Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat tissue, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells and adjoining connective tissue in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.
Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, discomfort and appearance of Lipedema nodules.
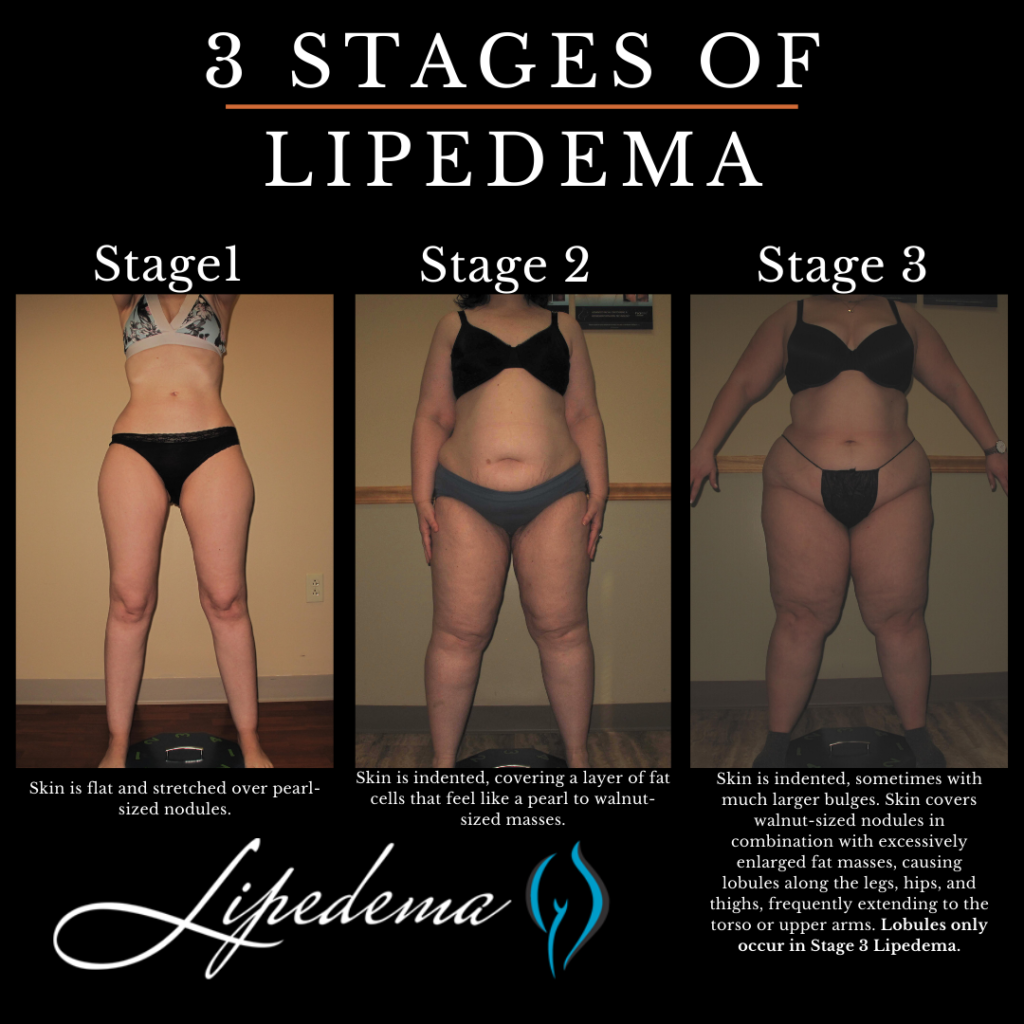
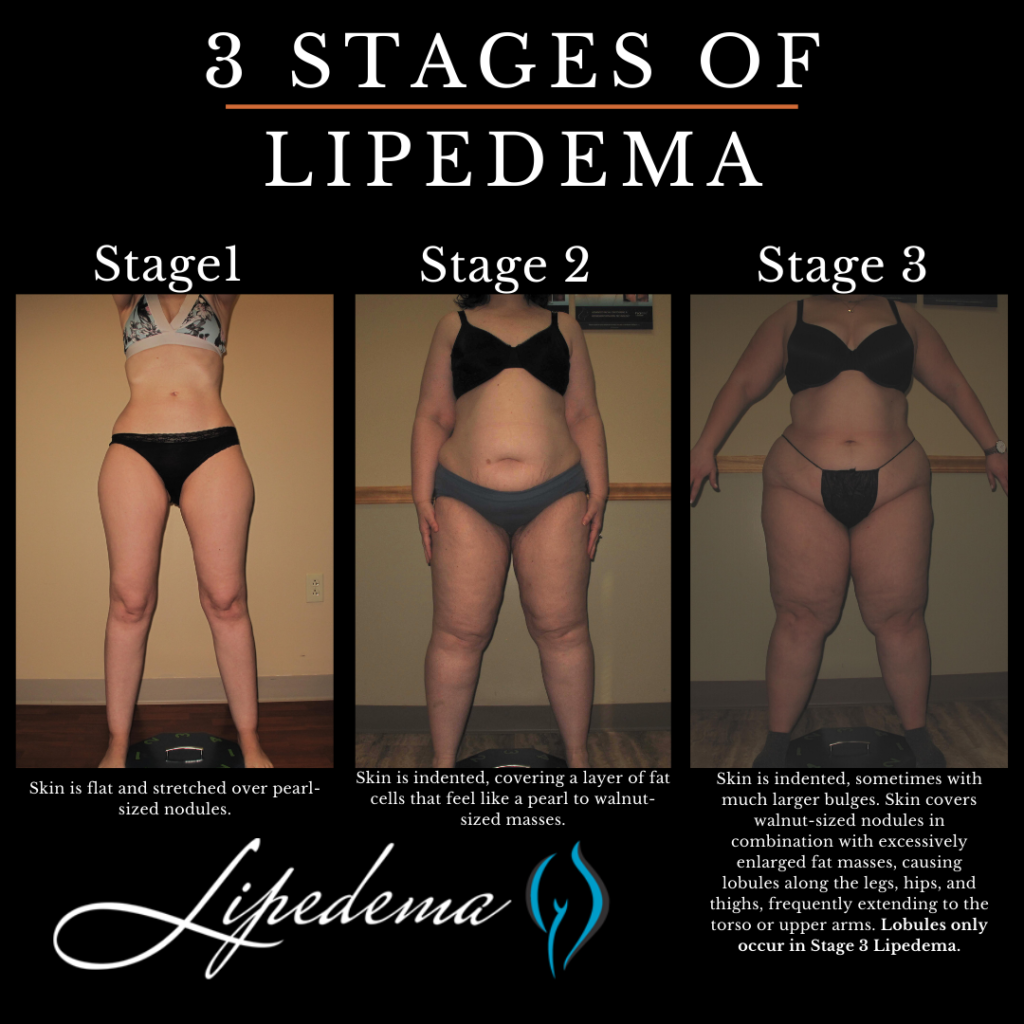
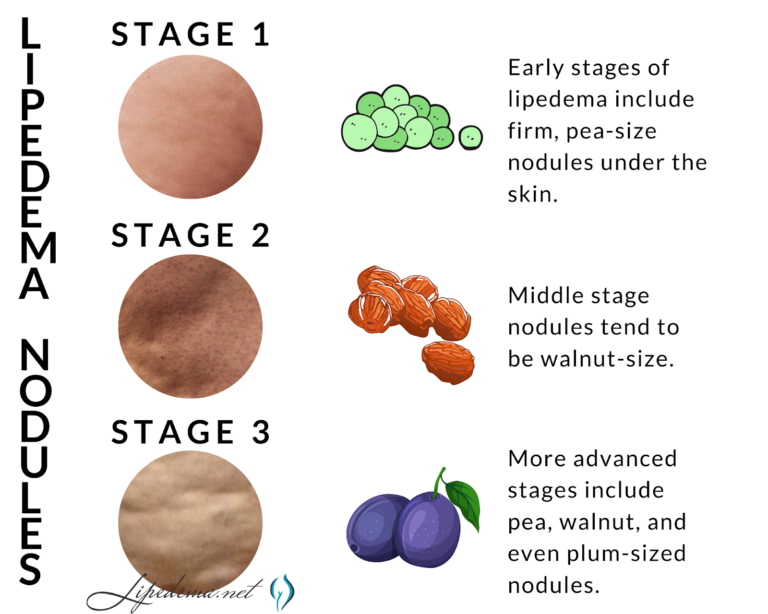
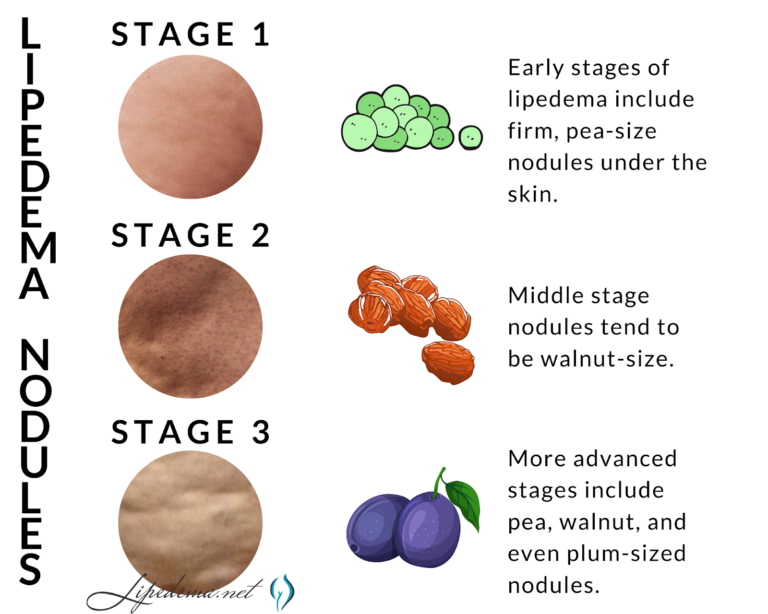
3 Stages of Lipedema Nodules
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like a pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized lipedema nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.
If one of these stages sounds like you, and you checked off multiple items on the list above, you may have Lipedema, but it’s impossible to say for sure. The only way to know for sure is to get a proper Lipedema diagnosis, which in itself is an important process.
What is a lipedema lobule?
