

In today’s society, body image and weight management are often hot topics of discussion. Many individuals strive to achieve their desired physique through diet and exercise. However, for some, the struggle to lose weight in certain areas, particularly the legs, can be frustrating and confusing. This leads us to a common question: Is it lipedema or obesity? In this comprehensive guide, we will explore the key differences between lipedema and weight gain, helping you understand your body better and make informed decisions about your health and well-being.
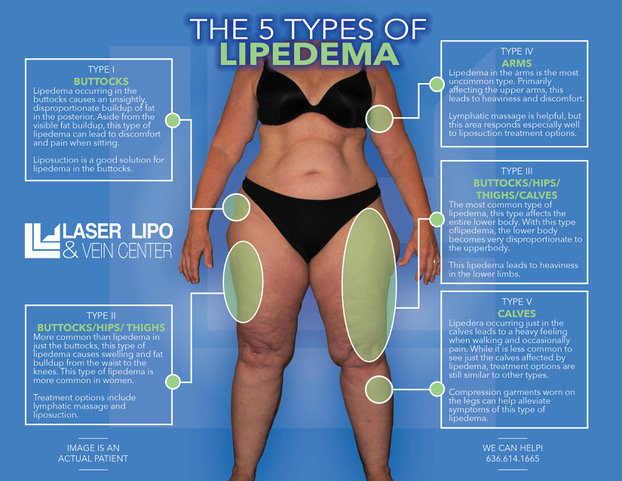
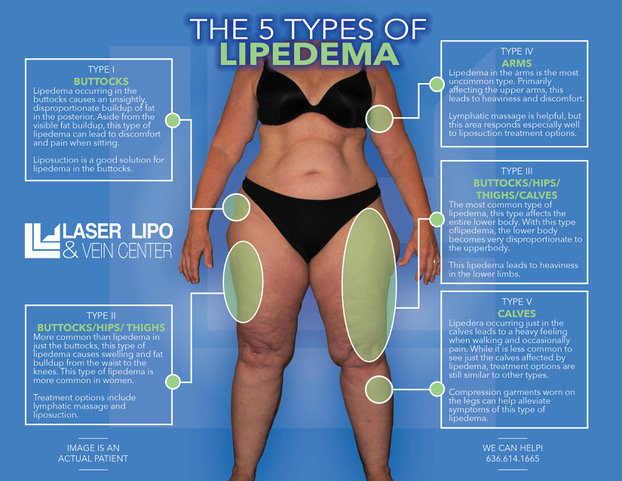
Lipedema is a chronic and progressive medical condition characterized by the abnormal accumulation of fat cells, primarily in the lower body. It predominantly affects women, with an estimated prevalence of 7-11% in Western countries. Lipedema causes a disproportionate increase in fat deposits in the legs, hips, and buttocks while sparing the hands and feet. Individuals with lipedema often have a smaller waist and upper body, creating a distinct pear-shaped appearance.
One of the primary distinctions between lipedema and weight gain is that lipedema fat is resistant to traditional weight loss methods such as diet and exercise. Despite leading a healthy lifestyle, individuals with lipedema find it challenging to reduce fat in the affected areas. Lipedema fat can also exhibit unique characteristics, such as a gelatinous texture and the presence of small nodules beneath the skin.
Lipedema is thought to have a genetic component, with hormonal changes during puberty, pregnancy, and menopause potentially triggering its onset or exacerbation. It is crucial to understand that lipedema is not caused by obesity. While many individuals with lipedema may also be overweight or obese, the condition itself is independent of weight status.


It is important to distinguish between lipedema and weight gain to ensure accurate diagnosis and appropriate treatment. While both conditions involve the accumulation of excess fat, they have distinct characteristics and underlying causes.
Lipedema presents with specific symptoms that differentiate it from general weight gain. Individuals with lipedema often experience:
In contrast, weight gain typically occurs more evenly throughout the body and is not associated with pain or other physical symptoms commonly seen in lipedema.
One of the key distinctions between lipedema and weight gain is the response to lifestyle changes. Individuals with lipedema often find that diet and exercise alone do not significantly impact the fat accumulation in the affected areas. Despite their best efforts, weight loss may be minimal or not occur at all in these specific regions. On the other hand, individuals experiencing general weight gain will typically see changes in their body composition through proper nutrition and physical activity.
Lipedema fat distribution differs from general weight gain. Lipedema fat primarily affects the lower body, including the legs, hips, and buttocks, while sparing the hands and feet. This leads to a distinct shape and disproportion between the upper and lower body. In contrast, weight gain is typically more evenly distributed throughout the body, without the characteristic pear-shaped appearance.
Lipedema not only affects physical health but can also have a significant psychological and emotional impact. Many individuals with lipedema experience depression, low self-esteem, and social isolation due to the perceived body image differences and the challenges associated with finding appropriately fitting clothing. Weight gain, on the other hand, may have similar psychological effects but is not specifically linked to the unique challenges faced by individuals with lipedema.


Accurate diagnosis is essential to establish appropriate treatment strategies for individuals with lipedema. If you suspect that you may have lipedema, it is crucial to consult with a healthcare professional experienced in the diagnosis and management of this condition. They will evaluate your symptoms, medical history, and perform a physical examination to assess fat distribution and other associated features.
Currently, there is no cure for lipedema, but various treatment options can help manage symptoms and improve quality of life. Treatment for lipedema may include:
It is important to note that liposuction is not a cure for lipedema but can offer significant improvements in symptoms and overall quality of life for select patients.


Understanding the difference between lipedema and weight gain is crucial for accurate diagnosis and appropriate treatment. Lipedema is a chronic condition characterized by the abnormal accumulation of fat in the lower body, while weight gain is a general increase in body weight. Lipedema fat is resistant to traditional weight loss methods, and individuals with lipedema often experience specific symptoms, such as pain, tenderness, and easy bruising.
If you suspect you may have lipedema, consulting with a healthcare professional or an experienced lipedema specialist is essential to develop an individualized treatment plan that addresses specific needs and goals. Dr. Wright and his team of experts are here for you whenever you’re ready to start your treatment journey!
Remember, your health and well-being are important, regardless of your body shape or size. By seeking appropriate care and support, you can live a fulfilling life and embrace your unique beauty.


