Vein flow and lipedema are two distinct but interconnected concepts that are important to understand when it comes to vascular health and the condition known as lipedema. Let’s dive into each of these topics to gain a better understanding.
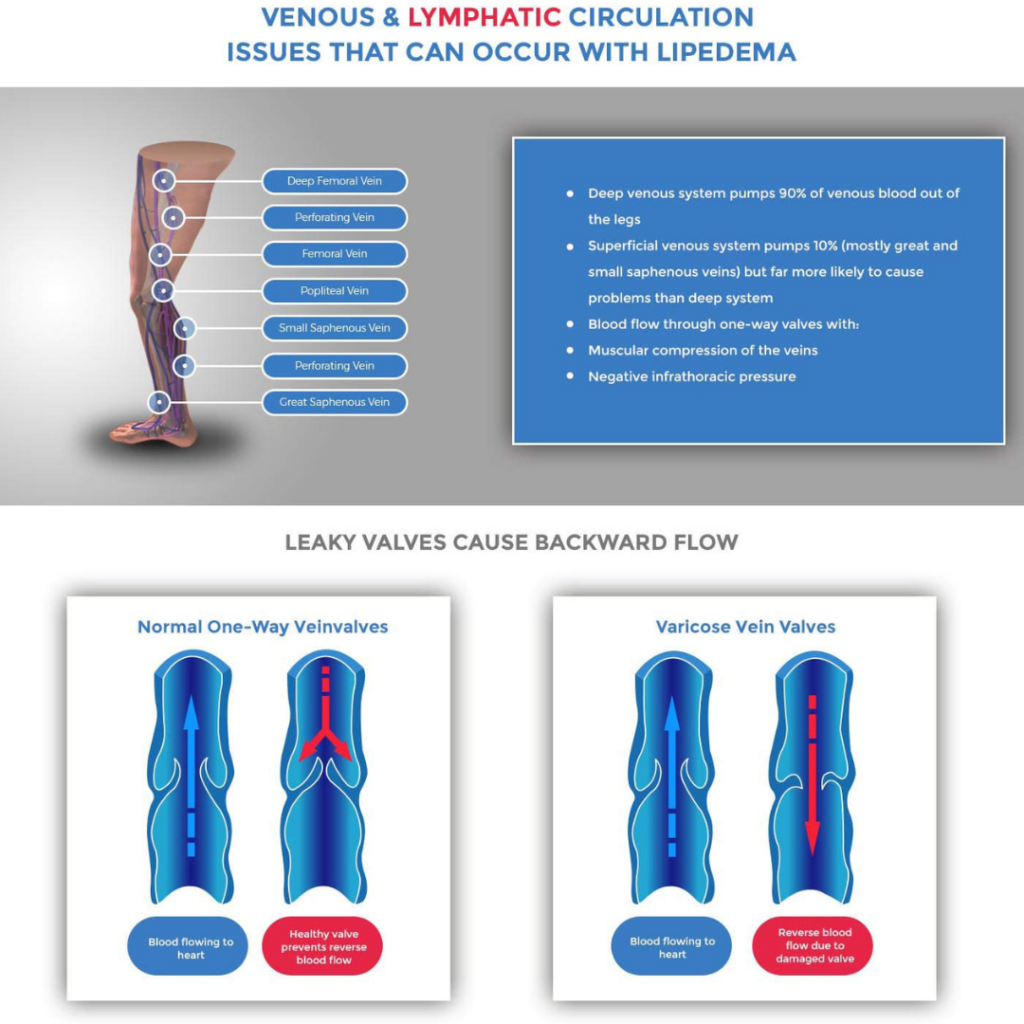
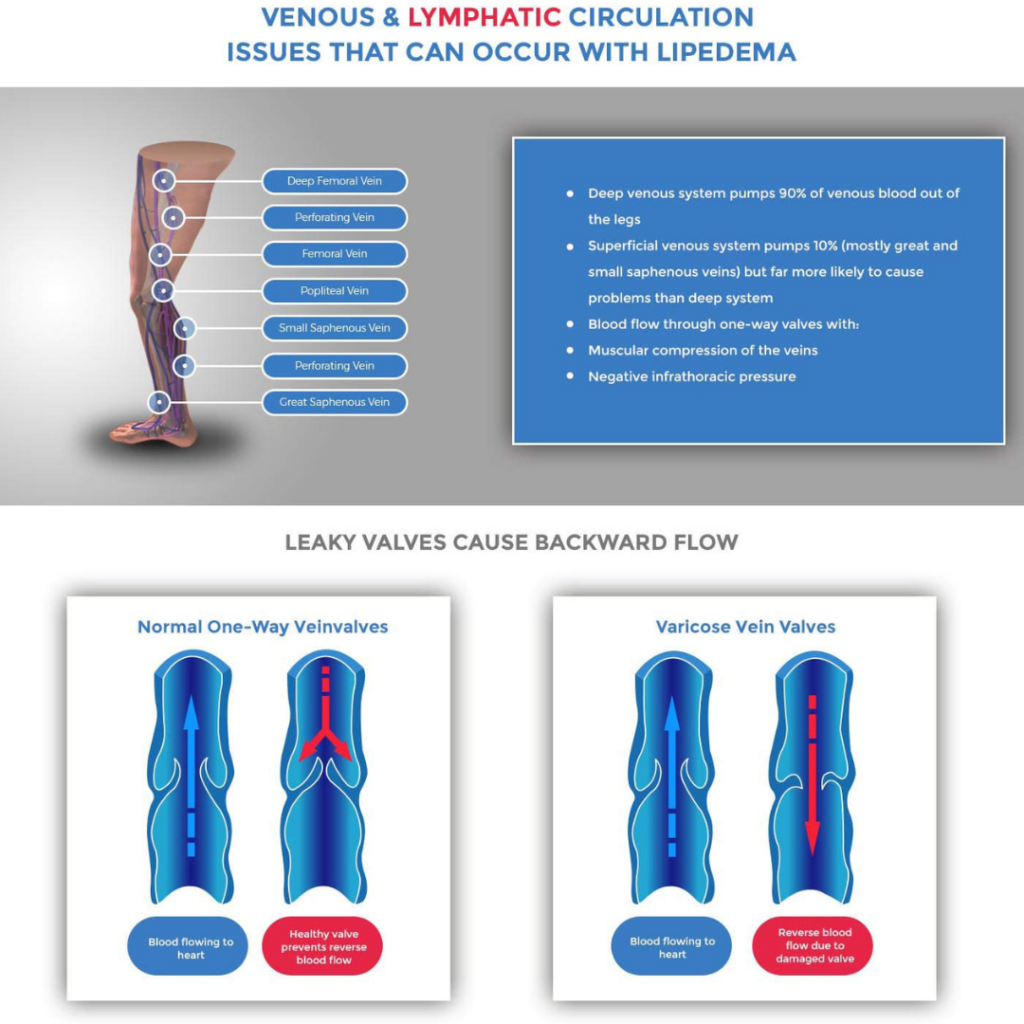
Vein flow, also known as venous blood flow, refers to the movement of blood through the veins in our bodies. Veins play a crucial role in returning deoxygenated blood back to the heart after it has circulated through the body. Vein flow is facilitated by a series of valves within the veins that prevent blood from flowing backward.
Proper vein flow is essential for maintaining healthy circulation and preventing conditions such as venous insufficiency and deep vein thrombosis. However, certain factors can disrupt vein flow, leading to poor circulation and potential health issues. When venous blood is disrupted either by obstruction from deep vein thrombosis (DVT) or by backward blood flow caused by venous insufficiency, it causes changes in the venous pressure, and it changes the biology of the tissue they serve. Below we explain in more detail how the changes in venous pressure cascade downstream to affect lymphatic function.
Now, let’s focus on lipedema, which is a chronic condition characterized by an abnormal accumulation of fat in specific areas of the body, typically the hips, thighs, and lower legs. Lipedema predominantly affects women and is often misdiagnosed or mistaken for obesity or lymphedema.
The exact cause of lipedema is still not fully understood, but it is believed to be related to hormonal imbalances, genetics, and other factors. Lipedema can cause pain, tenderness, swelling, and a disproportionate appearance in the affected areas. It can also lead to mobility issues and emotional distress due to body image concerns.
The connection between vein flow and lipedema lies in the fact that compromised vein flow can contribute to the development or worsening of lipedema symptoms. When vein flow is impaired, it can result in increased fluid retention and inflammation, exacerbating lipedema-related swelling and discomfort.
To manage lipedema effectively, it is crucial to address any underlying venous issues that may be present. This can involve interventions such as compression therapy, exercise, and lifestyle modifications. Additionally, maintaining a healthy weight, eating a balanced diet, and engaging in regular physical activity can also help manage lipedema symptoms.
