature to addressing their symptoms.
For patients in the later stages of Lipedema, the pain and disruption to daily life are not permanently addressed with compression garments, diet, and exercise alone. Traditional liposuction that uses general anesthesia, radio frequencies, ultrasound, or lasers are possibly damaging to the lymphatic vessels, and as such are not an option for Lipedema patients, either. However, Lymph-sparing liposuction is safe, using surgical techniques that avoid lymphatic injury, and the use of local tumescent anesthesia reduces the risk of complications. Generally, the most painful areas should be treated first, starting high on the legs and then moving downward in future surgeries.
Even with all the challenges presented by lipedema, there are those who you can trust. Dr. Wright continues to strive for better education, research, and coverage for the lipedema community. Do not let these challenges bring you down even further; let Dr. Wright and his expert team help you to reduce the symptoms of lipedema and live your life fully! Dr. Wright can help find the right procedure to help manage your lipedema symptoms. Don’t let lipedema take over your life; contact us today!
Hi everyone – it’s Cat again!
If you haven’t read my story or seen any of my videos before, I’m a long-time patient of Dr. Wright and am working towards completing a total of five Lipedema liposuction surgeries with him. I’ve put together some helpful tips and a bit about my story, and you can find all my videos on Dr. Wrights YouTube channel.
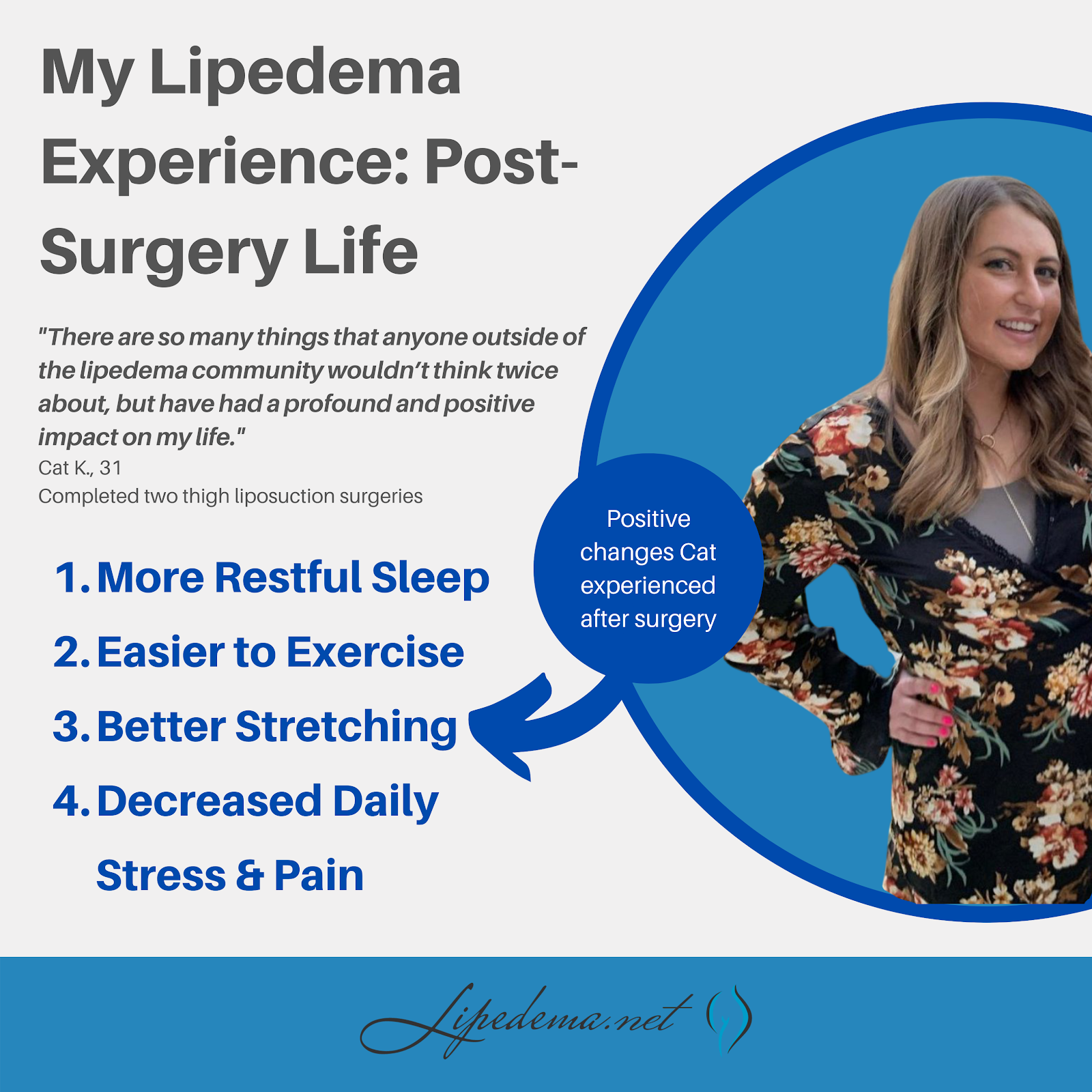
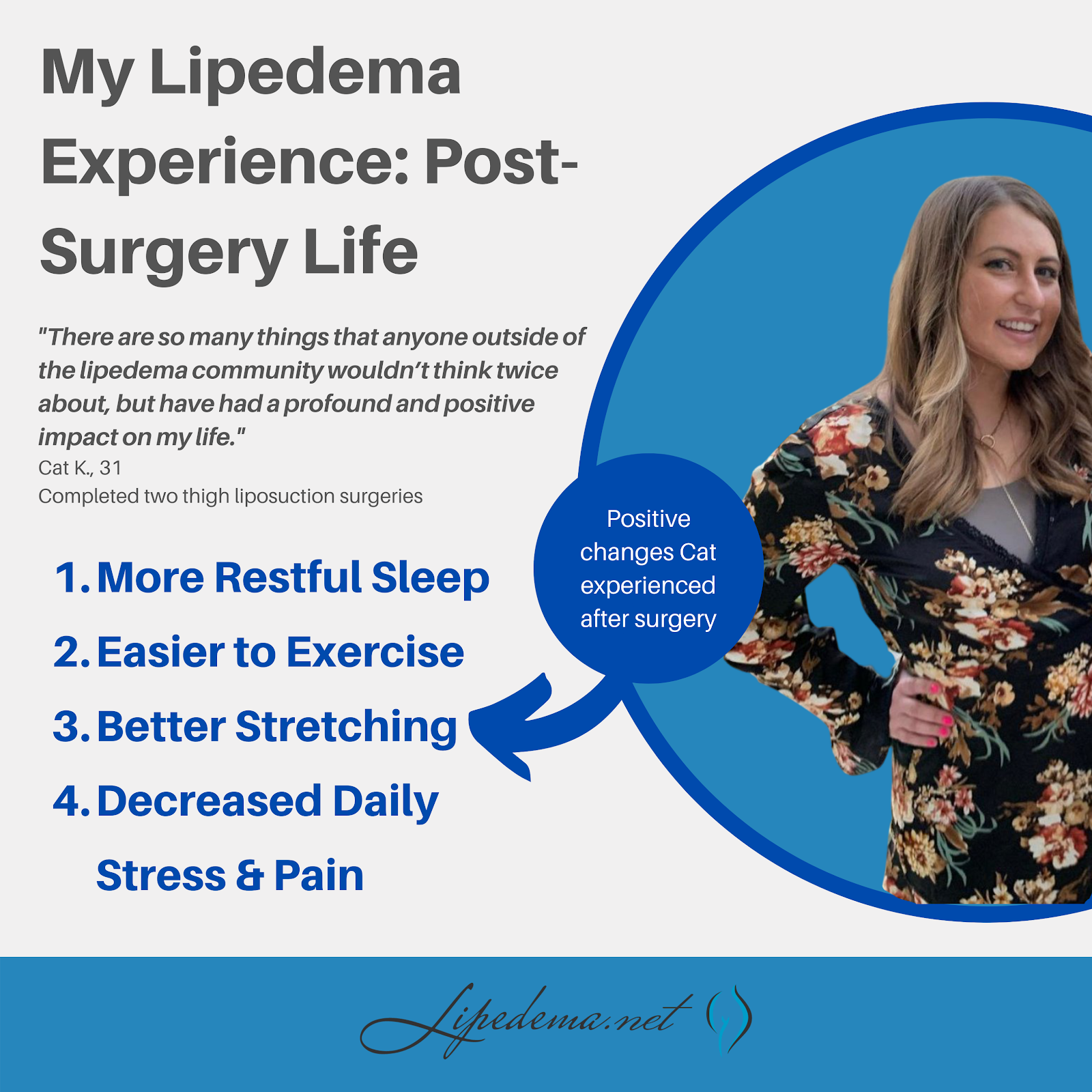