Lipedema and cellulitis are two conditions that often coexist, causing discomfort and distress to those affected. Understanding the relationship between these two conditions and implementing prevention strategies is crucial for optimal management. Lipedema is a chronic disorder characterized by an abnormal accumulation of fat in the legs and sometimes the arms, causing pain, swelling, and tenderness.
On the other hand, cellulitis is a bacterial skin infection that can occur as a complication of lipedema due to impaired lymphatic drainage and weakened immune response. It presents with redness, swelling, and warmth in the affected area. By addressing both lipedema and cellulitis simultaneously, individuals can experience relief from symptoms and prevent recurrent infections.
Prevention strategies for lipedema-related cellulitis may include maintaining good hygiene practices, promptly treating skin abrasions or wounds, wearing compression garments, and seeking early medical intervention to address lipedema symptoms. In this article, we will explore the relationship between lipedema and cellulitis, exploring effective prevention strategies and highlighting treatment options available in St. Louis. By understanding and managing these conditions, individuals can enhance their quality of life and overall well-being.
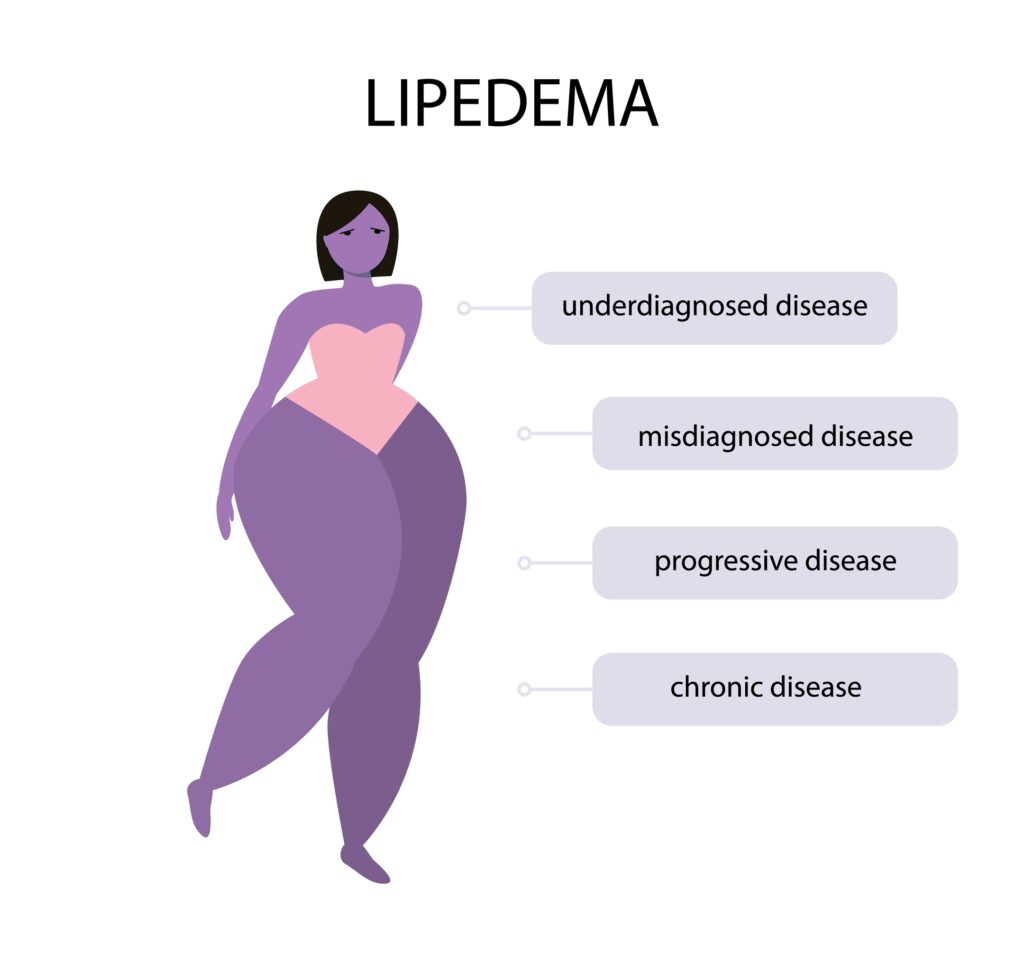
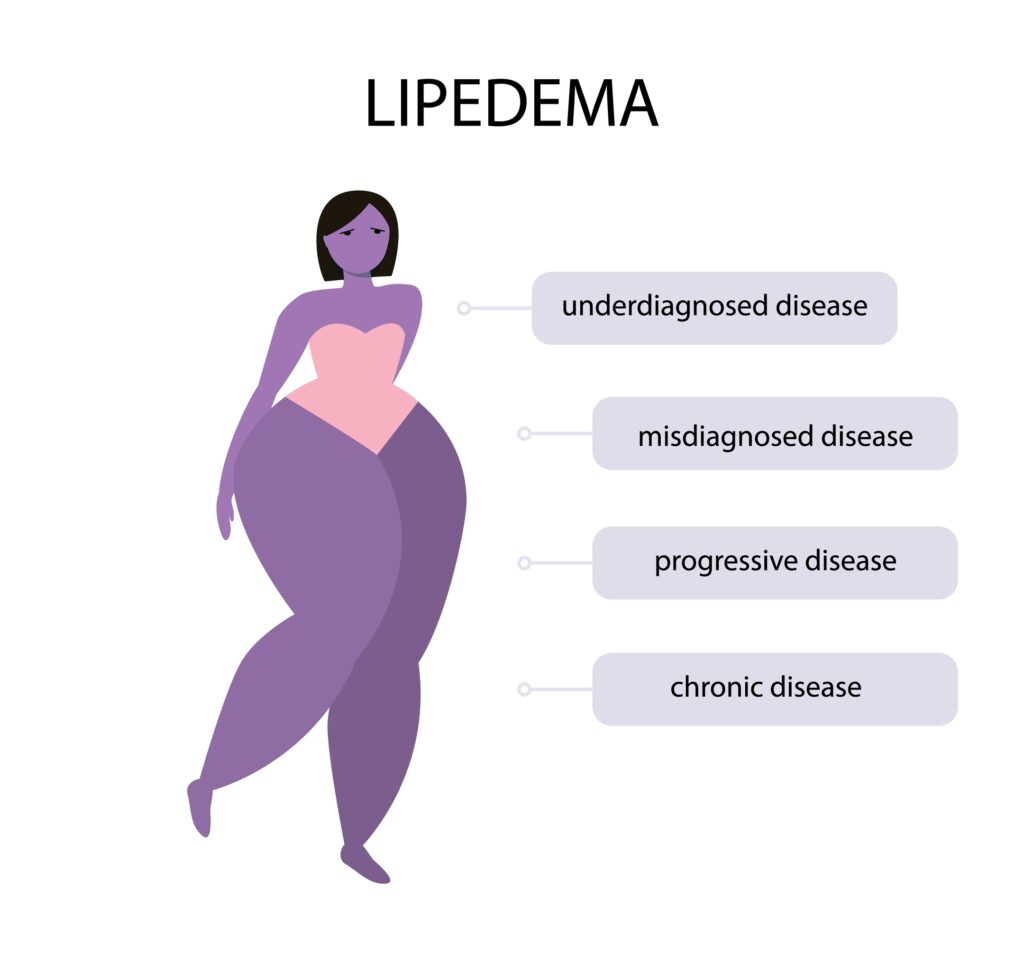
Lipedema is a fat tissue disease, mainly affecting women, that causes an enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Medical professionals often misdiagnose and dismiss lipedema as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
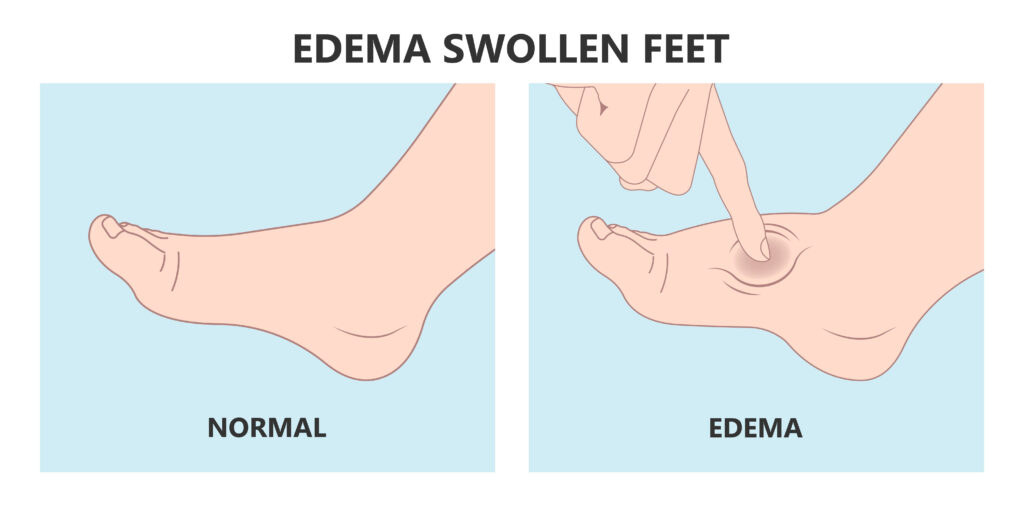
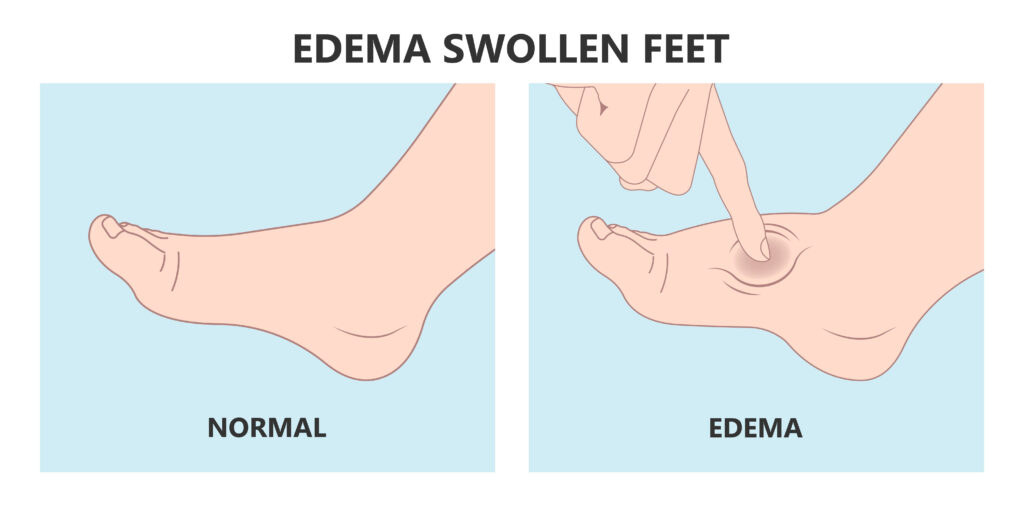
Women suffering from Lipedema often report the disease a sociated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.
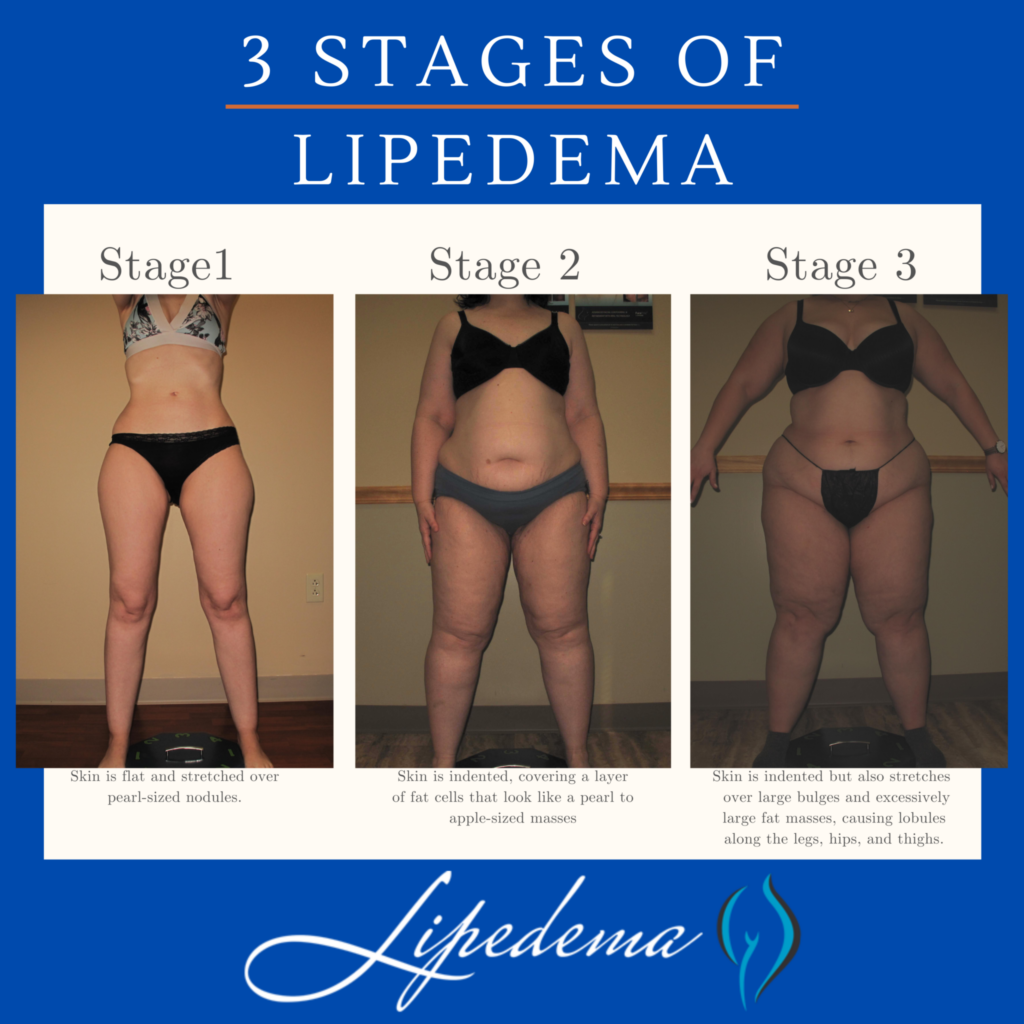
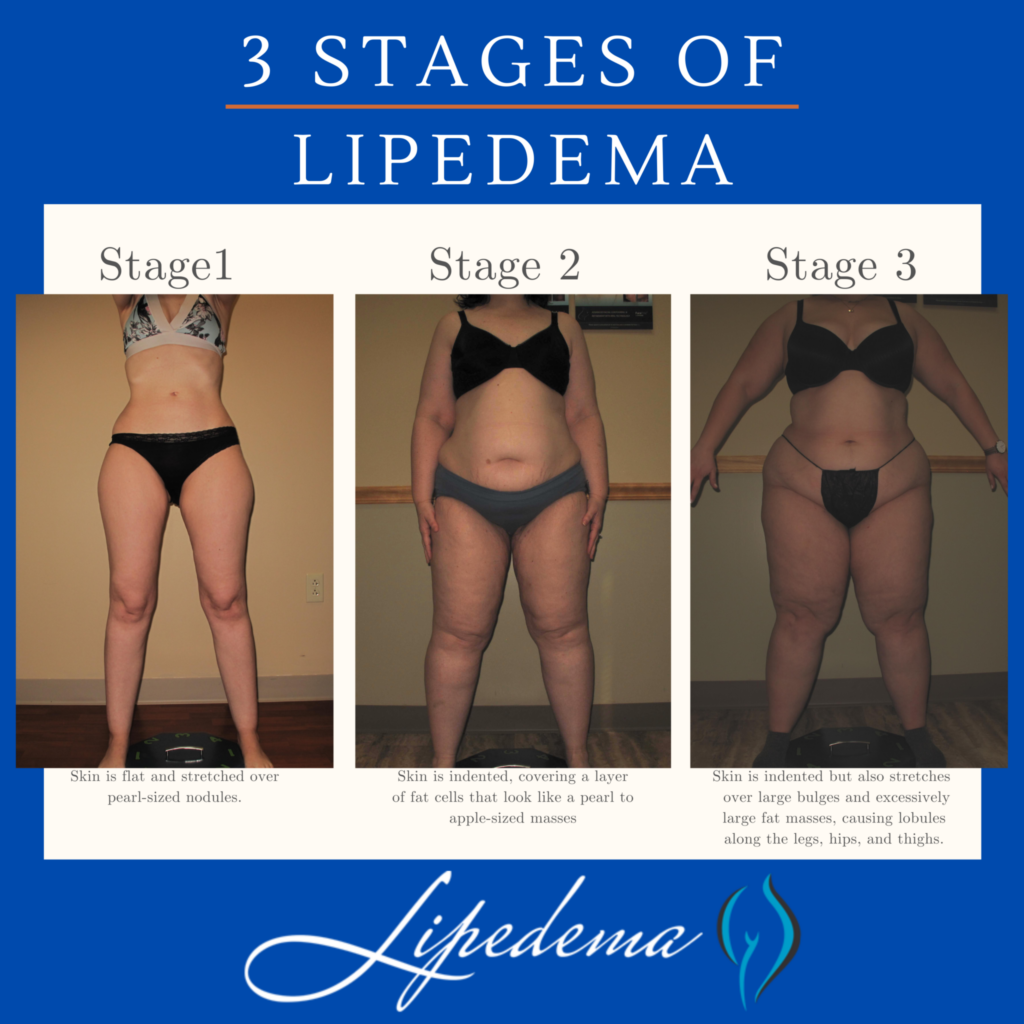
Early detection of lipedema is crucial for timely intervention and management. Several signs and symptoms can indicate the presence of lipedema. Initially, these symptoms may be subtle, but they become more evident as the condition progresses. Common indicators of lipedema include symmetrical swelling in the legs, unexplained bruising, heaviness and tenderness in the affected limbs, and a lower body size disproportionate to the upper body. In advanced stages, the skin may develop pearl-sized lumps, which can grow larger and resemble walnuts or plums.
Diagnosing lipedema can be challenging due to a lack of awareness among healthcare professionals. Many patients are misdiagnosed with obesity, leading to delayed treatment and unnecessary fat-shaming. To ensure accurate diagnosis and appropriate treatment, it is crucial to seek the expertise of a specialist familiar with lipedema. Early diagnosis allows for timely intervention and improves the chances of successful treatment outcomes.
Effective treatment strategies are available for individuals with lipedema. Lymphatic support, such as complete decongestive therapy, can help manage the symptoms of lipedema. Additionally, specialized suction lipectomy, a surgical procedure, can remove diseased lipedema fat while preserving lymphatic channels. This surgical intervention not only enhances the patient’s quality of life but also improves their self-confidence by restoring a more proportionate appearance to the lower body.
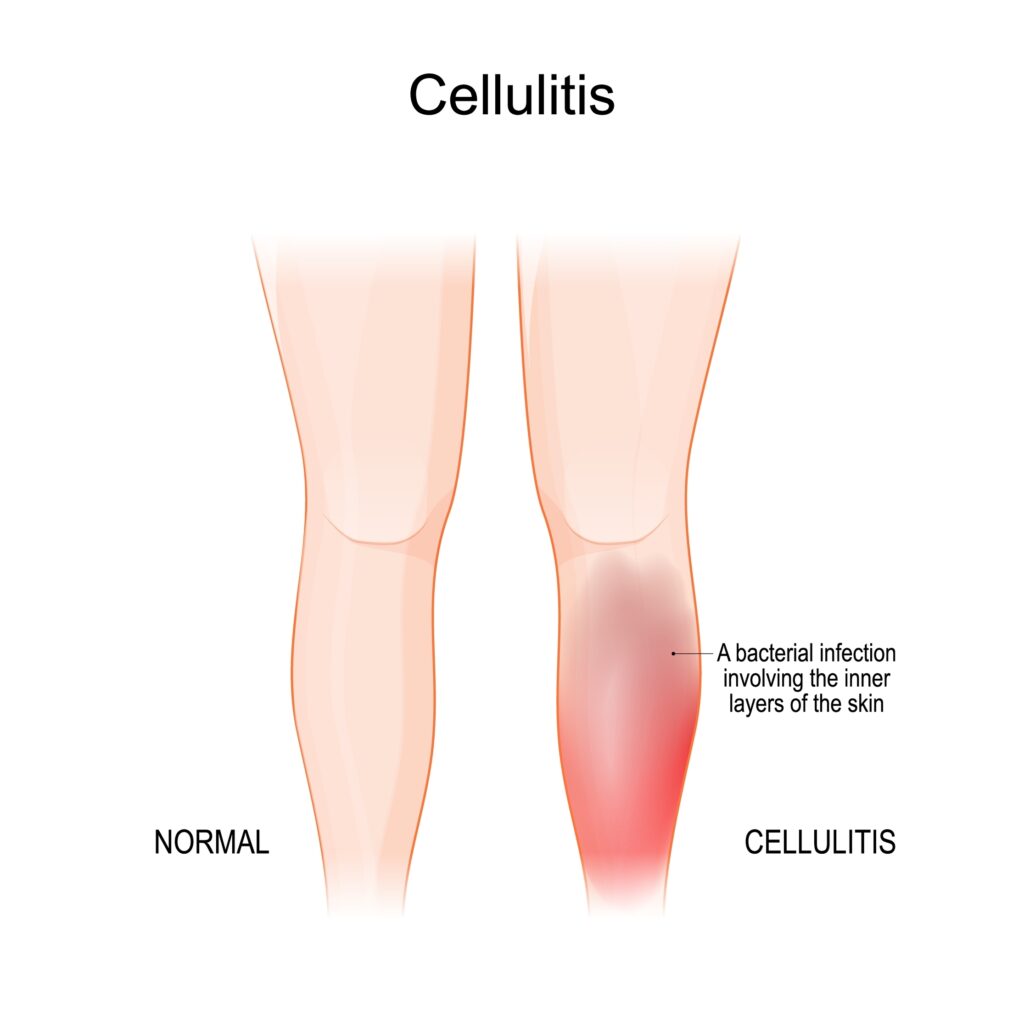
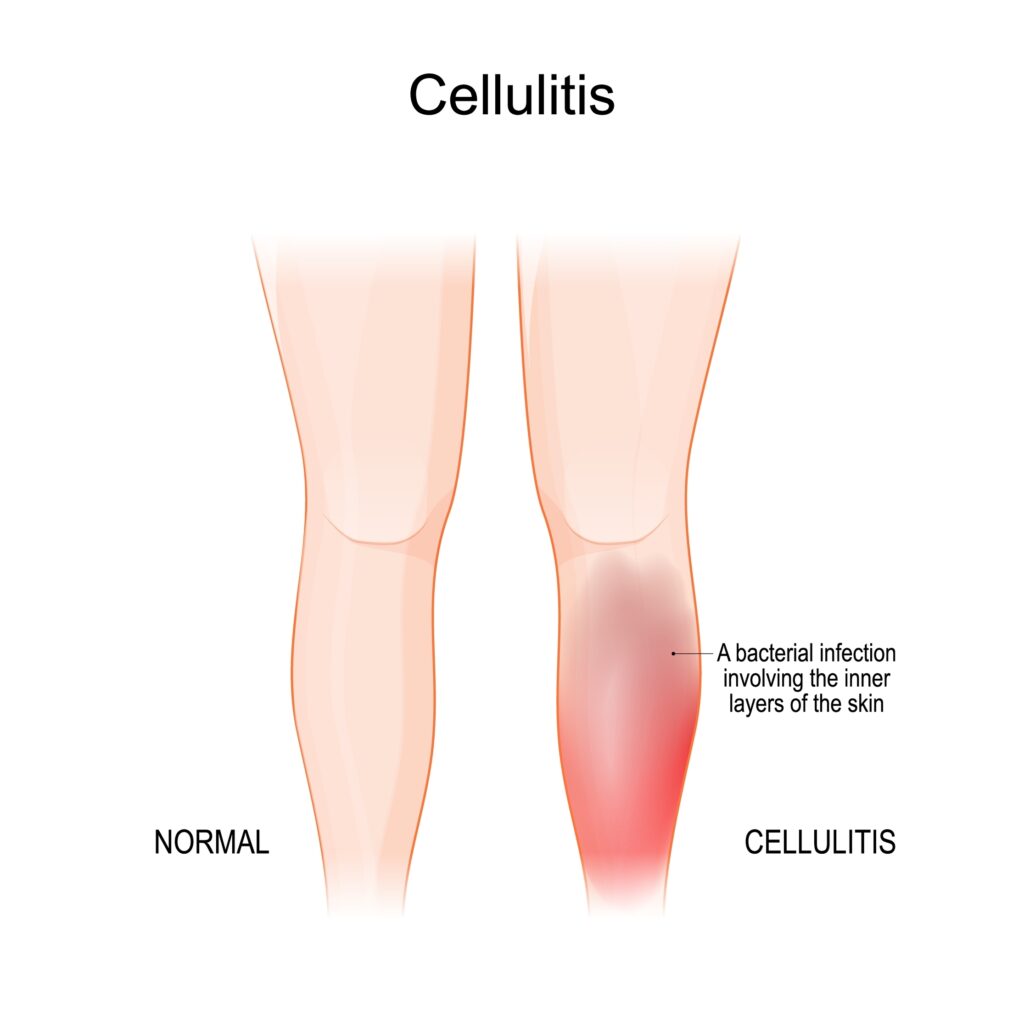
Cellulitis is a skin infection caused by bacteria that infiltrate the deep layers of the skin through breaks such as cuts or scratches. Common symptoms of cellulitis include redness, swelling, pain, tenderness, and the development of blisters. It is essential to note that cellulitis is not a direct symptom of lipedema but can arise due to the underlying condition.
While cellulitis is not a direct symptom of lipedema, individuals with lipedema are more susceptible to developing cellulitis due to factors such as poor circulation, lymphatic dysfunction, and chronic edema. Lipedema can compromise the lymphatic system’s ability to fight infections, increasing the risk of cellulitis. Therefore, it is essential to understand the relationship between lipedema and cellulitis and take preventive measures to mitigate the risk.
Preventing cellulitis in individuals with lipedema involves a multifaceted approach. It is crucial to manage the underlying risk factors that contribute to the development of cellulitis, such as chronic edema, venous disease, dermatomycosis, and obesity. By actively addressing these risk factors, the likelihood of recurrent cellulitis episodes can be significantly reduced. Additionally, non-antibiotic preventive measures, such as daily wound care, the use of protective creams and bandages, regular inspection of the feet, and maintaining good skincare practices, play a crucial role in preventing cellulitis.


