The Development and Validation of Lipedema Reduction Surgery
Lipedema is a connective tissue disease affecting subcutaneous adipose tissue (SAT) that has long puzzled the medical community. First identified by Drs. Alan and Hines in 1940, lipedema is characterized by painful, swollen limbs due to disproportionate fat accumulation, often triggered by hormonal changes. This condition predominantly affects women and can significantly impact their quality of life.
Traditional Approaches to Lipedema Management
Initially, lipedema management was conservative, involving compression garments, manual lymphatic drainage (MLD), and dietary guidance. However, while these methods provided some relief, they required ongoing commitment to therapy and were not definitive solutions. Many patients continued to experience discomfort and were left seeking more effective treatments.
Breakthrough with Liposuction: The First Lipedema Reduction Surgery
The introduction of liposuction for lipedema treatment marked a significant advancement. This journey began with Dr. Jeff Klein’s development of the tumescent anesthesia technique in the early 1990s. This technique, involving dilute local anesthetic and epinephrine along with small, blunt suction cannulas, minimized blood loss and allowed for outpatient procedures without general anesthesia.
In 1992, Dr. Gerhard Sattler, a dermatology professor at Darmstadt Hospital near Frankfurt, Germany, trained under Dr. Klein. Dr. Sattler, alongside colleagues Dr. Stefan Rapprich and Dr. Manuel Cornely, began to explore the use of this technique for lipedema treatment. At the time, these venous and lymphatics specialists were among the few medical specialists who could recognize and diagnose lipedema. During their practice, which focused on venous and lymphatic disease, they saw many women with lipedema. At that time, there was great concern about the lymphatic damage from liposuction. Their pivotal moment came in 1994 when they decided to perform liposuction on a lipedema patient who was not responding to conservative treatments and stated that she was in great discomfort and insisted on any options for relief from her lipedema pain. The successful outcome of this procedure spurred further interest and experimentation.
Minimizing Lymphatic Damage