At the end of February, I hit the one-year mark since undergoing my second Lipedema surgery. My initial goal was to get all five surgeries completed within one year of being diagnosed (in October 2019). However, thanks to COVID-19 and life and money and insurance unhelpful companies, here I am; It’s already March of 2021, and I’m praying I can get a third surgery done soon! Until then, I want to continue helping women like me who are struggling with Lipedema, in the hopes that I can show you the light at the end of the tunnel, and help make the journey a little less overwhelming! In the video below and through this post, I’ll take you through what my life has been like since recovering from my 2nd surgery, and what it’s like being half-healed; I’m living in the in-between of some areas being treated while others are still in the midst of the struggle.
After being officially diagnosed and working on non-surgical treatments, I met with Dr. Wright and his team to determine what surgeries I would need and on what areas of my body. We determined that I had Lipedema swelling and fat in my legs, abdomen, and arms, and would need a total of five surgeries: My legs, abdomen, front of my thighs, back of my thighs + buttocks, and my calves. I completed the front of my thighs in December 2019 and the back of my thighs and buttocks in February 2020. I had about 8 liters of fat removed in the first Lipedema removal surgery, and 12 liters (INSANE) in my 2nd surgery. To give you an idea of this volume, 8 liters is about 2 gallons of fat. So between the two, I’m free of a huge amount of lippy fat and am about 35 pounds lighter.