It’s important to consult with a qualified healthcare professional who specializes in vascular health and lipedema to receive an accurate diagnosis and develop an appropriate treatment plan tailored to your individual needs.
Understanding the relationship between vein flow and lipedema is essential for those affected by this chronic condition. By addressing any underlying venous issues and adopting a comprehensive management approach, individuals with lipedema can experience improved quality of life and better control over their symptoms.
Vein Problems and Lipedema
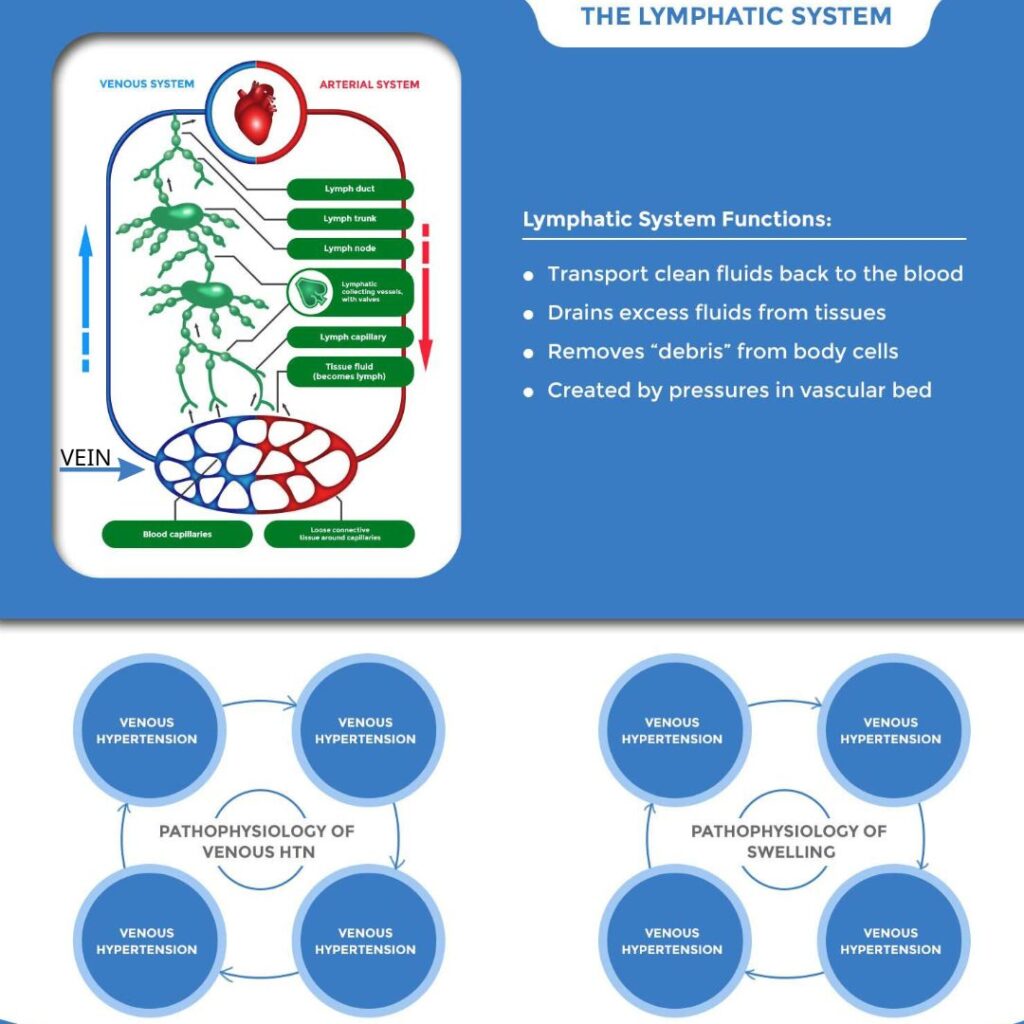
The Venous and Lymphatic circulation systems are intimately intertwined. The pressure in the venous system is the single largest driving force for the production of lymph. Venous disorders such as venous hypertension and venous reflux can cause excess lymph production and overwhelm lymphatic circulation.
The venous system and lymphatic circulation rely on the same passive contractions to clear fluid from limbs. There are many documented abnormalities of lymphatic flow in lipedema: Dilated lymphatics , impaired lymph flow and progression to secondary lymphedema. This increase lymph produced by venous insufficiency or back flow in turn drive inflammation and worsen lipedema .