Liposuction can cause permanent damage to lymphatic structures, leading to lymphedema. Lymphedema is a serious disease that is not only debilitating but can also cause rare forms of cancer, such as angiosarcoma. These venous and lymphatic specialists were very familiar with liposuction and other surgical causes of lymphedema. It is well known that lipedema itself impairs lymphatic function in affected limbs. The leaders of the lymphedema community were strongly against liposuction on women with lipedema. In his Lymphology textbook in 2006, Dr. Michael Foldi railed against the dangers to lymphatics from liposuction.
“Surgical removal of adipose tissue, lipectomy, can cause lymphedema as a complication because lymph vessels are always removed along with the fat. It is particularly dangerous if fat pads medial to the knee joints are excised – as previously explained, the ventromedial lymph vascular bundle is located in this region. Lymphedema is a much more serious disease than lipedema. People do not die of lipedema, but lymphedema can lead to angiosarcoma. Incidentally, lipectomy is not a minor procedure. The operation can even result in death as a consequence of a fat embolism.” -Dr. Michael Foldi
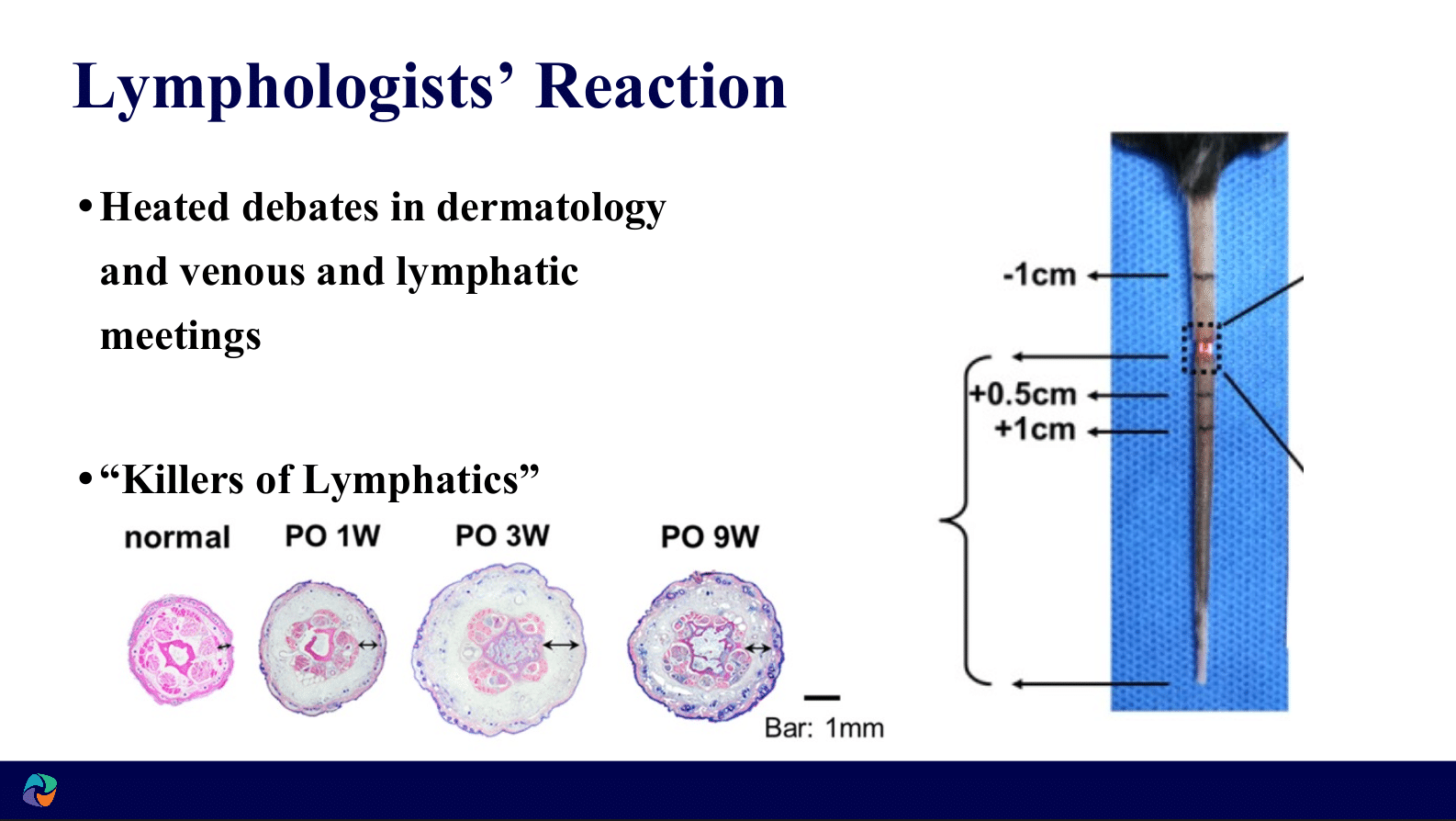
The originators of lipedema reduction surgery, Dr. Sattler, Raprich, Cornely, Stutz, Schmeller, Hoffman & Baumeister took to heart the concerns with the potential for lymphatic damage in liposuction on their lipedema patients.
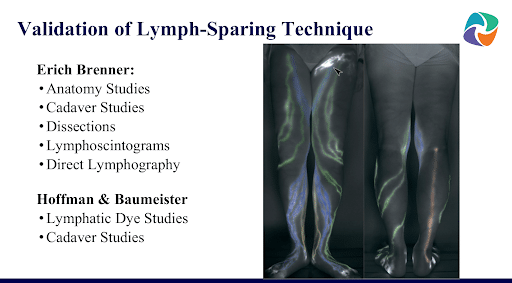
The early dermatologists and lymphatic surgeons like Dr. Sattler and Raprich were cautious and developed surgical techniques to minimize the harm to the lymphatic system. Numerous anatomical studies, lymphatic dye studies, and lymphoscintographic studies were performed to validate the safety and benefits of these new surgical techniques. These studies, published by Baumeister, Hoffman, and Frick in 1999, demonstrated that using tumescent anesthesia and longitudinal cannula strokes significantly reduced the risk of lymphatic damage.
Recognition and Controversy
Despite initial skepticism and controversy, particularly concerns voiced by lymphologists about potential lymphedema, continued research, and positive clinical outcomes gradually convinced the medical community of the procedure’s safety and efficacy. By 2002, Dr. Rapprich presented a study at the 20th World Congress of Dermatology in Paris documenting successful long-term results from tumescent liposuction in lipedema patients.
