
Lipedema is a common but not well recognized subcutaneous fat storage disorder. Some of the reasons it is poorly recognized are that lipedema can present in many forms and it is not very well known among medical professionals. It is often confused with Obesity and Lymphedema, which are more common and becoming even more so. The exact cause or causes of lipedema are not known. However, there appears to be a pattern of inheritance in 60% of women. Learn the cause of lipedema below!
While lipedema is likely inherited, the pathologic physiologic mechanism responsible for lipedema is not fully known. Medical research so far has given students and experts of the disease much to think about and consider. There are over a dozen of well-designed studies that are currently trying to better diagnose, understand, and treat lipedema. The author of this page participates currently in five studies to better understand the disease, its pathologic mechanism, and how to better treat it. In a recent article titled, ”Pathophysiological dilemmas of lipedema.” Dr. Szel discusses the three most compelling hypotheses for the cause of lipedema. The goal of this page is to use the current medical literature to share some educated thoughts about what is likely causing lipedema.
Hormones
Hormones have often been suspected as a cause of lipedema because lipedema almost exclusively occurs in women. Although it has been seen in some men who have hormone imbalances. Estrogen plays a role in fat metabolism. Estrogen receptors in adipose tissue can lead to differences in the lipolysis activity of the adipose tissue. For example, a decrease in alpha estrogen receptors and an increase in beta receptors leads to decreased lipolysis and increased fat deposition. Lipedema could be a result of differences in the number of estrogen receptors in the subcutaneous fat on buttocks arms and legs. Or just possible that there is a decreased signal in the estrogen receptors. While this is not proven yet, it could explain the development of lipedema during puberty and worsening during hormonal events such as childbirth.
A gene for Lipedema was recently discovered by the Journal of International Molecular Science. The gene that is associated with family members of women with Lipedema codes for the gene Aldo ketoreductase. The enzyme Aldo-keto reductase is responsible for the metabolism of progesterone. This finding makes sense in that it could be an important cause of lymphedema.
Estrogen and progesterone are known to affect the deposition of fat in the subcutaneous tissue. We know that when girls go through puberty they deposit more fat on their hips and thighs. Estrogen regulates body energy homeostasis and plays a role in the metabolism of fat including subcutaneous fat. Progesterone reverses the weight reduction actions of estradiol. A deficiency in the Aldo keto reductase would lead to increased progesterone in subcutaneous tissue.
Impaired Lymphatics
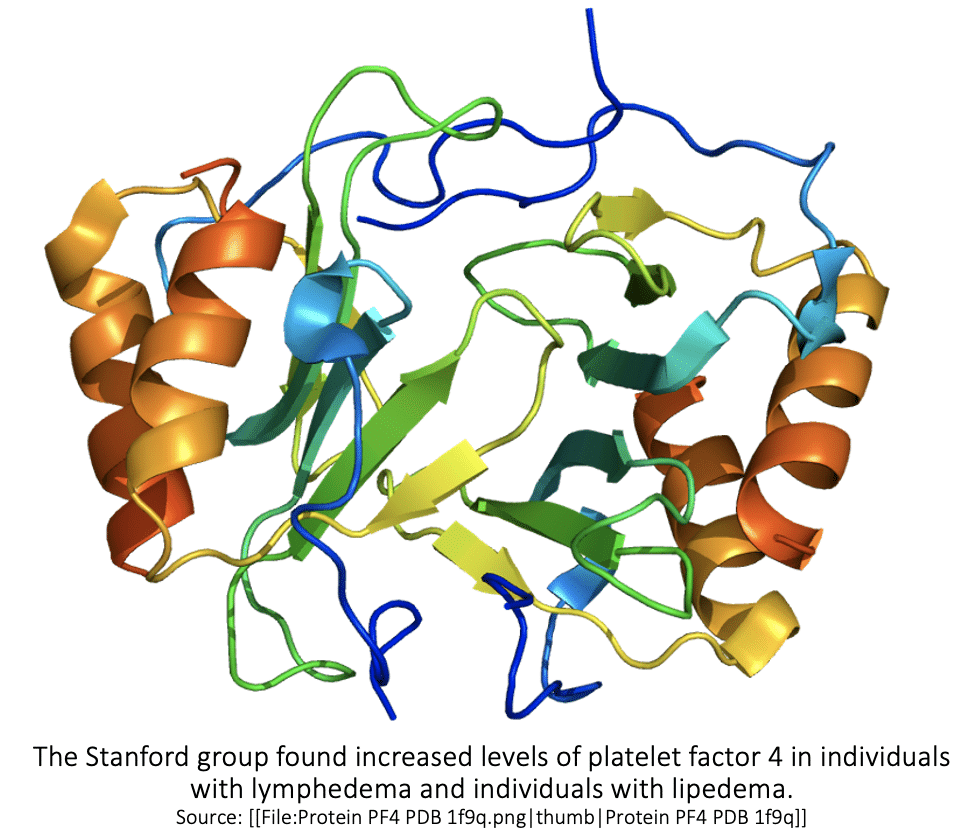
A group of researchers from Stanford University recently found a marker of both inflammation and the lymphatic function called PF4. PF4 stands for platelet factor four. Platelet factor 4 is released from platelets in response to injury and other inflammatory substances. The Stanford group found increased levels of platelet factor 4 in individuals with lymphedema and individuals with lipedema. You can read more about PF4 here.
