June is Lipedema Awareness Month, a time dedicated to raising awareness, providing resources, sharing knowledge, and advocating for equitable healthcare for patients with this complicated, misunderstood, and often misdiagnosed disease. This article will explore the history of lipedema, its symptoms, stages, diagnosis, treatment options, and the importance of research and awareness campaigns. By understanding the key aspects of lipedema and its management, we can help support those affected by the condition and contribute to a more informed and inclusive healthcare system.
Lipedema is a fat disorder that mainly affects women and causes enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
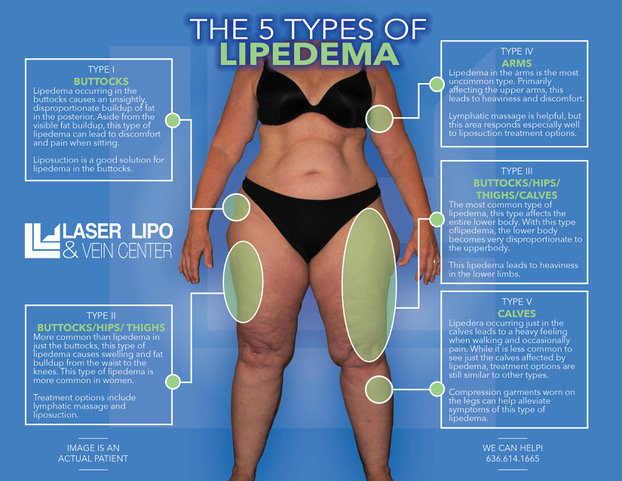
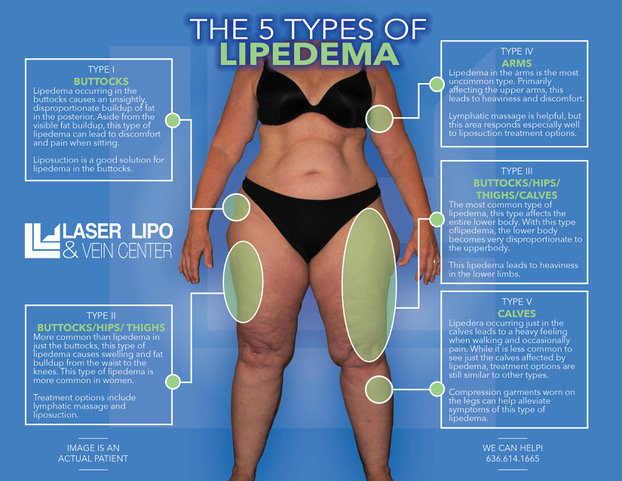
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Medical professionals often misdiagnose and dismiss lipedema as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
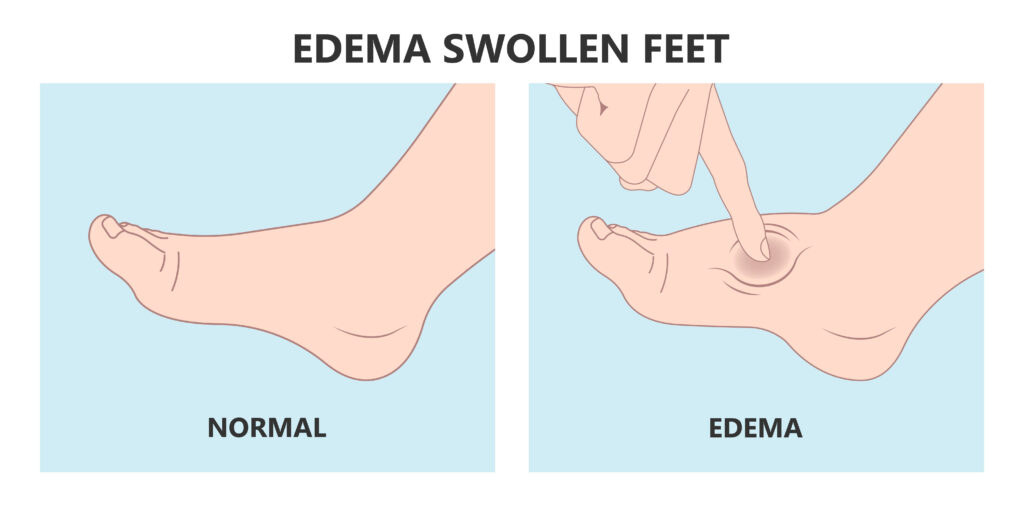
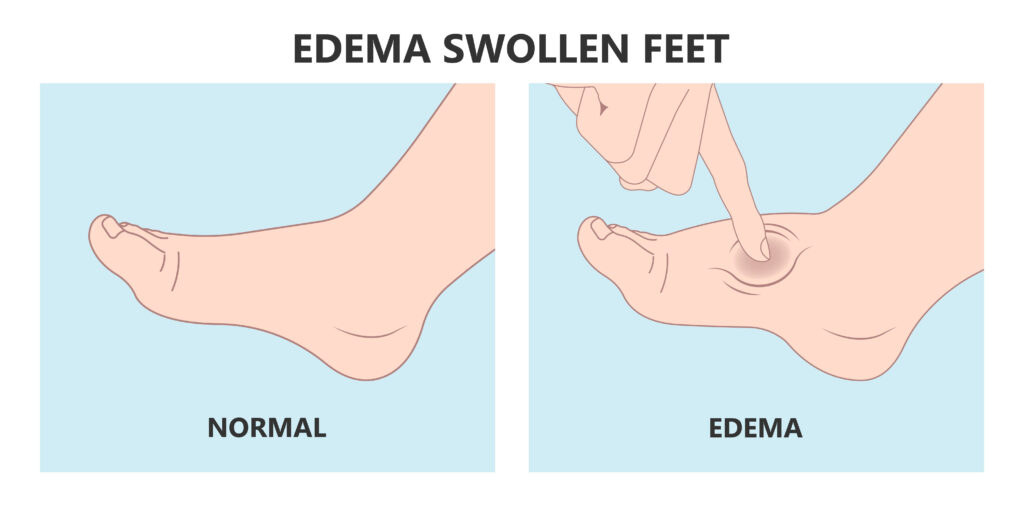
Women suffering from Lipedema often report the disease associated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.