Ongoing Developments and Global Acceptance
Subsequent studies by various experts, including Dr. Wilfred Schmeller in 2006 and Dr. Josef Stutz in 2007, further validated the safety and benefits of lymphatic-sparing liposuction techniques for lipedema. These studies highlighted pain reduction and improved limb function and quality of life. By the late 2000s, the technique had gained widespread acceptance and was being performed globally.
The Modern Approach
Today, liposuction for lipedema is recognized as a vital treatment option that can significantly improve patient outcomes. Techniques have evolved to minimize the disturbance to the principle lymphatic collectors that drain lymph from the legs and efficiently maximize fat and fibrous tissue removal. This specialized surgical approach is distinct from cosmetic liposuction, focusing on reducing pain and improving function rather than purely aesthetic enhancements.
All the medical literature supporting the safety and benefits of lipedema reduction surgery up until the last few years was published by dermatologists and venous and lymphatic specialists. The dermatologists and venous lymphatic specialists all followed the same surgical techniques, such as longitudinal cannula strokes and generous tumescent anesthesia. The vast majority of the literature and all the literature before 2016 demonstrating the safety and benefits of lipedema reduction surgery used these techniques. Recently, plastic surgeons have taken an interest in treating lipedema. These plastic surgeons have significantly more varied surgical techniques and some take no precautions to avoid disrupting lymphatic collectors. There is much less literature on the outcomes of these surgeries and no long-term literature on the outcomes of these surgeries using the more varied surgical techniques.
Over the last 25 years, studies by dermatologists and venous lymphatic specialists have shown decreased pain, decreased swelling, decreased need for compression and decongestion therapy, and improved quality of life. More recently, in 2023, a new study has shown improved mobility and knee mechanics from lipedema reduction surgery following surgical techniques to limit injury to principal lymphatic collectors.
As we reflect on the history of liposuction for treating lipedema, it is a testament to the relentless pursuit of innovation and understanding in the medical field. The journey from conservative management to advanced surgical interventions illustrates the evolution of care for lipedema patients, offering them a new lease on life free from chronic pain and mobility issues. The Dermatologist and Lymphatic Specialist developed and validated much published evidence of the safety and effectiveness of lipedema reduction surgery using specialized surgical techniques to protect principal collecting lymphatic vessels. There is less evidence for the safety and effectiveness of lipedema surgery performed by plastic surgeons who have recently started treating lipedema, and the limited published evidence that does exist using the newer, more varied, not lymphatic protecting lipedema surgical technique that does exist has shorter follow-ups. Time and further study will tell whether these more varied, less specific surgical techniques will prove safe and effective by the newer surgeons treating lipedema.
In conclusion, lymph-sparing liposuction describes a specific technique with a longitudinal cannula and was developed and validated by dermatologists and lymphatic specialists, including safety and effectiveness studies. The evidence for the effectiveness and safety for this technique has grown exponentially over the years. As the evidence for this specific type of lipedema reduction surgery has grown, new specialties have joined the core specialties of dermatology and lymphatic specialists in treating lipedema surgically. The newer specialties have brought more varied surgical techniques. There is much less evidence for the safety and effectiveness of these new surgical techniques.
Sources:
Frick A, Hoffmann JN, Baumeister RGH, Putz R. Liposuction technique and lymphatic
lesions in lower legs: Anatomic study to reduce risks. Plast Reconstr
Surg 1999;103:1868–73.
Hoffmann JN, Fertmann JP, Baumeister RGH, et al. Tumescent and dry liposuction
of lower extremities: Differences in lymph vessel injury. Plast Reconstr
Surg 2004;113:718–24.
Rapprich S, Loehnert M, Hagedorn M. Therapy of lipoedema syndrome by liposuction
under tumescent local anaesthesia. Ann Dermatol Venereol 2002;129:1S711.
Schmeller W, Meier-Vollrath I. Tumescent Liposuction: A New and Successful Therapy
for Lipedema. Journal of Cutaneous Medicine and Surgery. 2006;10(1):7-10.
doi:10.1007/7140.2006.00006.