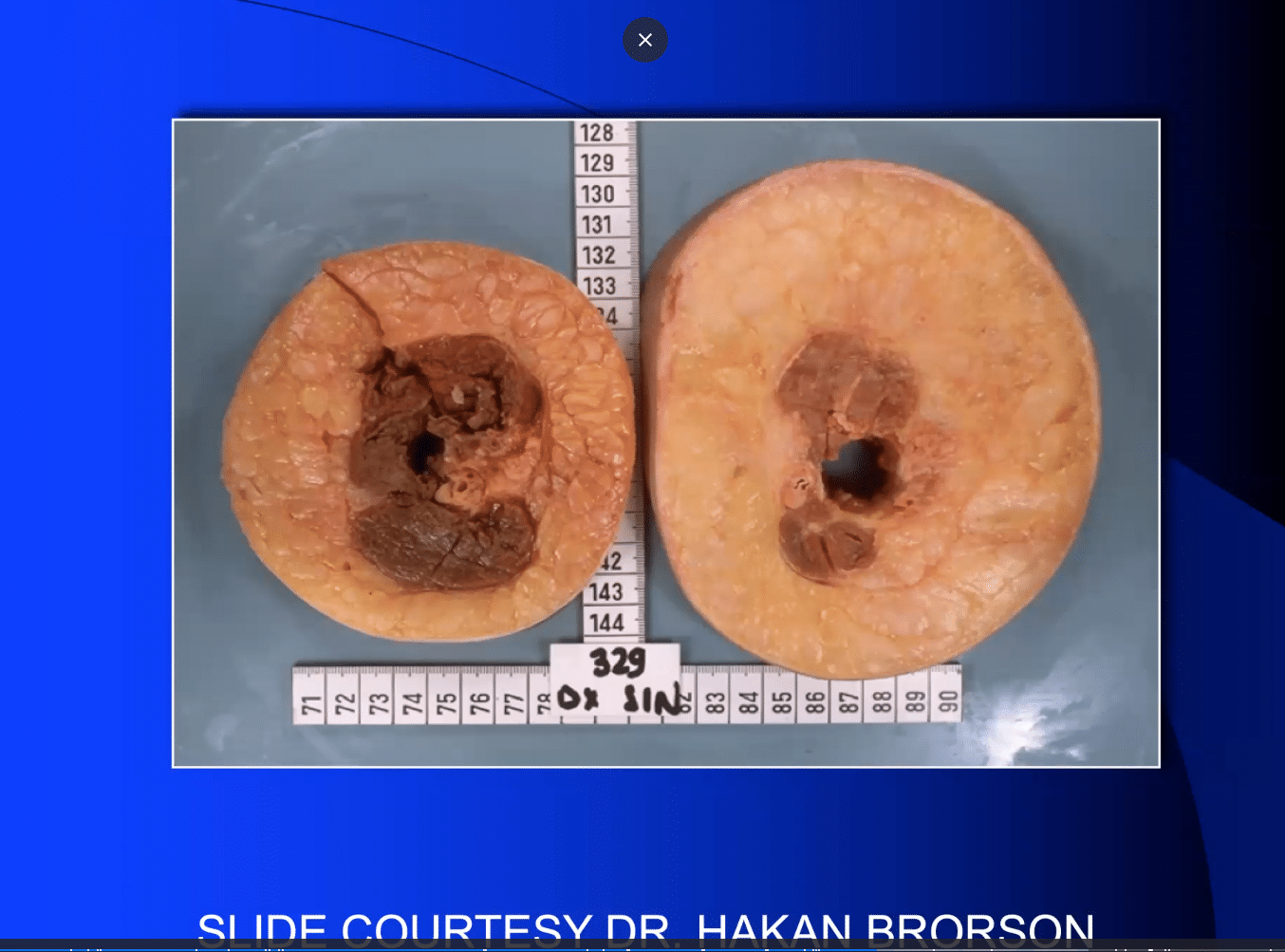
Several studies have shown that there is an impaired lymphatic function in patients with Lipedema. It is known that lymphatic impairment stimulates adipose. Hakan Brorson has shown that lymphedema leads to an increase in fat deposition in affected limbs, seen below.