Compression therapy has emerged as a beneficial approach for managing lipedema symptoms and reducing the risk of cellulitis. Compression garments, such as stockings or bandages, can help alleviate pain, reduce swelling, and improve lymphatic circulation in individuals with lipedema. These garments apply pressure to the skin and veins, promoting the clearance of lymph fluid and reducing chronic edema. Additionally, pneumatic compression pumps, which mimic manual lymphatic drainage techniques, can be used as an at-home treatment option to improve lymphatic flow and prevent fluid buildup in the affected limbs.
If cellulitis does occur in individuals with lipedema, prompt medical attention and appropriate antibiotic treatment are crucial. Cellulitis can cause severe complications and lead to further damage to the lymphatic drainage routes, exacerbating the swelling and long-term management of lipedema. Therefore, it is essential to seek immediate medical assistance if any symptoms of cellulitis, such as redness, warmth, pain, or fever, arise. Following the prescribed antibiotic treatment and taking necessary precautions, such as removing compression garments until the area heals, can help manage cellulitis effectively.
Raising awareness about lipedema is essential to ensure accurate diagnoses and appropriate treatment for affected individuals. Lipedema support organizations and online communities can provide valuable resources, information, and emotional support to individuals living with lipedema. By connecting with others who share similar experiences, individuals with lipedema can find solace, gain knowledge, and navigate their journey toward better health.
Lipedema is a prevalent adipose tissue disorder that affects a significant number of women worldwide. While cellulitis is not a direct symptom of lipedema, individuals with lipedema are more susceptible to developing cellulitis due to factors such as poor circulation and compromised lymphatic function. Preventive measures, such as managing underlying risk factors, utilizing compression therapy, and practicing good skincare, can significantly reduce the risk of cellulitis in individuals with lipedema. By increasing awareness, promoting early diagnosis, and providing appropriate treatment, we can improve the quality of life for individuals living with lipedema and mitigate the risk of cellulitis in this population. Dr. Wright and his team provide comprehensive treatment plans that consider a patient’s complete medical profile. If you’re looking for solutions to treat symptoms of Lipedema and/or cellulitis, contact us to set up an initial consultation.


Lipedema is a fat disorder that mainly affects women and causes enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity. While the exact prevalence of lipedema is still not well-known, estimates suggest that it may affect a significant portion of the female population. Below, we explore the lipedema prevalence and its symptoms, causes, and available treatment options.
Lipedema is a condition that often goes undiagnosed or misdiagnosed due to its similarity to other conditions, such as obesity and lymphedema. It typically begins during or after puberty, pregnancy, or menopause, suggesting a hormonal influence on its development. Lipedema is characterized by an irregular distribution of fat beneath the skin, causing the affected areas to become larger than other body parts. The condition primarily affects the legs but can also involve the arms in some cases. Unlike obesity, lipedema does not respond to traditional weight loss methods, making it distinct from lifestyle-induced weight gain. Additionally, lipedema is different from lymphedema as it does not start in the lower legs but rather affects the upper legs.
Lipedema is a connective tissue disease that may affect 6-19% of women. (1, 2, 3) If these numbers are valid and applied to the US population, millions of women in the US have lipedema.
Determining the exact prevalence of lipedema has been challenging due to the lack of awareness and recognition of the condition among healthcare professionals. However, recent studies and clinical observations have shed light on its prevalence. According to estimates, lipedema may affect approximately 1 in 9 women globally. This suggests that it is more common than previously believed. However, it is essential to note that the prevalence may vary depending on geographical location and the population studied.
In one study conducted in a referral clinic in Germany, it was found that approximately 11% of women and individuals assigned female at birth had lipedema. This estimate is higher than previous studies and highlights the need for increased awareness and understanding of the condition. However, it is essential to acknowledge that lipedema can be underdiagnosed or misdiagnosed, as it often resembles other conditions.


Lipedema is characterized by specific symptoms that differentiate it from other conditions. The most noticeable symptom is the disproportionate enlargement of the lower body, particularly the legs, hips, and buttocks. This irregular fat distribution can give the appearance of two different bodies combined, with a smaller upper body and a significantly larger lower body. The affected areas may exhibit a lumpy or nodular texture, and the skin may bruise easily. Individuals with lipedema may also experience pain, tenderness, and a heavy feeling in their legs. Other symptoms can include swelling, fatigue, and the development of spider veins or varicose veins in the legs.
It is important to note that lipedema can have a significant impact on an individual’s physical and emotional well-being. The appearance of the legs and the challenges in finding appropriately fitting clothes can lead to self-esteem issues, social isolation, and psychological distress. Therefore, early recognition and appropriate management of lipedema are crucial for improving the quality of life for affected individuals.
The exact cause of lipedema is still unknown, but several factors may contribute to its development. Hormonal influences are believed to play a role, as lipedema often starts or worsens during hormonal changes such as puberty, pregnancy, and menopause. Hormonal contraceptives, such as birth control pills, may also be a contributing factor. Additionally, there is evidence to suggest a genetic component to lipedema, as it tends to run in families.
While obesity itself does not cause lipedema, there is a correlation between the two conditions. It is estimated that more than 50% of individuals with lipedema have a body mass index (BMI) higher than 35. However, it is important to note that lipedema cannot be attributed solely to excess weight, as it is a distinct medical condition with unique characteristics.
Certain risk factors may increase the likelihood of developing lipedema. Being assigned female at birth, having a family history of lipedema, and having a BMI higher than 35 are factors associated with a higher risk of developing the condition.
Diagnosing lipedema can be challenging due to its resemblance to other conditions and the lack of awareness among healthcare professionals. A thorough medical history, physical examination, and evaluation of symptoms are essential for accurate diagnosis. Painful fat deposits and the presence of a significant difference in size between unaffected feet and affected legs can be indicative of lipedema.
There is no specific diagnostic test for lipedema. Still, imaging studies, such as ultrasound, DEXA scan, magnetic resonance imaging (MRI), computed tomography (CT), or nuclear medicine imaging, may be utilized to rule out other conditions or identify any associated complications. These tests can help in differentiating lipedema from conditions such as lymphedema and assessing the extent of fat deposition.
While there is no cure for lipedema, various treatment options are available to manage the symptoms and improve the quality of life for individuals with the condition. The treatment approach may vary depending on the severity of symptoms and individual needs.
Compression therapy, involving the use of compression garments or bandages, is commonly recommended to reduce swelling and provide support to the affected areas. Physical and occupational therapy, including manual lymphatic drainage therapy, can help improve mobility, reduce fluid buildup, and enhance overall well-being. Dietary changes, such as adopting an anti-inflammatory diet, may help manage symptoms and reduce the progression of lipedema. Strength and conditioning exercises, particularly low-impact activities like water exercise, can improve circulation, increase mobility, and promote overall fitness. Counseling or therapy may be beneficial for individuals with lipedema to address the psychological impact of the condition, including depression, low self-esteem, and body image concerns. Additionally, liposuction performed by specialized surgeons can be considered in select cases to remove the diseased lipedema fat and improve mobility and quality of life.


Ultimately, effective treatment will require surgical intervention to alleviate the appearance and pain of symptoms. Liposuction performed on the affected limbs is generally the most effective treatment. Removing diseased fat deposits helps reduce swelling of the limbs and alleviates the pain that holds patients back from everyday activities. This surgical treatment can provide various benefits and relieve the symptoms you are experiencing from lipedema. Dealing with lipedema can be difficult, especially if you are just now starting to take control of it. Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the growth of more fat cells, which can overwhelm the lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and worsening an already stressed system. Studies have shown that lymphatic function can improve after this type of liposuction in women with Lipedema using blunt cannulas, generous tumescent anesthesia, and special surgical techniques. Lipedema reduction surgery aims to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a “debulking” surgery, not a cosmetic surgery.