Lipedema is characterized by an abnormal accumulation of fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected, but the condition can also spread to the torso and arms. Symptoms of lipedema can be debilitating, and the fat cells associated with the condition are resistant to both diet and exercise programs.
Some common symptoms of lipedema include:
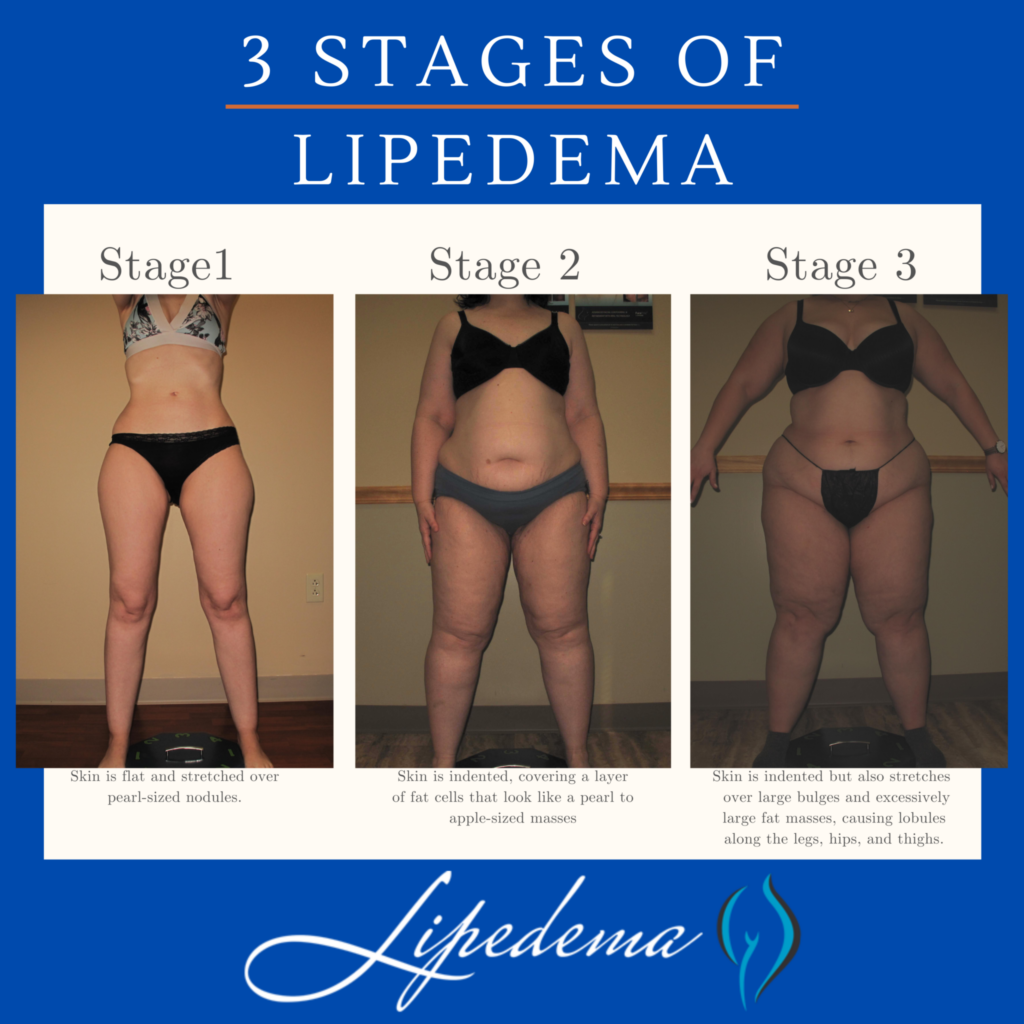
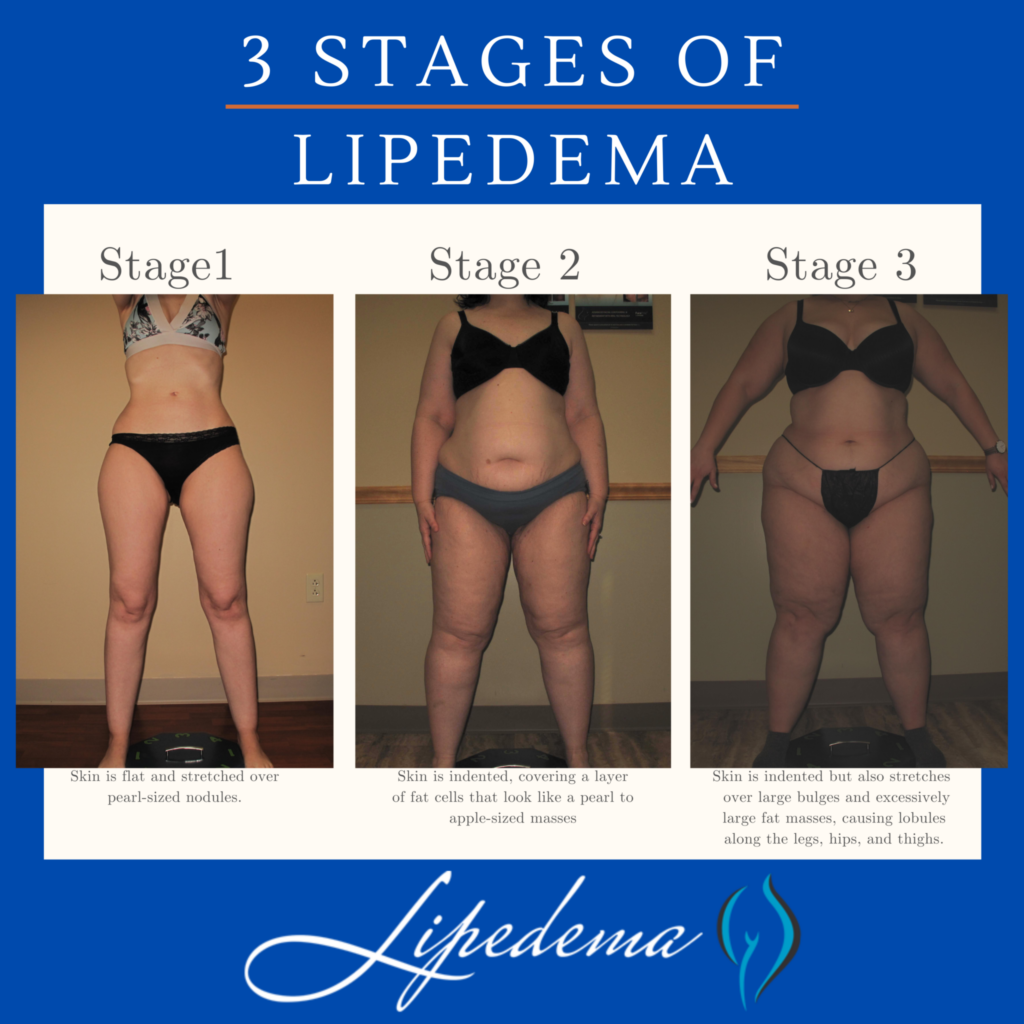
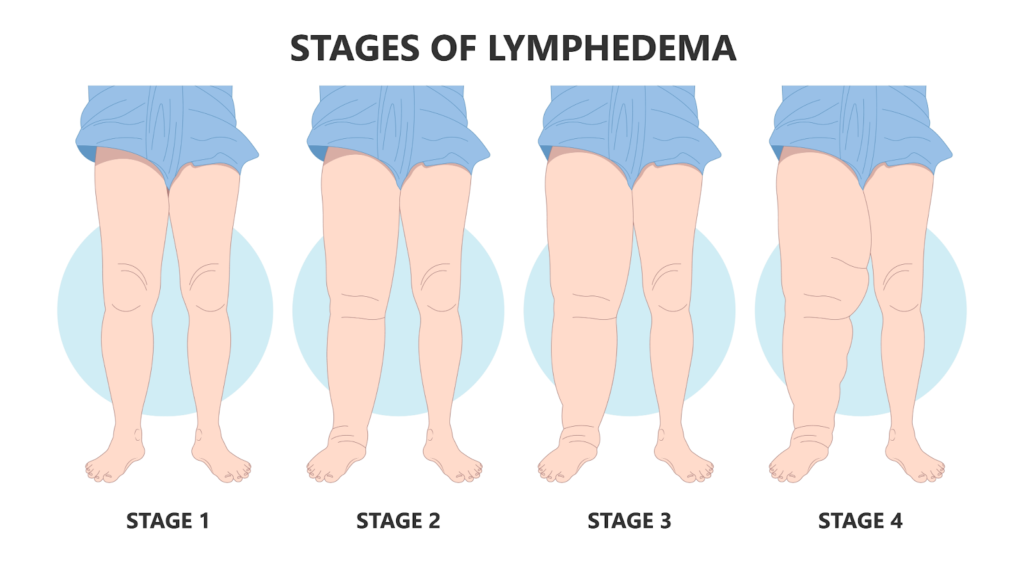
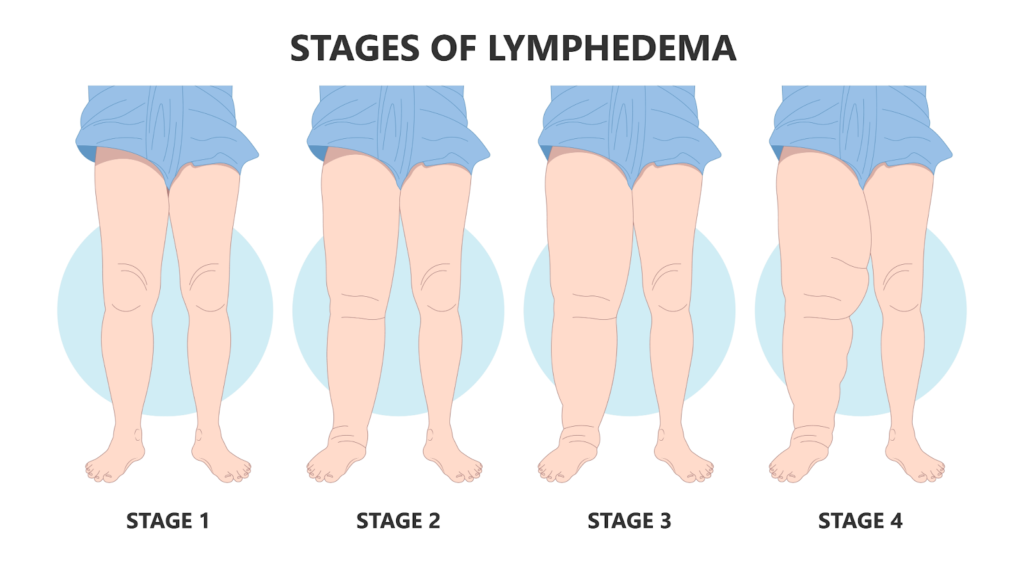