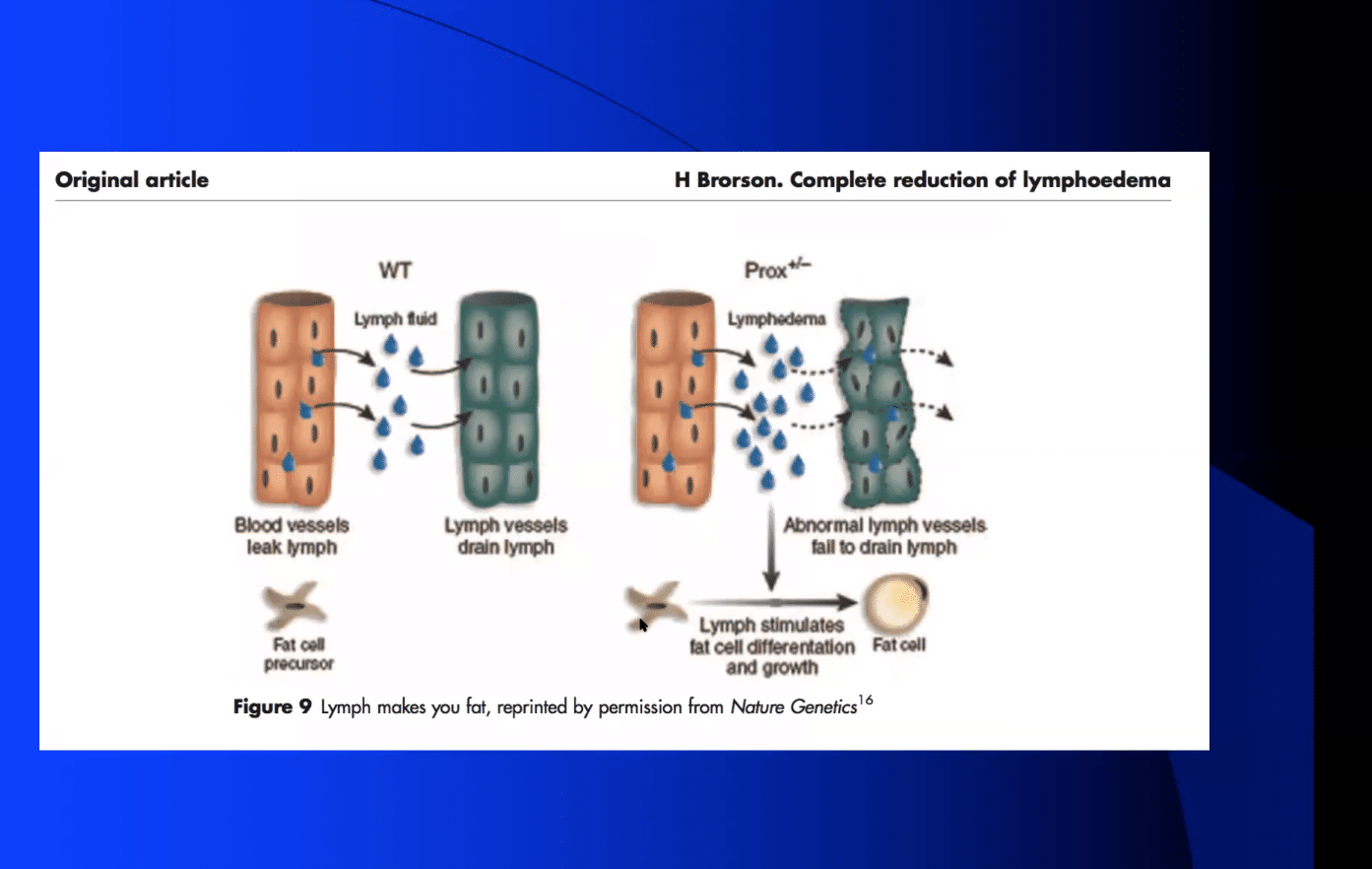
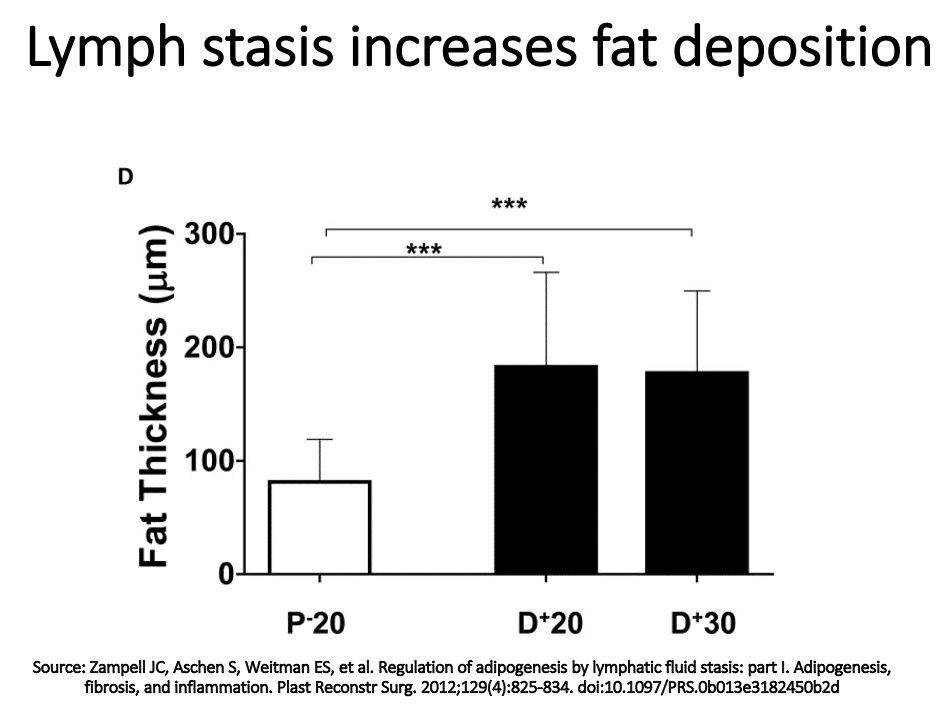
Zampell showed using a mouse tail model that lymphatic injury leading to lymphatic stasis increases fat deposition. These studies take with the evidence of lymphatic impairment in lipedema may explain the mechanism behind the increased fat accumulation on the arms and legs of women with lipedema.
Impaired Vascular Function
Another possible explanation for lipedema is impaired vascular function or vasculopathy. Microangiopathy is seen even in histologic studies of the early stages of lipedema. Tissue expansion by increased fat deposition requires increased vascularity. This tissue expansion causes tissue hypoxia and the tissue hypoxia of adipocytes leads to increased inflammatory markers like Tumor Necrosis Factor, TNF-alpha, and Interleukin 6, IL-6. It also can lead to increase secretion of VEGF.
Lipedema could also be caused by a lymphatic circulation problem. Lymphatic fluid promotes fat cell growth and in the presence of lymphatic fluid, chylomicrons have shown increased growth and differentiation. Or lipedema could be caused by an obstruction of lymphatic capillaries. There have been studies that are showing poor uptake lymph in the pre lymphatic spaces and lymphatic capillaries in lipedema.
Cause of Lipedema: Neuropathy