In stage 3 lipedema, lobules develop in the skin. The presence of a lobule is one of the most important physical changes to occur in the skin that differentiates stage 2 and stage 3 lipedema. Originally described by Dr. Schmeller, a lobule is defined as a “hanging flap of skin,” also called an “extrusion of skin that protrudes or sticks out from the expected smooth contour of the skin.” Lobules can be seen from a distance. The lobules can occur in many areas on the body in lipedema patients, but the classic areas are just below the knees, or subpatellar lobules, lobules
Lipedema Nodules and Fat
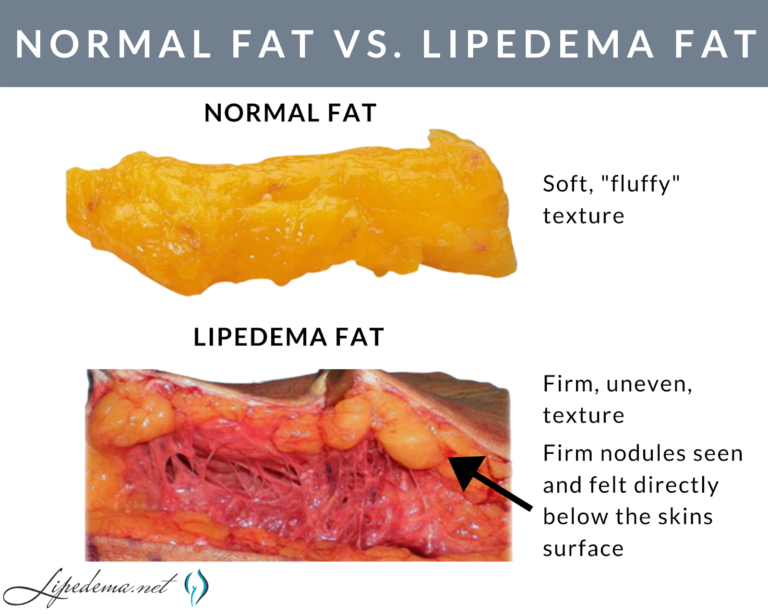
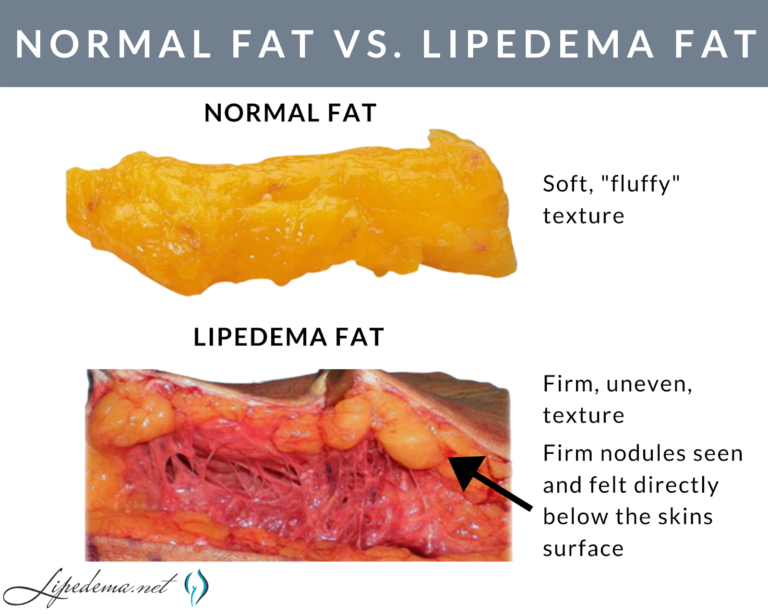
Lipedema is categorized as lipomatosis, also known as a subcutaneous fat disease that is characterized by abnormal fibrosis of the subcutaneous fat tissue. Fibrosis (also known as fibrotic scarring), is a pathological wound healing in which connective tissue replaces normal tissue, eventually leading to the formation of permanent scar tissue. The fibrosis of Lipedema fat tissue gives it a hard, nodular feeling when touched.