If you suspect that you may have lipedema, it is important to consult with a healthcare professional who specializes in the condition. A vascular surgeon, plastic surgeon, or dermatologist with expertise in lipedema can provide an accurate diagnosis and recommend appropriate treatment options based on your needs. Early diagnosis and management of lipedema are crucial in preventing the condition’s progression and improving overall health outcomes. By seeking professional help, individuals with lipedema can receive the care and support they need to manage their symptoms and maintain their quality of life. Lipedema is a prevalent condition that primarily affects women, causing abnormal fat buildup in the lower body. While the exact prevalence of lipedema is still uncertain, estimates suggest that a significant portion of the female population may be affected. Recognizing the symptoms, understanding the causes and risk factors, and seeking appropriate treatment are essential for managing lipedema and improving overall well-being. By increasing awareness and understanding of the condition, we can ensure that individuals with lipedema receive the care and support they deserve.
Sources
[i] Foldi E, Foldi M. Das lipodem. In: M Foldi, E Foldi, and S Kubik, eds. Lehrbuch der
Lymphologie für Mediziner, Masseure und Physiotherapeuten. Munich: Elsevier, Urban &
Fischer;2005:443-453.
https://www.amazon.com/F%C3%B6ldis-Textbook-Lymphology-Physicians-Lymphedema/dp/0723436460
[ii] Crescenzi R. Donahue PMC, Weakley S, Garza M, Donahue MJ, Herbst KL.
Lipedema and Dercum’s disease: a new application of bioimpedance. Lymphat Res
Biol 2019;17(6):671-679.
https://pubmed.ncbi.nlm.nih.gov/31408408/
[iii] Gould DJ, El-Sabawi B, Goel P, Badash I, Colletti P, Patel KM. Uncovering lymphatic
transport abnormalities in patients with primary lipedema. J Reconst
Microsurg 2020;36(2):136-141.
https://pubmed.ncbi.nlm.nih.gov/31546262/


Lipedema is a condition characterized by the abnormal accumulation of fat cells, primarily in the lower body, causing pain, swelling, and decreased mobility. While liposuction is considered the most effective treatment for lipedema, it’s imperative that individuals with lipedema first master the non-surgical treatment options to control their systems. Two popular alternatives that have gained attention are whole-body vibration and dry brush massage. In this comprehensive guide, we will delve into the benefits of these techniques, their impact on lymphatic circulation, and their potential as complementary treatments for lipedema.
Before diving into the specifics of whole body vibration and dry brush massage, it is crucial to grasp the fundamental aspects of lipedema and the lymphatic system. Lipedema is a chronic condition characterized by the disproportionate accumulation of fat cells, typically in the lower limbs, buttocks, and sometimes the arms. This adipose tissue buildup is often accompanied by pain, tenderness, and easy bruising. The lymphatic system plays a vital role in maintaining fluid balance, immune function, and waste removal. It consists of lymphatic vessels, lymph nodes, and other lymphoid organs.
The lymphatic system works in close coordination with the circulatory system to transport lymph, a clear proteinacious fluid rich in white blood cells, throughout the body. Lymphatic vessels run parallel to blood vessels, and lymph nodes act as filtration centers, removing waste products and pathogens before returning the filtered fluid to the bloodstream. When the lymphatic system is compromised, as in the case of lipedema, the transport and drainage of lymph can be impaired, leading to fluid accumulation, tissue swelling and inflammation. Evententually this tissue swelling and inflammation can lead to tissue growth.


Dry brush massage is a technique that involves using a soft-bristled brush to gently stimulate the skin’s surface, promoting lymphatic circulation and exfoliating the skin. Advocates of dry brush massage claim that it can help move venous blood, stimulate the lymphatic system, strengthen the immune system, improve surface circulation, and enhance the skin’s appearance.
To perform dry brush massage, you will need a brush with soft bristles, either with a handle or a strap. It is important to use the brush on dry skin, as wet skin or a wet brush will not yield the same benefits. Begin by using long, gentle, and firm strokes, moving the brush towards the heart and neck. Start at the feet and brush upward towards the knees, groin, abdomen, and chest. Then, proceed to brush the hands and arms up to the armpits. It is important to avoid the face during dry brush massage.
Whole body vibration (WBV) therapy involves standing, sitting, or lying on a vibrating platform, which causes mechanical vibrations to pass through the body. This stimulation is believed to have positive effects on muscle strength, circulation, and lymphatic flow. While there is limited research specifically examining the impact of WBV on lipedema, studies exploring its effects on skin blood flow and lymphatic circulation provide valuable insights.
A study conducted by Dr. Lowman in 2007 investigated the effects of lower-frequency vibration on skin blood flow. The study found that vibration significantly increased blood flow to the skin, highlighting the potential benefits of WBV in improving circulation. Another study conducted by researchers further demonstrated the effectiveness of low-frequency vibrotherapy in treating lipedema. The study compared the outcomes of patients who received manual lymphatic drainage (MLD) treatments alone versus those who received a combination of MLD and vibrotherapy. The findings revealed that the combined treatment led to significant reductions in lipedema size and improved quality of life compared to MLD alone.
While the exact mechanisms through which WBV affects lymphatic flow in lipedema are not fully understood, it is believed that the vibrations stimulate muscle contractions, which, in turn, facilitate lymphatic drainage. By incorporating WBV into a comprehensive lipedema treatment plan, individuals may potentially experience improvements in circulation, reduction in swelling, and enhanced overall well-being.
While whole-body vibration and dry brush massage offer potential benefits for individuals with lipedema, it is important to note that these techniques do not address the underlying cause of the condition, which is the abnormal accumulation of fat cells. Liposuction remains the most effective treatment for lipedema, as it permanently removes the problematic fat cells, providing long-lasting relief from pain, swelling, and mobility issues.
However, whole-body vibration and dry brush massage can be valuable complementary treatments to support overall lipedema management. By incorporating these techniques into a comprehensive approach that includes proper nutrition, compression therapy, exercise, and other recommended treatments, individuals may experience enhanced lymphatic circulation, reduced inflammation, and improved overall well-being.
Whole body vibration and dry brush massage show promise as complementary treatments for individuals with lipedema. While they may not replace liposuction, incorporating these techniques into a comprehensive management plan can potentially enhance lymphatic circulation, reduce swelling, and improve overall quality of life. As with any treatment, it is important to consult with a healthcare professional before starting any new regimen and to seek guidance tailored to individual needs. By taking a holistic approach to lipedema management, individuals can find relief and improve their well-being.
It is crucial to remember that lipedema affects individuals differently, and the effectiveness of treatment options may vary depending on the severity and stage of the condition. Consulting with a healthcare professional or an experienced lipedema specialist is essential to develop an individualized treatment plan that addresses specific needs and goals. Dr. Wright and his team of experts are here for you whenever you’re ready to start your treatment journey!