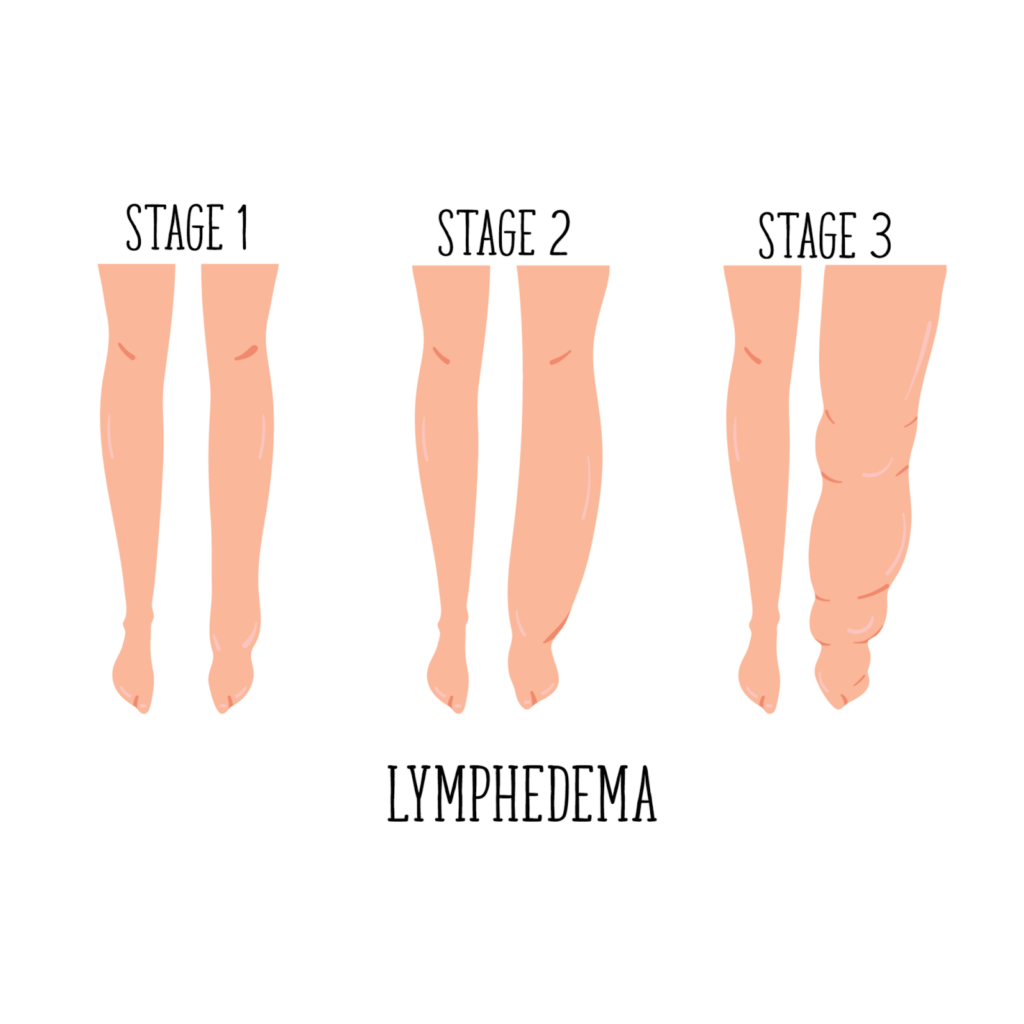
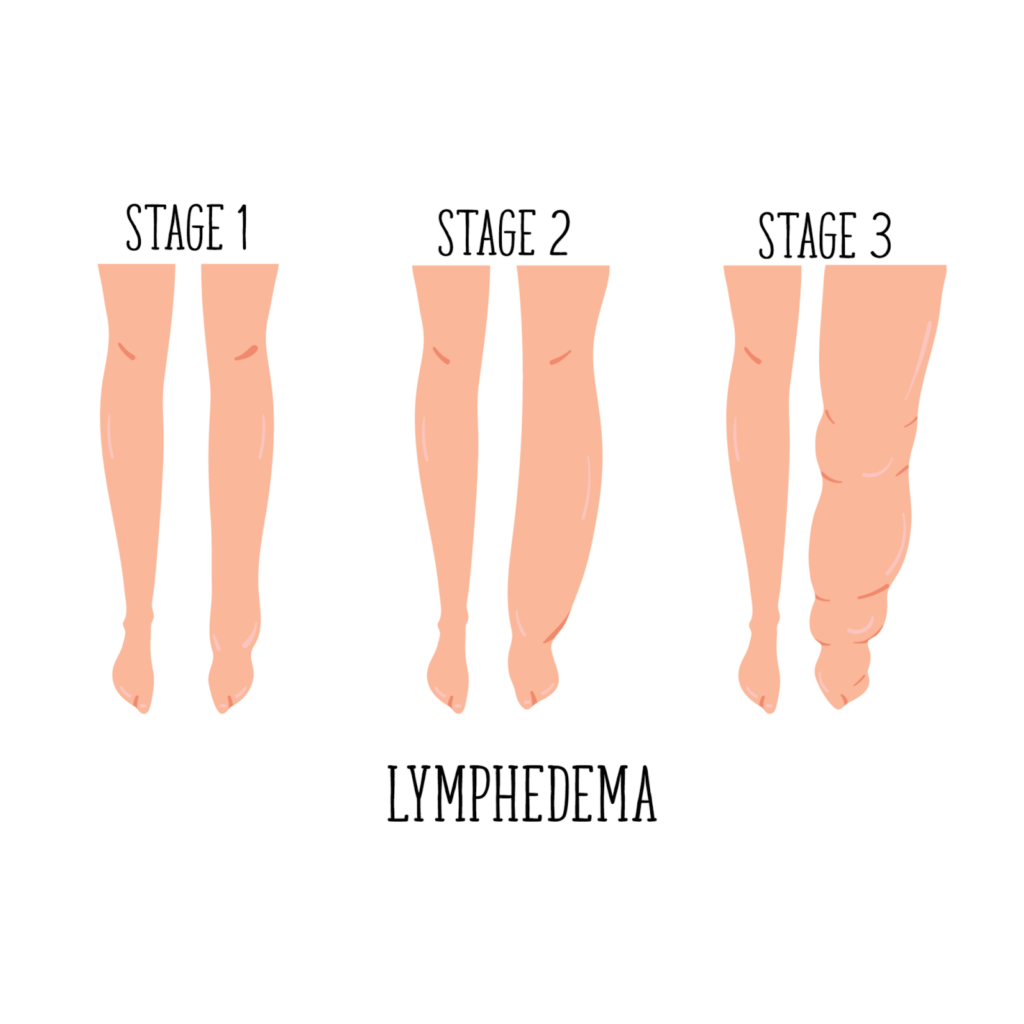
Lipedema progresses through three distinct stages, each with its own set of characteristics:
Several conditions can present similar symptoms to lipedema, making accurate diagnosis challenging. These conditions include:
Obtaining a correct lipedema diagnosis is crucial for effective treatment and management. Diagnosis typically involves a combination of a physical exam, patient questionnaires, and additional testing, such as ultrasounds or Doppler imaging. Some diagnostic tests used to differentiate lipedema from related conditions include:
While there is no definitive cure for lipedema, several treatment options can help manage the condition and improve the patient’s quality of life. These treatments may include:


Liposuction: This surgical intervention removes excess fat deposits and may provide long-term relief for some lipedema patients. However, it should be considered in consultation with a qualified healthcare professional and as part of a comprehensive treatment plan.