How to Determine If You Have Lipedema Nodules
Lipedema nodules are felt and not usually seen. In lipedema, the skin surface is soft, but just below the surface, the nodules can be felt as harder areas. Early-stage Lipedema (Stage 1) has small nodules the size of small seeds or peas, which often appear pearl-size. Middle-stage Lipedema (Stage 2) has larger nodules that feel the size of walnuts or gumballs. Later stage Lipedema (Stage 3) is characterized by the presence of lobules. The nodules in Stage may be the same size as the nodules in Stage 2, or they may be larger nodules up to the size of a plum.
The Lipedema nodules felt on the skin are important criteria for diagnosing Lipedema. Nodular or bumpy subcutaneous fat occurs with other conditions or diseases such as cellulite or obesity and other fat disorders, however, subcutaneous nodules must be present to diagnose lipedema. These nodules represent excess and slightly disorganized fibrosis of the subcutaneous tissue. Inflammation of the adipose tissue in lipedema is likely the cause of this fibrosis.
In these cases, fibrosis tissue in Lipedema patients swirls around the adipose tissue, but it usually won’t completely encapsulate it. If the adipose tissue is completely encapsulated by fibrous tissue, eventually it leads to a lipoma. Women with lipedema have an increased number of lipomas, but most of the bumps felt on the skin are nodules, rather than lipomas.
There are other lipomatosis diseases that cause similar side effects as Lipedema to be aware of through the diagnosis process. Dercum’s disease, for example, is characterized by multiple painful subcutaneous lipomas. Madelung’s Disease also has subcutaneous nodules (but not many lipomas), however, these cases occur more in the upper half of the body. Overall, subcutaneous nodules are present in all patients with lipedema but they also occur in other subcutaneous fat diseases or lipomatosis.