Lipedema is a condition that affects the distribution of fat in the body, primarily in the lower extremities. Lipedema is a progressive disorder and a significant portion of women with Lipedema progress to secondary Lymphedema. Understanding the relationship between lymphatics and Lipedema is crucial in understanding how lipedema develops and progresses.
It’s characterized as a “progressive disorder,” meaning the tissues enlarge and that, over time, there is a progressive deterioration of lymphatics. When looking at extracellular water content, which is a marker of lymphatic function, the higher the stage of lipedema, the greater the proportion of women with lipedema who also had increased amounts of extracellular water consistent with lymphatic impairment. To put it simply, research is finding that lipedema and lymphatic impairment are related.
The lymphatic system is responsible for maintaining the balance of fluids in the body and helps remove waste products and toxins through a network of vessels and lymph nodes. When the lymphatics are not functioning properly, fluid can build up, leading to swelling and inflammation. In the case of lipedema, there is often impaired lymphatic drainage. Excess fat cells can pressure the lymphatic vessels, causing them to become compressed and less effective at removing fluid.
Lymphatic impairment changes the whole biology of the affected tissues. In the legs and arms affected by lymphatic impairment, the biology of the fat cells and other connective tissues is changed. The cells and tissues are always creating proteins and storing and releasing fats as part of a normal, healthy bodily function. As part of this system, lymphatics are responsible for removing fatty acids, cellular debris, and large protein as they work to clean up, remodel, and maintain the structure and function of the tissues.
When we have lymphatic impairment in our tissues, the biology of these cells completely changes. There is an increased deposit of fibrous tissues, and the fat cells increase in number and size. These cells are no longer doing their job properly, and we don’t have equilibrium; the balance shifts towards tissue growth and fibrosis, leading to swelling and limb enlargement that is typical of lipedema and oftentimes, secondary lymphedema.
As the tissue enlarges in women with lipedema, we start to see more telltale signs of the disease, such as lobules and cuffs at the ankles and wrists. As these lobules and cuffs enlarge, the skin droops and hangs off the body. This, in turn, causes localized swelling and further disrupts the lymphatic flow, leading to a vicious cycle. The tissue enlargement caused by impaired lymphatics further disrupts lymphatic function. Read more about Lipedema Lobules and Nodules here.
Let’s break down in greater detail the lymphatic system and its role in maintaining healthy tissue. The lymphatic system is a network of vessels and organs that help remove waste, toxins, and excess fluid from our tissues. It plays a vital role in maintaining a healthy immune system and fluid balance. The lymphatics and veins are closely interconnected. Lymphatic vessels are responsible for carrying lymphatic fluid, which contains immune cells and waste products, while veins are responsible for carrying blood back to the heart. Both systems work together to ensure proper circulation throughout the body. For those struggling with vein health and lipedema, we’ve outlined the causes and treatments.
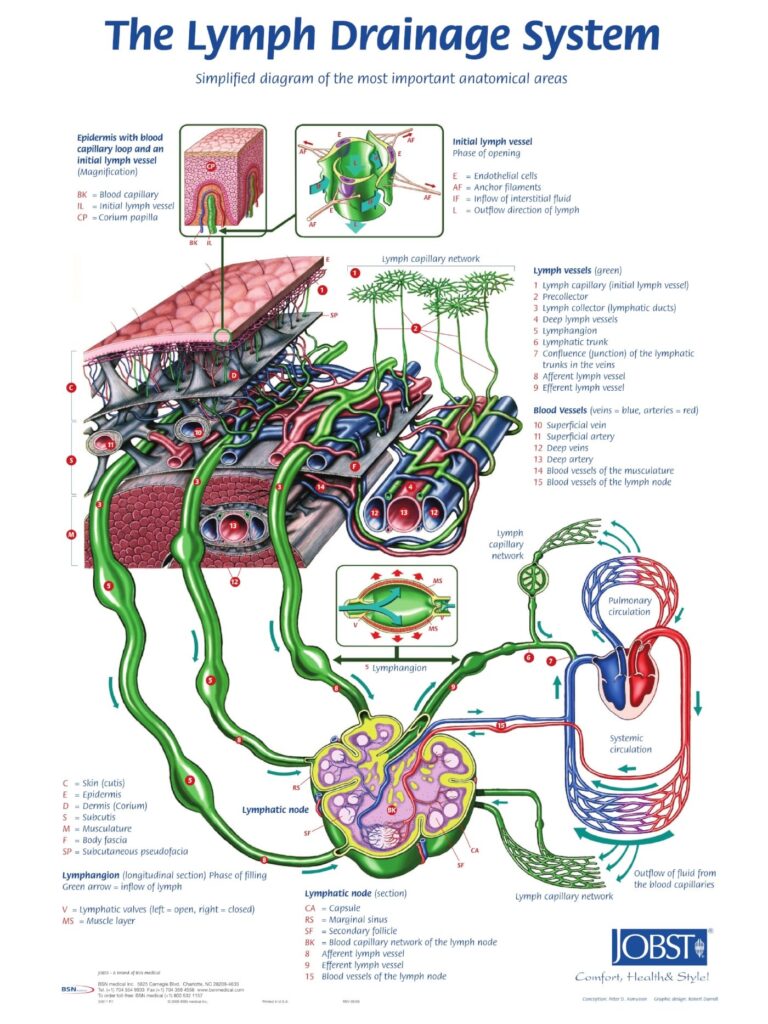
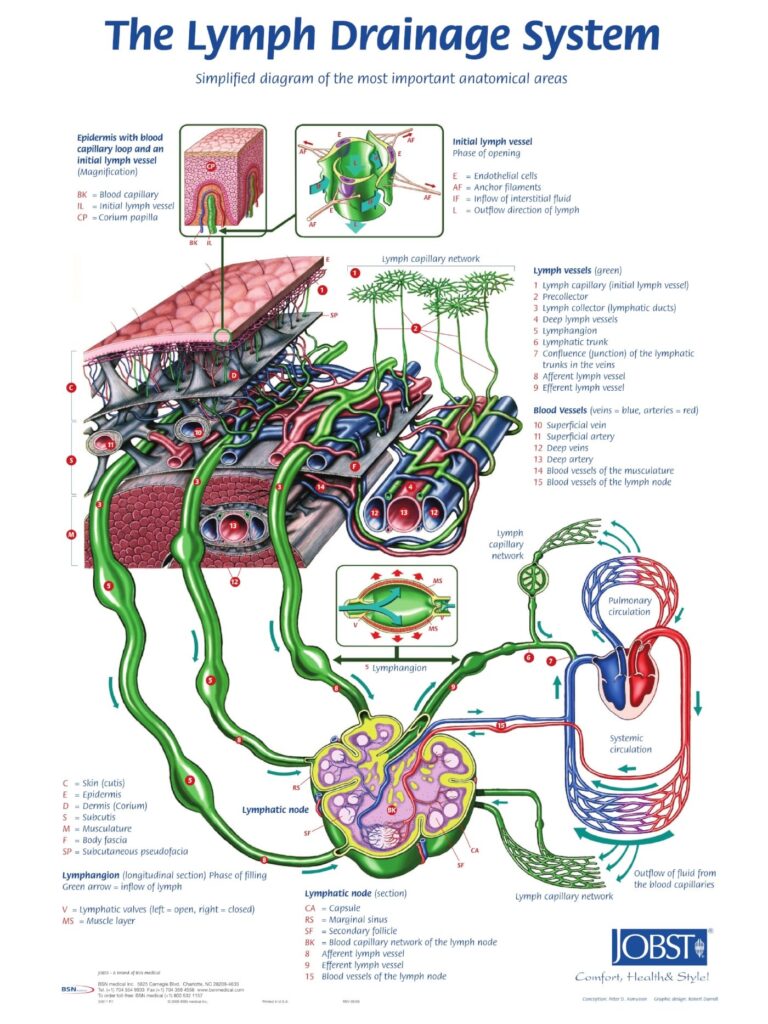
Like lipedema, lymphatic circulation has been neglected and largely ignored until recently. For example, the arterial-venous circulation system is nearly common knowledge. Most people learn about it in school, and we have a clear understanding of how it works: The heart pumps the blood through the arteries, which take the oxygenated blood to the tissues, and then the venous system returns the deoxygenated blood to the heart. This is a closed system. On the other hand, lymphatics are an open system that is seldom talked about in school. In this system, we aren’t focused on blood flow but on lymph fluid which is a clear and sometimes yellow-tinted proteinaceous fluid. Lymph is created in the tissues from the fluid that leaks out at the capillary level and contains large proteins, cells, and cellular debris.
The basic unit near the start of the lymphatic system is the lymphangion, which is a smooth muscle-lined vessel that propels the fluid toward our lymph nodes. The Lymphatic System is self-propelling. There are valves at the beginning of the lymphatic system that ensures that the fluid that enters will not be able to flow out and leave. Along the way, there are additional valves, much like the venous system, which ensure one-way flow. And also, like the venous system, the fluid is further aided and propelled forward by the contraction of muscles.
The lymphatics start at a lymphatic capillary level, which combines into lymphatic collecting ducts. These collecting ducts further collect together and become lymphatic trunks and enter lymph nodes. In the lymph nodes, the lymph is filtered, and lymphocytes scour and search for foreign cells and proteins that should be removed from the body. After the lymph is filtered through the lymph nodes, it’s sent toward the center of the body. Eventually, it ends up in the thoracic duct, where it returns to the venous circulation, just in front of the heart.
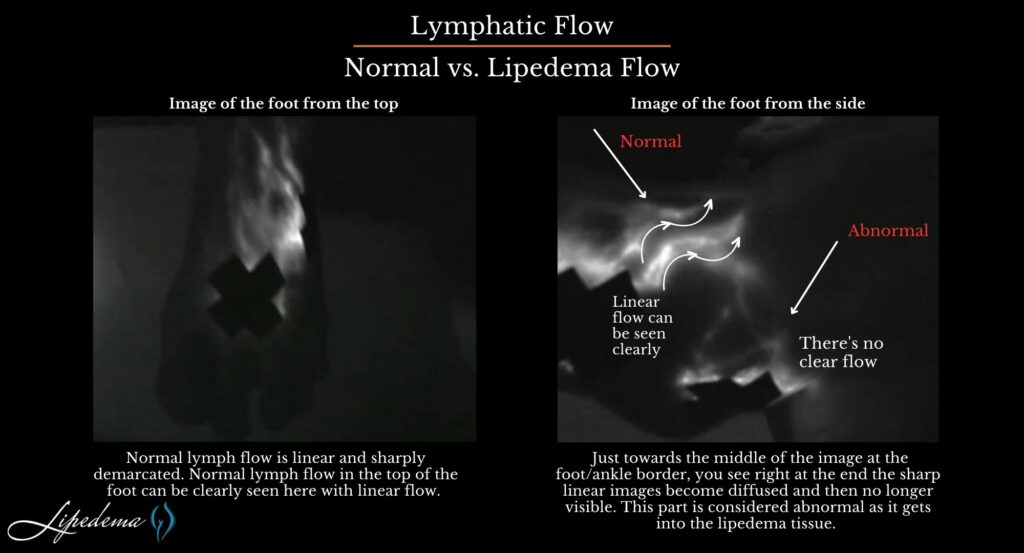
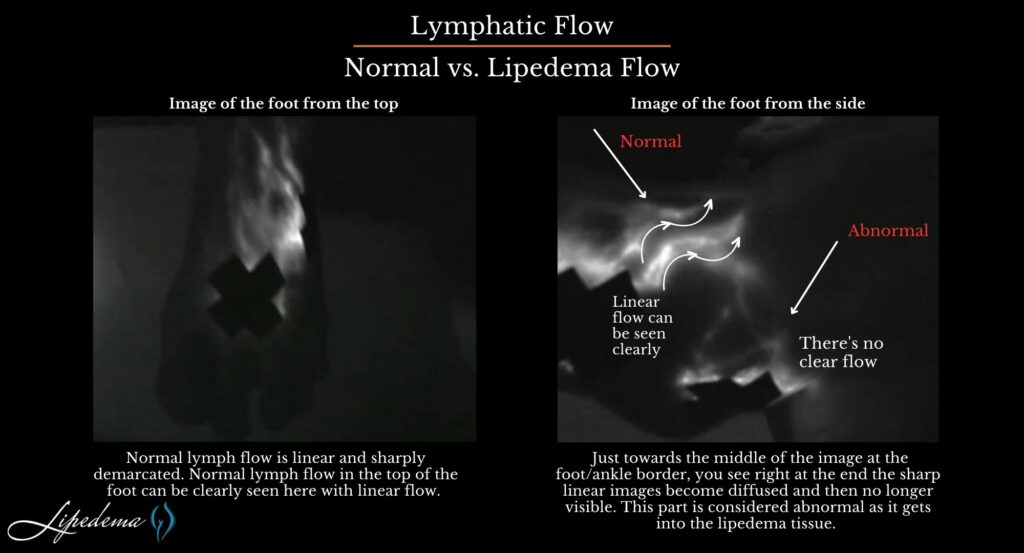
There are well-documented changes in the lymphatics of women with lipedema. Rasmusen and others have reported on dilated lymphatics in lipedema. Many other authors have reported on impairments of lymphatics in lipedema (Gould, Van De Pas). The following is a near-infrared direct lymphography image from research conducted by Dr. Wright. In it, you can see the difference between normal and Lipedema tissue found in the foot and ankle. In this image, there is normal, linear lymphatic flow in the lipedema patient’s foot, which changes to dilated, tortuous lymphatic flow as the lymph flows in the area of the ankle cuff caused by lipedema.
Normal lymphatic vessels seen with Near InfraRed [ NIR ] Imaging are linear and sharply demarcated, and as lymph moves into lipedema tissue, it becomes less demarcated and fuzzy or has more diffuse borders. Just towards the middle of the image at the foot/ankle border, you see right at the end, the sharp linear images become diffused and then no longer visible. This part is considered abnormal as it gets into the lipedema tissue.
The above images show that there are dilated lymphatics in lipedema and that there are reports that liposuction can injure lymphatics in lipedema. Now that we know the relationship between the two, it’s imperative that compression and other lymphatic flow-promoting treatments are included in the comprehensive treatment of lipedema. We’ll explain these practices below, and you can read more about the Lipedema Standard of Care here.
Before any type of surgery can be discussed, it’s important to ensure the non-surgical treatments are followed, and the lymphatic function is optimized. Examples of these practices are below, and you can also read an in-depth study about an approach to the best surgical outcomes by first addressing the inflammation in the tissues with dietary and lymphatic treatment. Read Dr. Amato’s research here.
Compression garments, such as compression stockings or sleeves, can also be useful in providing external support to the lymphatic vessels and promoting fluid movement. In addition to these therapies, maintaining a healthy lifestyle is key. Regular exercise, a balanced diet, and weight management can help reduce the burden on the lymphatics and improve overall lymphatic function. In conclusion, lymphatics and lipedema are closely intertwined. The impaired lymphatic drainage seen in lipedema can contribute to chronic swelling and inflammation, further complicating the condition. Understanding this relationship is vital for effective treatment and management of lipedema, with therapies aimed at improving lymphatic function playing a significant role. Read more about compression therapy here.


Exercising can help to activate the lymphatic drainage system in a patient’s limbs through the foot and calf muscle pump. Workouts that aren’t too strenuous help to move the excess fluids out of affected limbs, as well as reduce additional fat buildup. Good lymph flow depends on proper joint and muscle activity. This is especially true if the lymphatic system is compromised. Individuals suffering from lipedema can receive a great benefit when engaging in diaphragmatic breathing exercises. These exercises are especially beneficial when they are combined together with other parts of a decongestive regimen.
Because fat disorders and lymphedema can often feed into one another, exercise is a great option to help combat both. With its dual purpose of clearing out excess lymph fluid and burning fat, exercise offers exactly what patients need to deal with these disorders. Learn more about the best types of exercise for lymphatic flow here.


Dr. Wright recommends following a Rare Adipose Disorder (RAD) diet, a modification to a standard Mediterranean diet that helps you maintain a low glycemic index to limit the number of occurrences and levels your blood sugar spikes through the day. To do this, it is recommended that you avoid any refined or processed starches and sugars. These are usually found in pasta, rice, bread, corn, and potatoes. Avoiding processed food – especially processed carbohydrates – will keep your insulin levels low and provide you the best chance of limiting inflammation. Read more about healthy eating and lymphatic flow here.


Manual lymph drainage is just one component of complete decongestive therapy (CDT). In addition to MLD, complete decongestive therapy includes compression, exercise, and skincare. These therapeutic components, when performed together, can ultimately relieve the symptoms of lipedema, which can often be painful.
When you stimulate the lymphatic system, you will feel the effects of several lymphatic drainage benefits:
Increase the capacity of the lymphatic system, which will then let it process more fluid than normal.:
Other lymphatic drainage massage benefits include reduction of pain and swelling and an increase of venous return and circulation. Learn more about this technique here.
In addition to several other procedures and treatments for lipedema, pump therapy, whole-body vibration, and dry brush massage can also increase the circulation of lymph fluids and relieve the sometimes painful symptoms. Learn more about whole-body vibration and dry brush massage below!
Because the lymphatic system lies just below the skin’s surface, dry brushing has been considered an effective treatment for lipedema. The benefits of dry brushing have been shown to provide :
The dry brushing technique is performed with a brush, either with a handle or a strap, that has soft bristles. As the name says, the brush is used dry and without water. You will not get the same results if the skin or brush is wet. With long, gentle, firm strokes, go over your entire body (except the face). The strokes should move the skin toward the heart and neck. Start with the feet and brush upward to the knees, groin, abdomen, and chest. Then brush the hands and arms to the armpits. Read more about dry brushing and lymphatic flow here.
Lipedema reduction surgery is a spin-off of liposuction focused on reducing lipedema tissues, including fibrous tissue, fat, and extracellular contents. It is possible for lymphatics to be injured by a suction cannula during lipedema reduction surgery and/or cosmetic liposuction. Some argue whether this is possible, but studies show it can, and unfortunately, may happen for some. In a recent study published in the American Journal of Case Reports, According to a study by Wright and Herbst confirms that this can occur. So, it is essential if you have lipedema or suspect you may have lipedema that you get a proper diagnosis and work closely with skilled surgeons well-versed in lipedema, lymphatics, and lymphedema for the best possible outcomes and treatment plan before you proceed with any type of liposuction.
During liposuction, some temporary interruption to the lymphatic vessels is unavoidable. In most patients, the lymphatics return to normal in the postoperative period, especially for patients with underlying normal lymphatic function [ Read patients without lymphedema or lipedema]. Suction lipectomy with small blunt cannulas and surgical techniques focusing on avoiding lymphatic damage has been reported to halt lipedema progression. [Sandofer 1, 2] A modification of suction lipectomy can result in alleviating or at least improving the swelling, leg heaviness, and fatigue, the need for limb compression, and the need for lymphatic massage in women with lipedema. In patients with impaired lymphatic function such as chronic lymphedema (or lipedema), careful suction lipectomy using techniques to avoid lymphatic injury can result in improved lymphatic function and a decreased rate of secondary infection or cellulitis in the affected limbs. [Gould. Van de Pas 3,4,]. Once you understand that lymphatics are impaired in lipedema and you understand that lymphatic injury can occur, the natural question arises – How can we protect the lymphatic system in lipedema surgery? Read more about surgical treatments for lipedema here, and contact Dr. Wright and his team at St. Louis Laser Lipo & Vein Center to see what kind of plan is best for you!
Living with lipedema can be a challenging and isolating experience. It’s a condition that affects millions of people around the world, and yet it’s not widely understood or recognized by healthcare professionals. If you’re living with lipedema, you know how frustrating it can be to deal with the physical and emotional symptoms that come with it. But the good news is that there are coping strategies you can use to help empower yourself and take control of your life.
In this article, we’ll explore some of the most effective coping strategies for living with lipedema, from self-care practices to seeking support from others. Whether you’re newly diagnosed or have been living with lipedema for years, these strategies can help you feel more empowered, confident, and in control of your life. So let’s dive in and discover how you can start living your best life with lipedema today!
Lipedema is a chronic condition that affects mostly women, causing an abnormal accumulation of fat cells in the legs, hips, and sometimes arms. It’s often misdiagnosed as obesity or lymphedema, which can be frustrating for those living with it. However, it’s important to understand that lipedema is a medical condition that requires specialized care and treatment.
While the exact cause of lipedema is unknown, hormone imbalances and genetics are thought to play a role. Symptoms of lipedema may include pain, swelling, and sensitivity to pressure in the affected areas. It’s important to work with a healthcare professional who is knowledgeable about lipedema to receive an accurate diagnosis and appropriate treatment.