Despite being identified over 80 years ago, lipedema remains under-researched and poorly understood. Increased research efforts can lead to improved diagnostic techniques, better treatment options, and a deeper understanding of the condition’s underlying causes. Lipedema Awareness Month serves as an opportunity to raise awareness of the condition, educate healthcare professionals and the public, and support ongoing research initiatives.
There are several ways to participate in Lipedema Awareness Month and support patients living with the condition:
Lipedema Awareness Month is a crucial time for raising awareness, providing resources, and advocating for patients living with this often misunderstood and misdiagnosed condition. By educating ourselves and others, supporting research efforts, and promoting inclusive healthcare policies, we can contribute to a more informed and compassionate healthcare system for all those affected by lipedema.
Lymphedema is a condition that causes swelling in the limbs due to a buildup of lymph fluid. Various factors, including surgery, radiation therapy, and infection, can cause it. While lymphedema can be managed with proper treatment and self-care, traveling can present unique challenges for those with the condition. This article will discuss some tips for traveling with lymphedema to help you stay comfortable and healthy on your next trip.
Lymphedema is a condition that affects the lymphatic system, which is responsible for draining excess fluid from the body’s tissues. When the lymphatic system is not working properly, fluid can build up in the limbs, causing swelling and discomfort. This can make it challenging to move around and perform daily activities and increase the risk of infection.
For those with lymphedema, traveling can exacerbate these symptoms. Long periods of sitting or standing can cause fluid to pool in the limbs, leading to increased swelling and discomfort. Changes in altitude during air travel can also affect the lymphatic system, making it more difficult for the body to drain excess fluid.
Fortunately, there are several steps you can take to manage lymphedema while traveling. Here are some tips to help you stay comfortable and healthy on your next trip:
Before you travel, plan ahead to ensure you have everything you need to manage your lymphedema. This may include compression garments, bandages, or other medical supplies. If you are traveling by air, it is also a good idea to contact the airline ahead of time to request special accommodations, such as extra legroom or assistance with boarding.


Staying hydrated is important for everyone, but it is especially important for those with lymphedema. Drinking plenty of water can help to flush excess fluid from the body and reduce swelling. Bring a refillable water bottle with you and drink plenty of fluids throughout your trip.
Sitting or standing for long periods can cause fluid to pool in the limbs, leading to increased swelling and discomfort. To prevent this, try to move around as much as possible during your trip. Take frequent breaks to stretch your legs, walk around the cabin during a flight, or stop at rest areas during a road trip to get out and move around.
Compression garments are designed to help improve circulation and reduce limb swelling. If you have lymphedema, wearing compression garments can be especially helpful during travel. Wear your compression garments as directed by your healthcare provider and pack extra pairs in emergencies.


Elevating your legs can help reduce swelling and improve limb circulation. If you are traveling by car or train, try to elevate your feet on a pillow or blanket. If traveling by air, consider booking a seat with extra legroom or bringing an inflatable footrest to help elevate your legs during the flight.
Tight clothing can restrict circulation and exacerbate lymphedema symptoms. When packing for your trip, choose loose-fitting clothing that is comfortable and allows for easy movement. Avoid tight socks, stockings, or other clothing that may restrict limb circulation.
Traveling with lymphedema can be challenging, but with proper planning and self-care, staying comfortable and healthy on your next trip is possible. Remember to plan ahead, stay hydrated, move around as much as possible, wear compression garments, elevate your legs, and avoid tight clothing. Following these tips allows you to enjoy your travels without letting lymphedema symptoms get in the way.
On March 6th, we honor and celebrate the awareness, understanding, and support of those with lymphedema. Lymphedema is a chronic condition that is often overlooked, and World Lymphedema Day was created to bring awareness to this condition and support those living with it.
March is Lymphedema Awareness month, a time to put on your light blue ribbon and find creative ways to participate in educating the world on lymphatic diseases. The highlight of the month, World Lymphedema Day, falls on March 6th this year. The Lymphatic Network hosts a wide range of events worldwide for the community to participate in digitally and in person. Sign up for events and presentations on their home page, or use their guide to getting involved and participating on World Lymphedema Day. The clinical, patient, and advocacy communities and the private sector join forces all month long to increase awareness of this chronic condition.
The United States Senate established World Lymphedema Day in 2016 in response to a Senate bill written by the Lymphatic Education & Research network. Advocates celebrate each March annually, with the primary focus on educating the world on all lymphatic diseases: primary and secondary lymphedema (LE), lipedema (LI), lymphatic filariasis (LF), lymphatic malformations (LM), and the full lymphatic continuum (LC) of diseases impacted by the lymphatic system.