Removing Lipomatosis Nodules
In the earlier stages of Lipedema (Stage 1 and most patients in Stage 2), the subcutaneous nodules are removed with lipedema reduction surgery, which involves modification of cosmetic liposuction using tools and techniques which minimize harm to the lymphatics. In lipedema patients with larger or more adherent nodules, the nodules have to be manually extracted.
In these cases, a small incision is made over the nodules that resist removal with a suction cannula and are gently milked out of the skin. Obviously, surgeons don’t want to cause any more trauma than is absolutely necessary, however, there are instances where this method is the only way to get larger, more adherent nodules removed. Dr. Wright has several videos of the extraction process you can view here.
Think you have Lipedema nodules?
Below are the different tests you may experience during this time, and it’s important to keep them in mind as you select your doctor. Moving forward, thoroughness will be your best friend; we highly recommend “interviewing” different Lipedema experts to find someone you trust, someone who can provide at least some of these diagnostic tests, and someone who is well versed in treatment options.
Note: There is no single test to diagnose Lipedema. Tests, however, are important to rule out a related disorder.
Stemmer’s Sign Test
The Stemmer’s Sign is the inability to pinch the skin between the toes or fingers. As mentioned in our last section, Lipedema in advanced stages can be complicated by secondary Lymphedema and may have a stemmer’s sign. This test can help Lipedema experts determine if this is the case for you.
Venous Doppler Ultrasound
A Venous Doppler Ultrasound is a very useful test for the diagnosis of Lipedema and to locate potential nodules. Lipedema has many similarities to venous insufficiency, so this can also help rule out or confirm venous insufficiency. The Venous Doppler Ultrasound can readily detect venous insufficiency if done properly and by having the patient stand while completing it. A standing venous Doppler ultrasound is a painless, non-invasive, and inexpensive test that provides a lot of useful information about venous circulation. The Doppler ultrasound not only helps determine the presence of underlying venous problems, but it also gives critical information for managing Lipedema. If venous insufficiency is present, it is important that treatment is given as the resulting increased venous pressures can greatly aggravate Lipedema.
Lymphoscintigraphy
This is generally only used in complicated cases, where clinical diagnosis is not clear. This is a nuclear scan that assesses the lymph system. It may come back as normal in patients with Lipedema and may show the characteristic “corkscrew” changes with Lymphedema. In most cases of Lymphedema, lymphoscintigraphy shows delayed uptake. So lymphoscintigraphy can be very helpful to determine if and how significant a role lymphedema is playing in an individual’s symptoms, especially when there are widespread issues of swelling in the body.
We’re here to help!
Now that you’ve reviewed the signs and symptoms of Lipedema, determined that you identify with at least some of them, and you’ve familiarized yourself with other commonly related diagnoses, it’s time for the final step – finding a Lipedema specialist who can perform one of the diagnostic methods above. Each Lipedema doctor will have their own preferred method of diagnosing their patients and typically will include a physical exam, patient questionnaires, and then additional testing and ultrasounds to further support the physical exam.
A treatment plan should be discussed and developed between you and your Lipedema doctor, but you can read more about the non-surgical and surgical options that we recommend to our patients. While these will always depend on specific cases and patient needs, it can give you an idea of what options may be available to you. Our hope for all women with Lipedema, whether they are our patients or not, is that we can provide valuable tools and knowledge so that more women can make it to this point and take the next step in living a more mobile, healthy, and enjoyable life.
1. Pain with lipoedema Attempt to approximate W. Schmeller, I. Meier-Vollrath Capio Hanse-Klinik, Department of Liposuction and Operational-Aesthetic Dermatology, Lübeck, Germany LymphForsch 12 (1) 2008; 8-12
Prevention of Progression of Lipedema With Liposuction Using Tumescent Local Anesthesia; Results of an International Consensus Conference Matthias Sandhofer, MD. DermSurg-2019. link https://pubmed.ncbi.nlm.nih.