Living with lipedema can have a significant emotional impact on those affected. It’s not uncommon to feel self-conscious or embarrassed about the appearance of the affected areas, which can lead to anxiety, depression, and even social isolation. It’s important to acknowledge and address these feelings in order to cope with lipedema effectively.
One coping strategy is to focus on self-care and self-love. This can include practices such as positive self-talk, engaging in activities that bring joy, and practicing mindfulness and meditation. It’s also important to seek support from others, whether that’s through a support group or individual therapy.
While there is no cure for lipedema, there are coping strategies that can help manage symptoms and improve quality of life. One such strategy is maintaining a healthy lifestyle. This can include regular exercise, a nutritious diet, and stress-reducing practices such as yoga or tai chi.
Compression garments can also be helpful in managing symptoms such as pain and swelling. These garments work to improve circulation and reduce fluid buildup in the affected areas. It’s important to work with a healthcare professional to find the right type and fit of compression garment for your individual needs.
Another coping strategy is to practice good skincare. This can include moisturizing regularly, avoiding tight clothing, and protecting the skin from sun damage. These practices can help prevent skin irritation and infections, which can be common in those with lipedema.
Maintaining a healthy lifestyle is key in managing lipedema symptoms. Regular exercise can help improve circulation and reduce inflammation in the affected areas. This can include low-impact activities such as walking, swimming, and cycling.
A nutritious diet can also be helpful in managing lipedema symptoms. Foods that are high in antioxidants, such as fruits and vegetables, can help reduce inflammation. It’s also important to stay hydrated by drinking plenty of water throughout the day.
Stress-reducing practices such as yoga, meditation, and deep breathing can also be helpful in managing lipedema symptoms. These practices can help reduce anxiety and improve overall well-being.
Finding support from others who understand what you’re going through can be incredibly helpful in managing lipedema. There are a number of lipedema communities and resources available online and in person.
Online communities, such as Facebook groups and forums, can provide a space to connect with others, share experiences, and find support. In-person support groups can also be helpful in providing a sense of community and connection.
There are also a number of lipedema organizations and resources available, such as the Lipedema Foundation and the National Lymphedema Network. These organizations provide education, resources, and support for those living with lipedema.


Practicing mindfulness and meditation can be helpful in coping with the emotional and physical symptoms of lipedema. Mindfulness involves being present and fully engaged in the present moment, while meditation involves focusing the mind and relaxing the body.
There are a number of mindfulness and meditation practices that can be helpful in managing lipedema symptoms. These can include deep breathing exercises, guided meditations, and body scans. It’s important to find a practice that works for you and to make it a regular part of your self-care routine.
Regular exercise can be helpful in managing lipedema symptoms, but it’s important to choose exercises that are low-impact and gentle on the affected areas. Walking, swimming, and cycling are all great options, as they help improve circulation without putting too much pressure on the legs.
Yoga and tai chi can also be helpful in managing lipedema symptoms. These practices focus on gentle movements and breathing, which can help reduce stress and improve overall wellbeing.
It’s important to work with a healthcare professional or certified fitness instructor to find the right type and intensity of exercise for your individual needs.
While there is no cure for lipedema, there are a number of treatment options that can help manage symptoms. These can include manual lymphatic drainage, which is a type of massage that helps improve lymphatic flow and reduce swelling. Compression therapy, as mentioned earlier, can also be helpful in managing symptoms. It’s essential to work with a healthcare professional who is knowledgeable about lipedema to determine the best treatment options for your individual needs.
Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the collection of fat cells, which can cause the obstruction of lymphatic capillaries (branch-like blood vessels).
Extra care must be taken to avoid injuring the lymphatic system and making an already stressed system worse. Using blunt cannulas generous and special surgical techniques, studies have shown that lymphatic function can actually improve after this type of liposuction in women with Lipedema. The goal of lipedema reduction surgery is to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a debulking surgery, not a cosmetic surgery.
Two specialized liposuction techniques have been shown in studies to benefit individuals with lipedema: water-assisted and tumescent liposuction. In addition to the surgical equipment used, it is important to choose a surgeon with experience and who is cautious when performing lipedema surgery. These factors can have an essential influence on protecting lymphatic flow and function.
Lipedema Reduction Surgery or Lymph Sparing Liposuction has been shown to improve pain, swelling and quality of life of women with lipedema. New research by Dr Wright is showing that Lipedema Reduction Surgery can improve the knee mechanics and mobilty of women with lipedema comparable to or better than replacing a knee joint of someone with end stage arthritis in their knee.
Living with lipedema can be challenging in the workplace, particularly if your job requires a lot of standing or sitting. It’s important to take breaks throughout the day to stretch and move around and to wear comfortable clothing and footwear.
Communicating with your employer about your condition and needs can also be helpful. This can include requesting accommodations such as a standing desk or a flexible schedule.
It’s important to remember that you are not alone in your experience with lipedema and that there are strategies and resources available to help you succeed in the workplace.
Living with lipedema can be a challenging and isolating experience, but it’s important to remember that there are coping strategies and resources available to help you manage symptoms and improve your quality of life. From self-care practices to seeking support from others, these strategies can help you feel more empowered, confident, and in control of your life.
It’s important to work with a healthcare professional who is knowledgeable about lipedema to receive an accurate diagnosis and appropriate treatment.
Additionally, finding support from others who understand what you’re going through can be incredibly helpful in managing lipedema.
By practicing mindfulness, maintaining a healthy lifestyle, and utilizing treatment options such as manual lymphatic drainage and compression therapy, you can take control of your life with lipedema and live a fulfilling life. Remember, you are not alone in your experience; there is hope for a brighter future.
June is Lipedema Awareness Month, a time dedicated to raising awareness, providing resources, sharing knowledge, and advocating for equitable healthcare for patients with this complicated, misunderstood, and often misdiagnosed disease. This article will explore the history of lipedema, its symptoms, stages, diagnosis, treatment options, and the importance of research and awareness campaigns. By understanding the key aspects of lipedema and its management, we can help support those affected by the condition and contribute to a more informed and inclusive healthcare system.
Lipedema is a fat disorder that mainly affects women and causes enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Medical professionals often misdiagnose and dismiss lipedema as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
Women suffering from Lipedema often report the disease associated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.
Lipedema is characterized by an abnormal accumulation of fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected, but the condition can also spread to the torso and arms. Symptoms of lipedema can be debilitating, and the fat cells associated with the condition are resistant to both diet and exercise programs.
Some common symptoms of lipedema include:
Lipedema progresses through three distinct stages, each with its own set of characteristics:
Several conditions can present similar symptoms to lipedema, making accurate diagnosis challenging. These conditions include:
Obtaining a correct lipedema diagnosis is crucial for effective treatment and management. Diagnosis typically involves a combination of a physical exam, patient questionnaires, and additional testing, such as ultrasounds or Doppler imaging. Some diagnostic tests used to differentiate lipedema from related conditions include:
While there is no definitive cure for lipedema, several treatment options can help manage the condition and improve the patient’s quality of life. These treatments may include:


Liposuction: This surgical intervention removes excess fat deposits and may provide long-term relief for some lipedema patients. However, it should be considered in consultation with a qualified healthcare professional and as part of a comprehensive treatment plan.


Despite being identified over 80 years ago, lipedema remains under-researched and poorly understood. Increased research efforts can lead to improved diagnostic techniques, better treatment options, and a deeper understanding of the condition’s underlying causes. Lipedema Awareness Month serves as an opportunity to raise awareness of the condition, educate healthcare professionals and the public, and support ongoing research initiatives.
There are several ways to participate in Lipedema Awareness Month and support patients living with the condition:
Lipedema Awareness Month is a crucial time for raising awareness, providing resources, and advocating for patients living with this often misunderstood and misdiagnosed condition. By educating ourselves and others, supporting research efforts, and promoting inclusive healthcare policies, we can contribute to a more informed and compassionate healthcare system for all those affected by lipedema.
Lipedema, a condition characterized by abnormal fat accumulation in the lower body, affects millions of women worldwide but remains largely underdiagnosed. The disorder can cause swelling, discomfort, and mobility issues, often leading to body image struggles and self-consciousness. Despite this, several celebrities have courageously opened up about their experiences with Lipedema, aiming to empower others and raise awareness about the condition. In this article, we highlight ten celebrities with lipedema who embraced their Lipedema diagnosis and continue to lead successful lives in the spotlight.
Lipedema is a condition that primarily affects women and is characterized by painful swelling of the legs and buttocks. It is known as a “painful fat disorder” because it causes fat to accumulate in the lower body, leading to discomfort and difficulty moving.
Lipedema can be challenging to diagnose because its symptoms are often similar to other conditions, such as obesity and lymphedema. Additionally, the cause of lipedema is still unknown, although it is believed to be a genetic disorder triggered by hormonal changes.


British-American actress Mischa Barton is known for her stellar performances on both the big screen and television. Although not officially confirmed, the appearance of her legs in numerous paparazzi shots suggests that Barton could have Lipedema. Despite the challenges of living with this condition, Barton has continued to excel in her career, proving that Lipedema does not define one’s success or talents.


Canadian singer-songwriter Nelly Furtado has been open about her struggles with self-image and body proportions. Her pear-shaped body, a common characteristic of Lipedema, has not deterred her from becoming a Grammy Award-winning artist. Furtado is a prime example of how embracing one’s unique qualities and focusing on one’s talents can lead to great achievements, despite living with Lipedema.


British actress Maisie Smith, known for her roles in television and film, has also been suspected of having Lipedema due to the appearance of her legs. While Smith has not explicitly discussed her condition, her success in the entertainment industry demonstrates that a Lipedema diagnosis does not need to overshadow one’s accomplishments.


Kelly Clarkson, a famous singer and songwriter, has openly discussed her struggles with Lipedema. Diagnosed in 2006, Clarkson has managed her symptoms through lifestyle changes, healthy eating, and proper treatment. Her openness about her condition and continued success in the music industry serves as an inspiration for those living with Lipedema.


Television personality and radio host Wendy Williams has vocalized her experience with Lipedema and its associated challenges. Williams has tried to maintain a healthy lifestyle and balance her weight while living with the condition. Her transparency about her Lipedema journey has brought awareness to the issue and paved the way for more open conversations about the condition.


Reality TV star Shaughna Phillips, known for her appearance on Love Island, has openly shared her struggles with Lipedema. After her diagnosis, Phillips underwent liposuction to remove excess fat deposits from her legs. Her candid discussion of the condition and its impact on her life has helped raise awareness and empower others facing similar challenges.
Lipedema has characteristic shapes and sizes on the legs and arms, which can lead to speculation about the existence of lipedema. Of course, we must caution ourselves and others that there are clinical symptoms and specific signs on a physical exam that lead to an official diagnosis. It’s only with a good history and physical exam by a physician experienced with Lipedema that a diagnosis can be provided.
The following celebrities have been speculated to have lipedema based on photos and videos. However, they have not communicated that they have been diagnosed with lipedema.


Emmy and Golden Globe-winning actress Kathy Bates has been open about her Lymphedema diagnosis, however, there is widespread speculation that she has Lipedema. While the two share many characteristics and their treatment shares some overlap, they are two different diseases, have different complications, and require different care.
After years of struggling to find a treatment that worked for her, Bates found a doctor who understood her condition and helped her manage its symptoms effectively. Bates’ story highlights the importance of finding the right medical professional to help manage Lymphedema and its impact on one’s life and career. Bates has since become an advocate for women experiencing similar stories, as seen through her work with the Lymphatic Education & Research Network.


Legendary singer Mariah Carey has faced speculation about her possible Lipedema diagnosis due to her body proportions. If true, Carey has successfully maintained an influential career in the music industry without this disease affecting her. It’s hard to imagine a holiday season passing without hearing her voice in “All I Want for Christmas.”


Award-winning singer-songwriter Alicia Keys has been speculated to have Lipedema due to the visible fat accumulation around her thighs and lower tummy areas. Although not officially diagnosed, Keys has shown resilience and determination throughout her career. If she has been diagnosed and simply not addressed it publicly, this is another example that Lipedema does not need to hold anyone back from achieving greatness in their chosen field.


Comedian and actress Amy Schumer is another celebrity suspected of having Lipedema due to her thicker legs. Though Schumer has not confirmed her diagnosis, she has made waves in the entertainment industry. If she has Lipedema, her success proves that Lipedema does not define one’s talents or capabilities. Additionally, she’s one of the loudest and proudest for adopting body positivity.