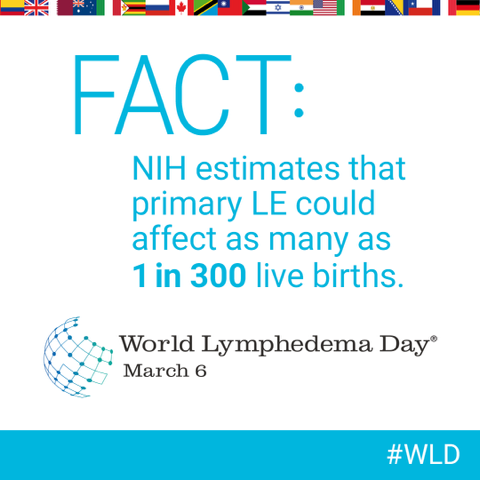
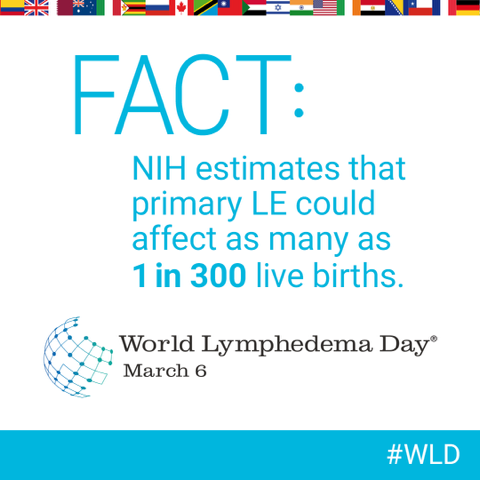
Lymphedema is when excess fluid accumulates in the body’s tissues, causing swelling. It can develop when the lymphatic system, which helps move fluid to the bloodstream, is damaged or blocked. There are two types of lymphedema: primary lymphedema, which is caused by a genetic disorder, and secondary lymphedema, which is caused by an injury or medical condition. Lymphedema can affect any body part but is most commonly found in the arms and legs.
Lymphedema is a condition that occurs when lymphatic fluid, a transparent liquid composed of fat, water, salts, and proteins, begins to pool and accumulate in the arms and the legs. The initial and most predominant symptom indicating the presence of Lymphedema is significant swelling of these extremities. Medical experts point to damaged lymph vessels as the cause behind fluid retention leading to Lymphedema.. Other potential causes for fluid retention are linked to infections, genetics or underlying medical conditions, especially cancer and its treatment. Keep reading to learn more about the treatment of Lymphedema in St Louis.
The most common cause of lymphedema is damage to the lymph nodes or lymph vessels due to cancer treatments such as radiation and chemotherapy. Other causes of lymphedema include surgery, trauma, infection, and other medical conditions such as congestive heart failure or cirrhosis of the liver.
In some cases, the cause of lymphedema is unknown. This is called idiopathic lymphedema. It is most often seen in women over the age of 50.
The most common symptom of lymphedema is swelling in the affected area. This swelling can be mild or severe and can range from a feeling of heaviness to visible swelling. Other symptoms of lymphedema include pain, tightness, aching, and stiffness in the affected area. In some cases, lymphedema can also cause changes in the skin, such as thickening, discoloration, and itching.


It is widely understood and accepted that Lymphedema can be an inherited medical condition and, as a result, is recognized under three distinct categories. Congenital Lymphedema refers to symptoms that develop in early childhood. Lymphedema Praecox refers to symptom development that occurs during adolescence, while Lymphedema Tarda refers to symptoms that show up in patients later in life. Lymphedema quite commonly develops in patients due to a traumatic injury damaging lymphatics. This type of trauma is generally linked to removing lymph nodes during surgical procedures related to cancer treatment or radiation. Infection is a second factor closely linked to the development of Lymphedema.
The treatment of lymphedema depends on the type and severity of the condition. Mild cases of lymphedema can often be managed with lifestyle changes such as maintaining a healthy weight, exercising regularly, and avoiding repetitive activities that can cause further damage to the lymphatic system.


For more severe cases of lymphedema, treatments such as manual lymphatic drainage, compression garments, and physical therapy can be used to reduce swelling and improve the function of the lymphatic system. Surgery may sometimes be necessary to remove excess fluid and reduce swelling.
In addition to World Lymphedema Day, March is also Lymphedema Awareness Month. This is a necessary time to spread awareness about lymphedema and to support those living with the condition. There are several ways to get involved, from attending events and spreading the word on social media to donating to organizations that support lymphedema research.
The color for World Lymphedema Day is blue, and the lymphedema awareness ribbon is silver. Wearing these colors can be a great way to show your support for those living with lymphedema.
There are many ways to celebrate World Lymphedema Day. One of the best ways is to spread awareness and educate others about the condition. You can do this by talking to your friends and family about lymphedema, sharing posts on social media, attending events, and donating to organizations that support lymphedema research.
Another way to show your support is to wear blue and the lymphedema awareness ribbon on March 6th. This is a great way to raise awareness and show your support.
And finally, remember to reach out to those living with lymphedema. A simple message of support can go a long way in helping those living with this condition feel seen and heard.
Several great resources are available if you want to learn more about lymphedema. The National Lymphedema Network is a great place to start, as they provide information about the condition, resources for finding treatment, and support for those living with lymphedema.
The Lymphatic Education and Research Network is another excellent resource. They provide a wealth of information about lymphedema, from the latest research to support groups and resources for care and treatment.
World Lymphedema Day is an important day for honoring and celebrating those living with lymphedema. It is a day to raise awareness and support those living with the condition. There are many ways to get involved in celebrating World Lymphedema Day, from spreading awareness to reaching out to those living with the condition. We hope that you will join us in celebrating World Lymphedema Day! Contact Laser Lipo and Vein Center to schedule a consultation!
Good news, these conditions are not life-threatening on their own. However, if undiagnosed or untreated, they will worsen over time and may contribute to several other secondary ailments and complications. If you have signs of swelling, and pain in your body, especially in your legs and arms, seek treatment starting with your primary care physician. Ongoing care of lipedema and lymphedema with a vascular expert lessens the risk of other serious problems.
For instance:
Remember, you are in control of how you manage your health and well-being. Educate yourself and do not hesitate tol ask for help. A great resource for emotional support from the comfort of your home is https://www.mind-diagnostics.org. A study by researchers at the University of California, Berkeley found online counseling can be just as effective as face-to-face therapy while being more convenient, affordable, and accessible.