Finally, lipedema could be caused by neuropathy. A decrease in sympathetic nerve function could cause impaired lipolysis and increased fat accumulation. Dr. Karen Herbst has noticed cutaneous hypothermia in lipedema. Hines noticed that there is an increase in vascular congestion peripherally in lipedema with reddened feet.
New Research on Lipedema Genes
In recent years the number of medical research studies about the causes of lipedema has been increasing. There is also growing interest by experts in the vascular, lymphatic, and fat storage fields to try to more completely understand lipedema. With the ongoing scientific research and increased interest, we may not be far from having a clear understanding of the cause or causes of lipedema.
Read about the causes of lymphological liposculpture here.
Aldo-Keto Reductase 1C1 (AKR1C1) has been marked as the First Mutated Gene in a Family with Nonsyndromic Primary Lipedema. This gene codes for an enzyme that breaks down progesterone and aldosterone. As a result, this gene mutation would result in a slower and less efficient reduction of progesterone to hydroxyprogesterone, and an increased subcutaneous fat deposition in variant carriers.
References:
E. Szél Pathophysiological dilemmas of lipedema. Medical Hypotheses 83 (2014) 599–606.. https://www.ncbi.nlm.nih.gov/pubmed/25200646.
Google Scholar Link
DOI:10.1016/j.mehy.2014.08.011