There have been claims about whether or not parts of Kim Kardashian’s body are real or the result of implants, and there’s also debate on whether her body shape is due to Lipedema or plastic surgery. Several outlets report that Kim has said she’s been diagnosed with Lipedema, but there are no known ways to prove if she stated this or not. Either way, Kim has made a name for herself as one of the most famous and wealthy celebrities in the world, with a large part of her reputation surrounding her body and its Lipedema-like proportions.
Celebrities with Lipedema are powerful examples of resilience, determination, and self-acceptance. Their stories of struggle and triumph inspire others battling the condition to embrace their unique qualities and continue pursuing their passions. By raising awareness and fostering open conversations about Lipedema, these celebrities are helping to break the stigma surrounding the condition, encouraging those affected to seek support and treatment and empowering them to lead fulfilling lives despite their diagnosis.
Lipedema is a chronic condition that affects many women, causing painful swelling in their legs and arms. The swelling can be so severe that it affects their mobility and quality of life. While there is no cure for Lipedema, there are ways to manage its symptoms. One of the most effective ways is to practice Lymphatic Yoga. This form of yoga is specifically designed to help stimulate the lymphatic system, which removes waste and toxins from the body.
By practicing Lymphatic Yoga, people with Lipedema can improve their circulation, reduce inflammation, and ease their pain. In this article, we’ll explore the benefits of Lymphatic Yoga for people with Lipedema and how it can be incorporated into their daily routine.
Lymphatic Yoga is a gentle form of yoga that involves fluid movements, breathing exercises, and mindfulness techniques. It is designed to stimulate the lymphatic system, which is crucial to our body’s immune system. The lymphatic system is a network of vessels and nodes that transport lymph, a clear fluid that contains white blood cells, throughout the body. The lymphatic system helps to remove waste, toxins, and excess fluid from the body. When the lymphatic system is not working properly, it can lead to a buildup of fluid in the tissues, causing swelling and inflammation.
Lymphatic Yoga helps to stimulate the lymphatic system by using gentle movements and deep breathing. The movements are designed to create a pumping action that helps to move the lymphatic fluid throughout the body. Deep breathing helps to increase oxygen levels in the body, which can also help to reduce inflammation. By practicing Lymphatic Yoga, people with Lipedema can improve their lymphatic flow, reduce swelling, and ease their pain.
Lipedema is a chronic condition that affects mostly women. It is characterized by the abnormal accumulation of fat and fluids in the legs, thighs, and buttocks. The swelling is usually symmetrical, meaning it affects both legs equally. Lipedema can also affect the arms and can cause pain, tenderness, and bruising. The exact cause of Lipedema is unknown, but it is thought to be related to hormonal imbalances and genetics.
Lipedema is often misdiagnosed or mistaken for obesity, leading to frustration and a delay in treatment. It is essential to recognize the symptoms of Lipedema and seek treatment early. Treatment options include compression therapy, manual lymphatic drainage, and Lymphatic Yoga.
Lymphatic Yoga can be an effective way to manage Lipedema symptoms. By stimulating the lymphatic system, Lymphatic Yoga can help to reduce swelling and inflammation. It can also improve circulation, which can help to reduce pain and discomfort. Lymphatic Yoga can be done at any time of the day and modified to suit individual needs and abilities.
The gentle movements and deep breathing of Lymphatic Yoga can help to stimulate the lymphatic system. The movements are designed to create a pumping action that helps to move the lymphatic fluid throughout the body. This can help to reduce the buildup of fluid in the tissues, which is a common symptom of Lipedema. Deep breathing can also help to increase oxygen levels in the body, which can help to reduce inflammation.
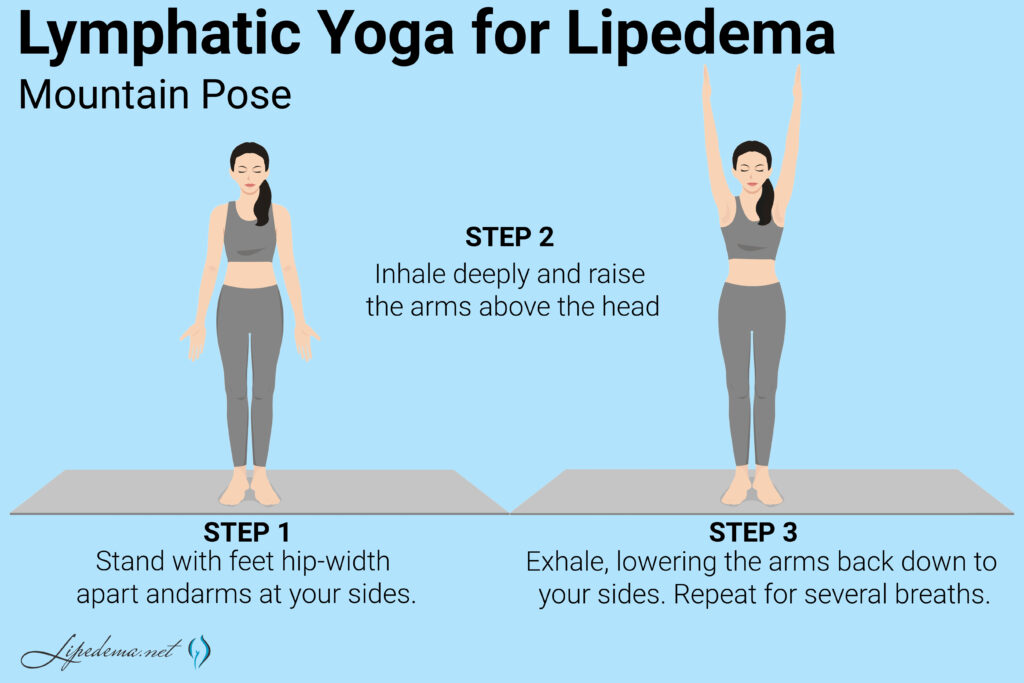
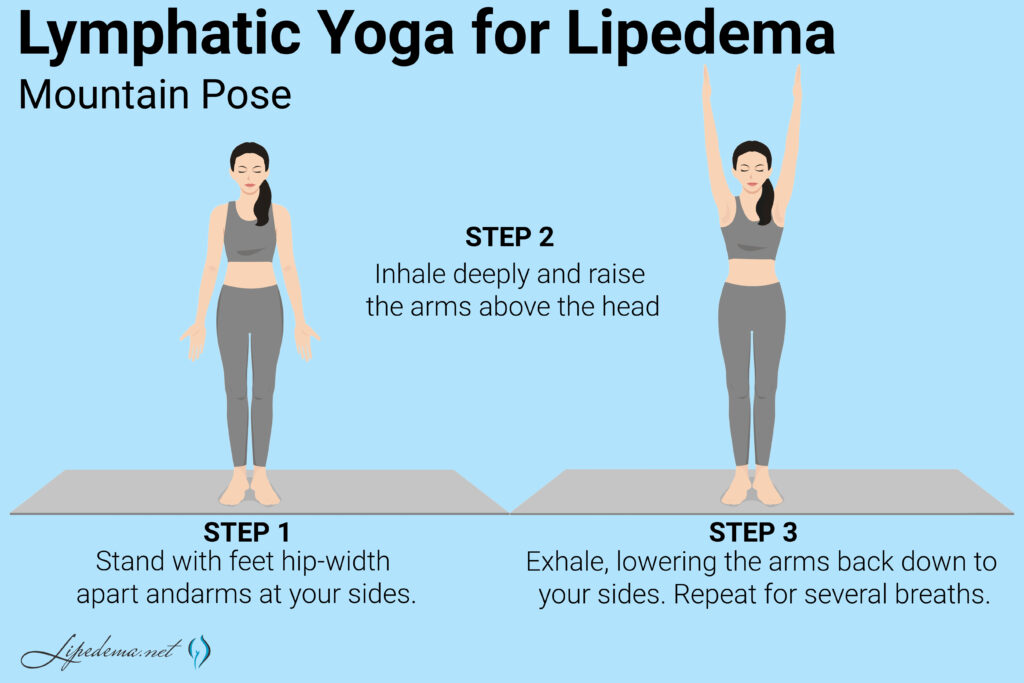
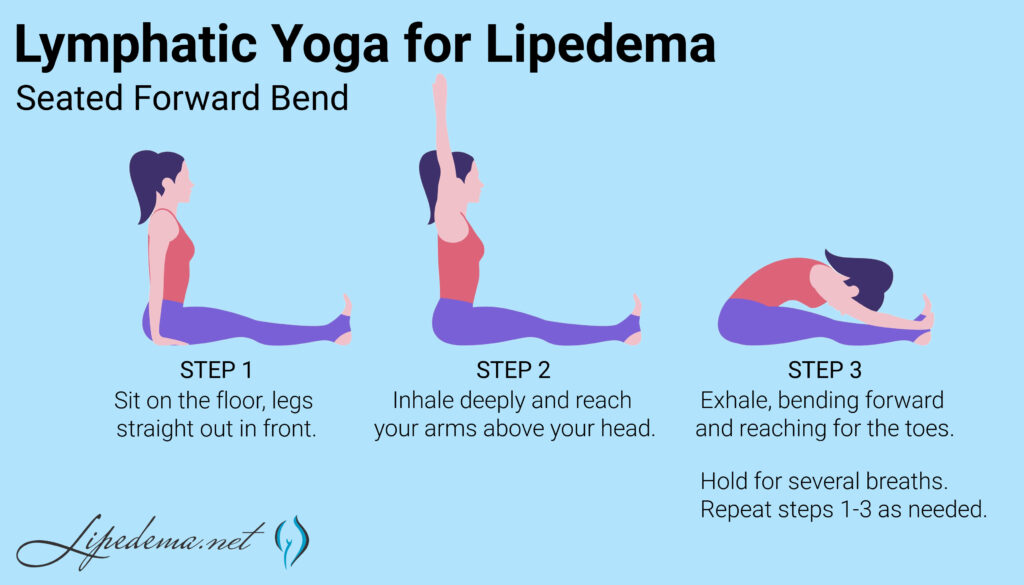
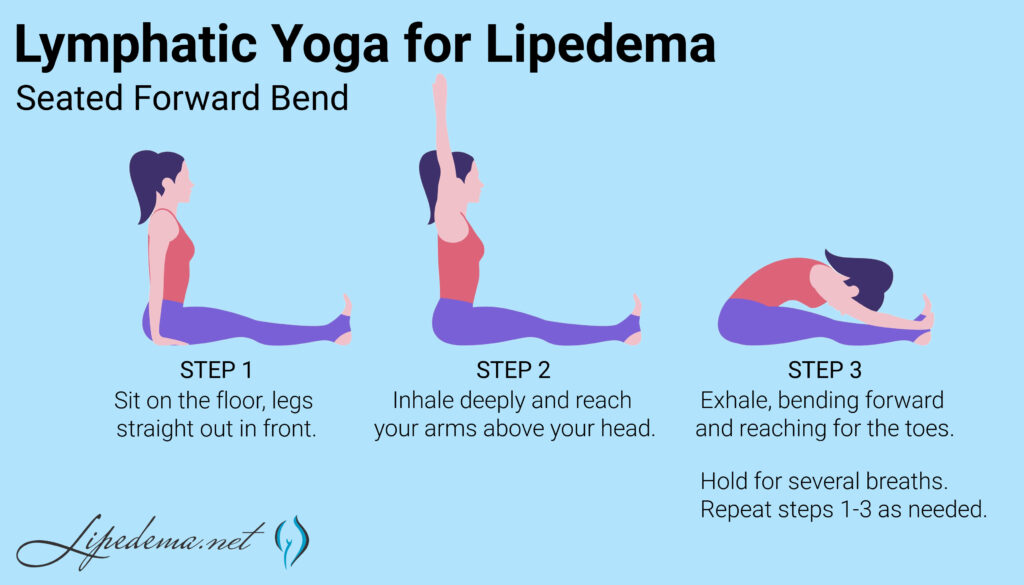
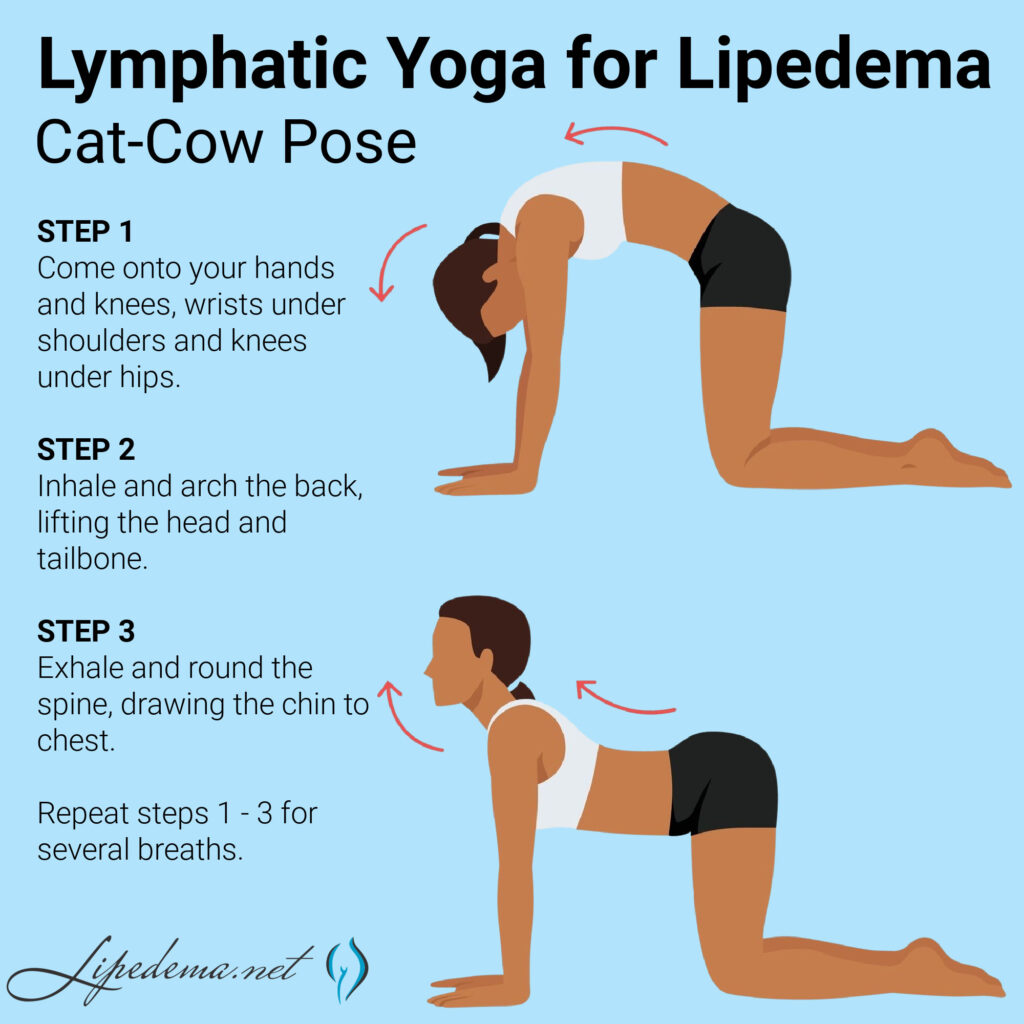
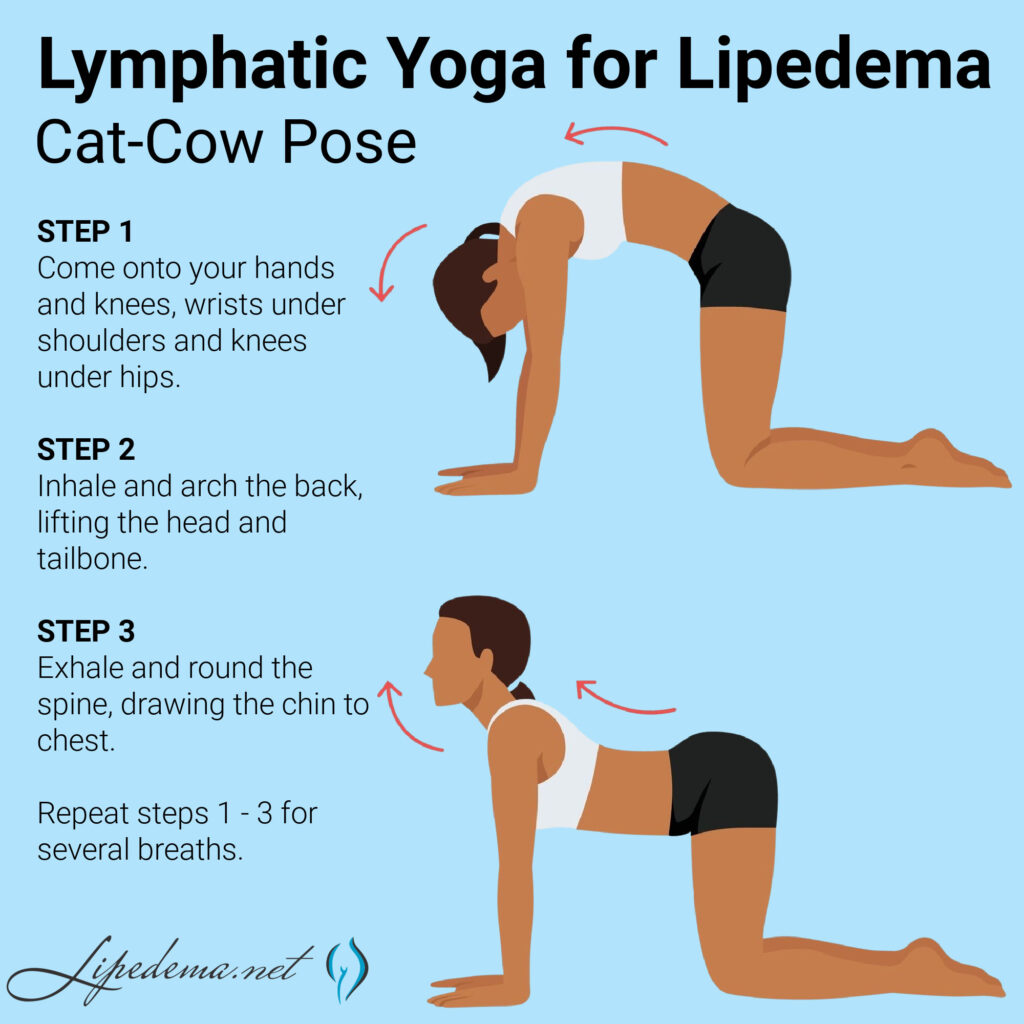
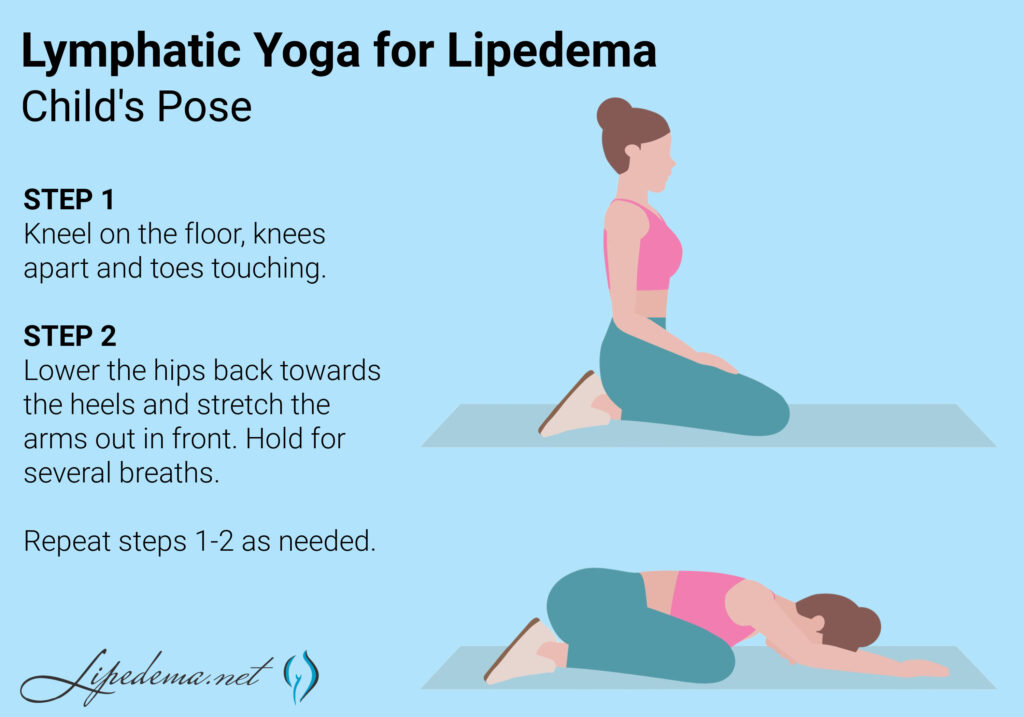
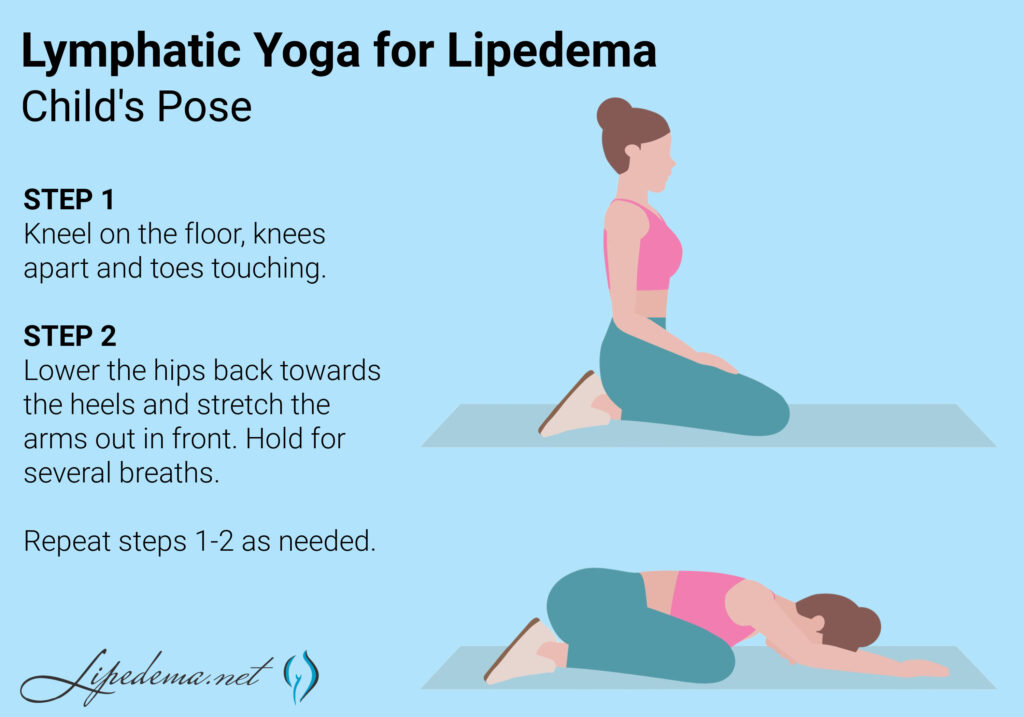
Several Lymphatic Yoga poses can be used to reduce swelling and pain associated with Lipedema. These poses are gentle and can be modified to suit individual needs and abilities.
Here are some Lymphatic Yoga poses that can be helpful for people with Lipedema:
Lymphatic breathing techniques can be used to help improve lymphatic flow and reduce swelling. These techniques involve deep breathing and can be done at any time of the day.