Sources:
https://www.healthgrades.com/right-care/symptoms-and-conditions/lymphedema
https://my.clevelandclinic.org/health/diseases/8353-lymphedema
https://www.nhs.uk/conditions/postural-tachycardia-
syndrome/#:~:text=Postural%20tachycardia%20syndrome%20(PoTS)%20is,as%20postural%20orthostati
c%20tachycardia%20syndrome
https://www.aapmr.org/about-physiatry/conditions-treatments/pain-neuromuscular-medicine-
rehabilitation/degenerative-joint-disease
https://www.nhs.uk/mental-health/conditions/body-
dysmorphia/#:~:text=Body%20dysmorphic%20disorder%20(BDD)%2C,affects%20both%20men%20and%
20women.
https://www.betterhelp.com/study/Study_of_BetterHelp_eCounseling.pdf
Through efforts led by LE&RN (the Lymphatic Education & Research Network), the Senate has passed a bill for the LD Commission (Lymphatic Disease Commission) to increase research and lymphatic education. The bill passed in the Senate last month, with a vote of 68-31. Now that it’s passed in both houses of Congress, it is now on President Biden’s desk to be signed into law. This is exciting and unprecedented news for men and women suffering from lymphatic diseases!
Video: LE&RN’s Appeal to Congress video here.
The following language is taken directly out of the recently passed bill and is a direct reflection of the hard work and dedication of advocates in this community. NHLBI refers to the National Heart, Lung, and Blood Institute and NIH refers to the National Institute of Health, two of the nation’s medical research agencies that support scientific studies for advancing knowledge and discovery in health.
Lymphedema (LE)—The agreement directs NHLBI to increase support for research on LE and to establish a Research Condition Disease Categorization category for research related to lymphedema.
National Commission on Lymphatic Diseases—The agreement directs NIH to establish a National Commission on Lymphatic Diseases and to engage with relevant Institutes, Centers, and external stakeholders in establishing this Commission. The agreement directs NIH to provide an update on progress to establish the Commission within 60 days of the enactment of this Act.


This is the latest step in pushing for resources for deeper research into the causes, best treatment practices, and even genetic dispositions for lymphatic diseases that are not yet clearly identified across healthcare. A National Commission on Lymphatic Diseases pushes Lymphatic Diseases to the forefront of national research as a priority, and ultimately this gives experts in this field a seat at the table to tell Congress what we need in order to provide the best care to patients. Most exciting, the bill now directs NIH to establish this Commission within the next two months after President Biden signs!
Lymphedema is a condition that occurs when lymphatic fluid, a transparent liquid composed of fat, water, salts, and proteins, begins to pool and accumulate in the arms and the legs. The initial and most predominant symptom indicating the presence of Lymphedema is significant swelling of these extremities. Medical experts point to damaged lymph vessels as the cause of fluid retention leading to Lymphedema. When lymphatic fluid isn’t able to properly circulate through the human bloodstream via lymph nodes and vessels, retention quickly occurs. Other potential causes for fluid retention are linked to infections, genetics or underlying medical conditions especially cancer and its treatment. Keep reading to learn more about the treatment of Lymphedema in St Louis.
It is widely understood and accepted that Lymphedema can be an inherited medical condition and as a result, is recognized under three distinct categories. Congenital Lymphedema refers to symptoms that develop in early childhood. Lymphedema Praecox refers to symptom development that occurs during adolescence, while Lymphedema Tarda refers to symptoms that show up in patients later in life. Lymphedema quite commonly develops in patients as a result of a traumatic injury damaging lymphatics. This type of trauma is generally linked to the removal of lymph nodes during surgical procedures related to cancer treatment or radiation. Infection is a second factor closely linked to the development of Lymphedema.
This is a widespread side effect in patients with lymphedema, where the skin hardens over time. In the early stages of lymphedema, swelling is soft to the touch. However, over time, the swelling hardens the skin due to the development of connective tissue fibers underneath the skin of the affected areas.
The growth of numerous papillomas, more commonly referred to as warts.
Hardening and tightening of the skin and connective tissues.
Leg swelling is one of the most common symptoms of lymphedema and prompts patients to seek treatment.


Lymphedema is a progressive condition that can quickly transform into a more serious medical issue. The risks of leaving Lymphedema untreated can include a heightened vulnerability to infection leading to lymphangitis and cellulitis. Similarly, Lymphedema can commonly lead to fibrosis or hardening and scarring of the skin and subcutaneous fat cells. This condition has the potential to impede the overall circulation of lymph fluid causing physical movement to become a painful task. These conditions comprehensively increase the pressure put on veins working to move blood through the body towards the heart.
A physical exam will be carried out and the results compared to the patient’s medical history and profile. A venous doppler ultrasound is commonly utilized to assess the potential for venous insufficiency which can also lead to increased swelling of the limbs. To verify the presence of Lymphedema, a physician may choose to perform a Lymphoscintigraphy. This procedure involves the injection of a radioactive solution into the potentially affected area of the body to decisively map the path of lymphatic fluids in a targeted region. The option for the physician to perform a Lymphangiography involves the replacement of the radioactive solution with a medicinal dye.
Patients suffering from Lymphedema are at a greater risk of developing infections and there are some simple home care strategies that help diminish the overall risk factor. Those suffering from Lymphedema should always completely dry affected limbs after showering or swimming. Wearing protective shoes and clothing reduces the risk of cuts or injuries while the addition of compression garments is highly recommended in the promotion of healthy blood circulation. Sitting with the legs uncrossed is another simple strategy towards promoting improved lymphatic flow. Maintaining a dedicated exercise routine along with a healthy diet has been shown to help reduce the risk of injury or infection related to Lymphedema.
While there is no permanent cure for Lymphedema, complications, and progression of the disease can be managed effectively with a combination of Lymphedema treatment St Louis options. Compression garments are the primary method recommended for managing Lymphedema. Compression stockings, sleeves, leggings, and gauntlets provide the first line of defense when it comes to promoting healthy blood circulation. Manual lymphatic drainage or massage can aid in the management of Lymphedema as well. This technique works to manually move the lymph out of congested areas. When this type of massage is combined with compression bandages the treatment method may be referred to as Complete Decongestive Therapy.
For patients with more severe cases of Lymphedema, intermittent compression pump lymphedema therapy may prove effective. These compression pumps actively work to move trapped lymphatic fluid through the lymphatic circulatory system.