Because I live in Austin and Dr. Wright’s office is in St. Louis, the COVID-19 pandemic has made continuing surgeries difficult. His expertise, kindness, and genuine passion for helping women like us make the travel well worth it under any other circumstances, but we’re trying to be extremely cautious with flights. Over the last year, my partner and I have even thought about making the 13-hour drive to his office rather than continuing to wait, but the thought of riding in a car post-surgery is daunting.


In mid-march, I have a virtual consultation with Dr. Wright to touch base and make plans for my 3rd surgery, this time focused on my calves. I’m so excited to get the next phase rolling, and hoping that the world calms down and allows for safe travel soon!
My first and second surgery recoveries were actually extremely different. While the overall process and the surgeries themselves were all the same, I needed a week to recover the first time, and about two weeks to recover the second time. My backside was a bit harder to recover from due to the large volume of fat that was taken, and simply because sitting and laying down was more uncomfortable. I was able to drive, work, and get back to most of my routine within a few days, but I preferred to take it easy for the full two weeks because I was still leaking tumescent fluid, and putting on those compression garments is tough for the first two weeks (more like the first 6 weeks, just to set your expectations…) – I preferred to do this in the comfort of my home for as long as possible.


Interestingly, in the first surgery, I had a lot of numbness on the inside of my thighs, which lasted about a month. Numbness is completely normal after liposuction as your nerves start to heal, so it wasn’t necessarily worrisome, but it was uncomfortable. It made walking extremely uncomfortable and, to the delight of my friends and family, I waddled like a duck for several weeks. So even though I spent more time on the couch after my second surgery, I still “enjoyed” it far more than the first. It’s just proof that every area of the body and every patient is different. But I loved the end results of both!
As I sit here today, I find myself in a funny limbo in regards to living with my lipedema. The already-treated areas of my legs are doing great! No bruising, no swelling, and no sensitivity at all. In fact, my thighs even feel different to the touch – the remaining fat (I’m no bodybuilder yet, haha) is soft and fluffy – something I’ve never experienced before. The only fat I’ve ever encountered has been dominated by my lipedema fat – firm or tight, bulging, and sore.
But because I’m mid-treatment overall, the remaining areas of my body are still very much experiencing the pain of lipedema. The tops of my legs are great, and the bottom of my legs are struggling. My arms and abdomen are progressing and gaining more fluid and lipedema fat. As I work out, I get excited to see small changes in my thighs and depressed seeing no changes in the other parts of my body. When I bump into something with my calf and I get a pang of pain, I get angry and then grateful when I realize I can’t remember the last time I felt that in my thighs. It’s so many mental and physical feelings and changes all at once!
There are so many things that anyone outside of the lippy community wouldn’t think twice about but have had a profound and positive impact on my life post-surgery.
As I move into my next three surgeries, I’m sure I’ll have more updates! But until then, what questions do you have about my lipedema journey or the general process for getting treatment? Leave a comment or contact Dr. Wright and his team, and we’d be more than happy to put together more resources for you! We’re all in this together!
All the best,
Cat
Still unsure if you have Lipedema? Worried about all the unknowns of seeking treatment? You’re not alone! Meet Cat, one of the numerous women with lipedema, Dr. Wright’s patient who travels from Austin, Texas to St. Louis to complete her five scheduled lipedema surgeries. Cat is a writer, a women’s health advocate, and has a passion for documenting her journey and helping other women through it. As long as she can remember, Cat has struggled with her weight. She was never considered an obese child or teen, was active in sports from a young age, and trained and ran half marathons as an adult. Still, though, she found herself struggling with her weight and living with debilitating pain. She spent her summers avoiding the outdoors (because that meant she had to wear shorts or be miserable), never participated in beach or pool trips, and lived a daily struggle of physical and emotional pain.


Not knowing any different, her family explained her issues away, helplessly insisting that she naturally had a “pear body shape”, which ran in her family. She bruised constantly, which was diagnosed as anemia. While she is slightly anemic, Cat has reported that her bruising and painful-to-the touch legs have improved drastically after only two surgeries on her lower body. After years of doctors telling her she was overweight and needed to continue to cut down her calories, Cat was at a loss. Below are her experiences, which she’ll continue to update through the remaining surgeries and recovery process.
Lipedema Ruined & Saved This Fat Girl’s Life
In her first blog post related to Lipedema, Cat writes of her journey towards diagnoses, which ultimately led her to Dr. Wright’s office in 2019.
When the Solution is More Painful Than the Problem
After her initial consultation and diagnosis, Dr. Wright and his team put a treatment plan together for Cat. Her first surgery was in December 2019, and this article outlines what she experienced before, during, and after treatment.
Stay tuned for more! Cat recently completed her 2nd surgery on her upper legs and will be reporting back to detail her experiences. Lipedema is estimated to affect 10% of all women across the world – you’re far from alone, and we’re here to help you through this process to a more fulfilling, healthy, and pain-free life.