Here are some lymphatic breathing techniques that can be helpful for people with Lipedema:
Lymphatic self-massage can be used to help improve lymphatic flow and reduce swelling. This technique involves gentle massage movements that help to move the lymphatic fluid throughout the body.
Here are some lymphatic self-massage techniques that can be helpful for people with Lipedema:
Incorporating Lymphatic Yoga into your daily routine can be a great way to manage Lipedema symptoms. Here are some tips for getting started:
In addition to Lymphatic Yoga, other natural remedies can help manage Lipedema symptoms.
These include:
Lipedema can be challenging to manage, but there are ways to reduce its symptoms. Lymphatic Yoga is a gentle and effective way to stimulate the lymphatic system, reduce inflammation, and ease pain associated with Lipedema. Incorporating Lymphatic Yoga into your daily routine can improve your lymphatic flow, reduce swelling, and improve your overall quality of life. Remember to start slow, be consistent, and listen to your body. With time and practice, you can find relief from your Lipedema symptoms and enjoy a more active and comfortable life.
Lymphedema is a condition that causes swelling in the limbs due to a buildup of lymph fluid. Various factors, including surgery, radiation therapy, and infection, can cause it. While lymphedema can be managed with proper treatment and self-care, traveling can present unique challenges for those with the condition. This article will discuss some tips for traveling with lymphedema to help you stay comfortable and healthy on your next trip.
Lymphedema is a condition that affects the lymphatic system, which is responsible for draining excess fluid from the body’s tissues. When the lymphatic system is not working properly, fluid can build up in the limbs, causing swelling and discomfort. This can make it challenging to move around and perform daily activities and increase the risk of infection.
For those with lymphedema, traveling can exacerbate these symptoms. Long periods of sitting or standing can cause fluid to pool in the limbs, leading to increased swelling and discomfort. Changes in altitude during air travel can also affect the lymphatic system, making it more difficult for the body to drain excess fluid.
Fortunately, there are several steps you can take to manage lymphedema while traveling. Here are some tips to help you stay comfortable and healthy on your next trip:
Before you travel, plan ahead to ensure you have everything you need to manage your lymphedema. This may include compression garments, bandages, or other medical supplies. If you are traveling by air, it is also a good idea to contact the airline ahead of time to request special accommodations, such as extra legroom or assistance with boarding.


Staying hydrated is important for everyone, but it is especially important for those with lymphedema. Drinking plenty of water can help to flush excess fluid from the body and reduce swelling. Bring a refillable water bottle with you and drink plenty of fluids throughout your trip.
Sitting or standing for long periods can cause fluid to pool in the limbs, leading to increased swelling and discomfort. To prevent this, try to move around as much as possible during your trip. Take frequent breaks to stretch your legs, walk around the cabin during a flight, or stop at rest areas during a road trip to get out and move around.
Compression garments are designed to help improve circulation and reduce limb swelling. If you have lymphedema, wearing compression garments can be especially helpful during travel. Wear your compression garments as directed by your healthcare provider and pack extra pairs in emergencies.


Elevating your legs can help reduce swelling and improve limb circulation. If you are traveling by car or train, try to elevate your feet on a pillow or blanket. If traveling by air, consider booking a seat with extra legroom or bringing an inflatable footrest to help elevate your legs during the flight.
Tight clothing can restrict circulation and exacerbate lymphedema symptoms. When packing for your trip, choose loose-fitting clothing that is comfortable and allows for easy movement. Avoid tight socks, stockings, or other clothing that may restrict limb circulation.
Traveling with lymphedema can be challenging, but with proper planning and self-care, staying comfortable and healthy on your next trip is possible. Remember to plan ahead, stay hydrated, move around as much as possible, wear compression garments, elevate your legs, and avoid tight clothing. Following these tips allows you to enjoy your travels without letting lymphedema symptoms get in the way.