March is Lymphedema Awareness month, a time to put on your light blue ribbon and find creative ways to participate in educating the world on lymphatic diseases. The highlight of the month, World Lymphedema Day, falls on March 6th this year. The Lymphatic Network hosts a wide range of events all around the world for the community to participate in, both digitally and in person. Sign up for events and presentations on their home page, or use their guide to getting involved and participating on World Lymphedema Day. All month long, the clinical, patient, and advocacy communities, as well as the private sector, join forces to increase awareness of this chronic condition.
World Lymphedema Day was established by the United States Senate in 2016 in response to a Senate bill written by the Lymphatic Education & Research network. Advocates celebrate annually each March, with the primary focus on educating the world on all lymphatic diseases: primary and secondary lymphedema (LE), lipedema (LI), lymphatic filariasis (LF), lymphatic malformations (LM), and the full lymphatic continuum (LC) of diseases impacted by the lymphatic system.
Lymphedema is a condition that occurs when lymphatic fluid, a transparent liquid composed of fat, water, salts, and proteins, begins to pool and accumulate in the arms and the legs. The initial and most predominant symptom indicating the presence of Lymphedema is significant swelling of these extremities. Medical experts point to damaged lymph vessels as the cause behind fluid retention leading to Lymphedema. When lymphatic fluid isn’t able to properly circulate through the human bloodstream via lymph nodes and vessels, retention quickly occurs. Other potential causes for fluid retention are linked to infections, genetics or underlying medical conditions especially cancer and its treatment. Keep reading to learn more about the treatment of Lymphedema in St Louis.


Individuals suffering from Lymphedema often report experiencing swelling of the limbs which tends to be more significant on one side of the body as compared to the other. Additionally, those struggling with Lymphedema may experience fatigue, heaviness, tightness, or lack of flexibility affecting the limbs that are swollen. Inflammation and redness of the arms and legs are common symptoms associated with Lymphedema.
It is widely understood and accepted that Lymphedema can be an inherited medical condition and as a result, is recognized under three distinct categories. Congenital Lymphedema refers to symptoms that develop in early childhood. Lymphedema Praecox refers to symptom development that occurs during adolescence, while Lymphedema Tarda refers to symptoms that show up in patients later in life. Lymphedema quite commonly develops in patients as a result of a traumatic injury damaging lymphatics. This type of trauma is generally linked to the removal of lymph nodes during surgical procedures related to cancer treatment or radiation. Infection is a second factor closely linked to the development of Lymphedema.
Lymphedema is a progressive condition that can quickly transform into a more serious medical issue. The risks of leaving Lymphedema untreated can include a heightened vulnerability to infection leading to lymphangitis and cellulitis. Similarly, Lymphedema can commonly lead to fibrosis or hardening and scarring of the skin and subcutaneous fat cells. This condition has the potential to impede the overall circulation of lymph fluid causing physical movement to become a painful task. These conditions comprehensively increase the pressure put on veins working to move blood through the body towards the heart.
A physical exam will be carried out and the results compared to the patient’s medical history and profile. A venous doppler ultrasound is commonly utilized to assess the potential for venous insufficiency which can also lead to increased swelling of the limbs. To verify the presence of Lymphedema, a physician may choose to perform a Lymphoscintigraphy. This procedure involves the injection of a radioactive solution into the potentially affected area of the body to decisively map the path of lymphatic fluids in a targeted region. The option for the physician to perform a Lymphangiography involves the replacement of the radioactive solution with a medicinal dye.
Patients suffering from Lymphedema are at a greater risk of developing infections and there are some simple home care strategies that help diminish the overall risk factor. Those suffering from Lymphedema should always completely dry affected limbs after showering or swimming. Wearing protective shoes and clothing reduces the risk of cuts or injuries while the addition of compression garments is highly recommended in the promotion of healthy blood circulation. Sitting with the legs uncrossed is another simple strategy towards promoting improved lymphatic flow. Maintaining a dedicated exercise routine along with a healthy diet has been shown to help reduce the risk of injury or infection related to Lymphedema.


While there is no permanent cure for Lymphedema, complications, and progression of the disease can be managed effectively with a combination of Lymphedema treatment St Louis options. Compression garments are the primary method recommended for managing Lymphedema. Compression stockings, sleeves, leggings, and gauntlets provide the first line of defense when it comes to promoting healthy blood circulation. Manual lymphatic drainage or massage can aid in the management of Lymphedema as well. This technique works to manually move the lymph out of congested areas. When this type of massage is combined with compression bandages the treatment method may be referred to as Complete Decongestive Therapy.
For patients with more severe cases of Lymphedema, intermittent compression pump lymphedema therapy may prove effective. These compression pumps actively work to move trapped lymphatic fluid through the lymphatic circulatory system.
Swelling of the arms and legs is generally the first symptom of Lymphedema but can also be linked to underlying venous insufficiency. When this is the case, seeking vein treatment options can significantly improve symptoms associated with Lymphedema. Dr. Wright and his team at the St. Louis Laser Lipo and Vein Center provide comprehensive Lymphedema therapy plans that take a patient’s full medical profile into consideration. When you’re looking for solutions to treat symptoms of Lymphedema of underlying vein disease, make sure to contact us to set up an initial consultation.
Currently, most of the supplies needed to manage lipedema and lymphedema are not covered by Medicare. Compression garments, donning devices and wraps, which are critical for the proper care and management of these diseases are not covered except when caused by cancer treatment. These garments are quite expensive and need to be replaced as often as every six months. The lymphedema can be just devastating when caused by an inherited condition as is the case of lipedema or an infection. If lymphedema is not properly controlled by compression garments it progress and spiral into a progressively disabling condition.
The Lymphedema Treatment act will improve coverage for lymphedema from any cause from Medicare. Other insurance will follow Medicare lead. This legislation is critical for improving the health and lives of patients who suffer from lymphedema. There is much to do. Please follow these links to learn how you can contact your representative in the US Congress and Senate. Also, learn how to promote awareness for this important cause through social media.