- Vein insufficiency can add to or worsen symptoms of lipedema disease (also known as Lipoedema, Lipodema, and Lipodem)
- Significant vein problems mean saphenous vein insufficiency not spider veins
- It is important to treat significant vein problems prior to Lipedema lipo
Dr. Wright explains vein problems in women with Lipedema.
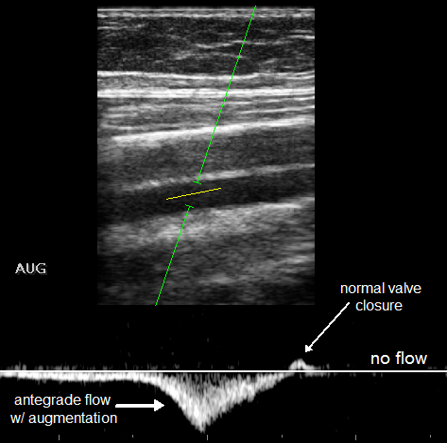
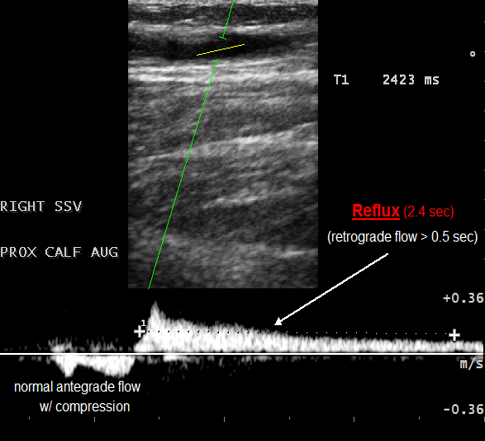
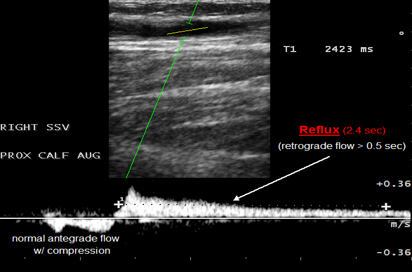
Venous Reflux Ultrasound (VRU)VRU: Identifies Venous Reflux as Reversed Flow
|
||||||
|
Credit: American College of Phlebology (ACP) Venous Reflux Ultrasound (VRU)
|
||||||
Lipedema with Vein Changes
|
||||||
|
Credit: American College of Phlebology (ACP) Consequences of Venous Hypertension
|
||||||
In Conclusion
|
Other References
Sandofer 2 High Volume Liposuction in Tumescence Anesthesia in Lipedema Patients: A Retrospective Analysis
Gould Uncovering Lymphatic Transport Abnormalities in Patients with Primary Lipedema
Does tumescent liposuction damage the lymph vessels in lipoedema patients?
Crescenzi R, Marton A, Donahue PMC, Tissue sodium content is elevated in the skin and subcutaneous adipose tissue in women with lipedema: Obesity (Silver Spring), 2018; 26(2); 310-17.
Hoffmann JN, Fertmann JP, Baumeister RG, Putz R, Frick A. Tumescent and dry liposuction of lower extremities: differences in lymph vessel injury. Plast Reconstr Surg. 2004 Feb;113(2):718-24; discussion 725-6. doi: 10.1097/01.PRS.0000101506.84361.C9. PMID: 14758241.
Iker E, Mayfield CK, Gould DJ, Patel KM, Characterizing lower extremity lymphedema and lipedema with cutaneous ultrasonography and an objective computer-assisted measurement of dermal echogenicity: Lymphat Res Biol, 2019; 7(10); 525-30.
Peprah K, MacDougall D: Liposuction for the treatment of lipedema: A review of clinical effectiveness and guidelines, 2019, Ottawa (ON), Canadian Agency for Drugs and Technologies in Health.
Rasmussen 2022.[Lymphatic function and anatomy in early stages of lipedema]
It also well reported that higher stages of lipedema are associated with impaired lymphatic functioning. ,7–9].
The Diagnosis and Treatment of Peripheral Lymphedema: 2016 Consensus Document of the International Society of Lymphology: Lymphology, 2016; 49(4); 170-84.
Wright TF, Herbst KL. A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema. Am J Case Rep. 2022 Jul 11;23:e935016. doi: 10.12659/AJCR.935016. PMID: 35811389; PMCID: PMC9284075.