Patients are commonly confused about the difference between lymphedema and lipedema. Both conditions can cause limb swelling but have different causes and treatments. Below we explain the difference between lymphedema and lipedema and how to identify and treat each disease.
Understanding Lymphedema and Lipedema
Lymphedema and lipedema are both conditions that cause swelling in the limbs. However, they have different causes and symptoms. Lymphedema is caused by damage to the lymphatic system, which is responsible for draining excess fluid from the body. Lipedema, conversely, is caused by inflammation, fibrosis, and expansion of the subcutaneous adipose tissue.
Most Lymphedema can be caused by surgery, radiation therapy, or infection. For example, a patient who has had breast cancer surgery may develop lymphedema in the arm on the same side as the surgery. In rare instances, Lymphedema may be congenital or caused by a genetic disorder. Lipedema is a genetic condition that primarily affects women. It generally appears after hormonal changes. It often develops during puberty, pregnancy, or menopause.
What Causes Lymphedema and Lipedema?
Lymphedema is caused by damage to the lymphatic system, which can occur due to surgery, radiation therapy, or infection. When the lymphatic system is damaged, it cannot drain excess fluid from the body, which leads to swelling in the affected area.
Lipedema is a genetic condition caused by inflammation, fibrosis, and hypertrophy of subcutaneous adipose tissue in the legs, thighs, and buttocks. The exact cause of lipedema is unknown, but it is thought to be related to hormonal changes that occur during puberty, pregnancy, or menopause, may be genetic, and often can be seen in family history.
Lymphedema vs. Lipedema: Key Differences
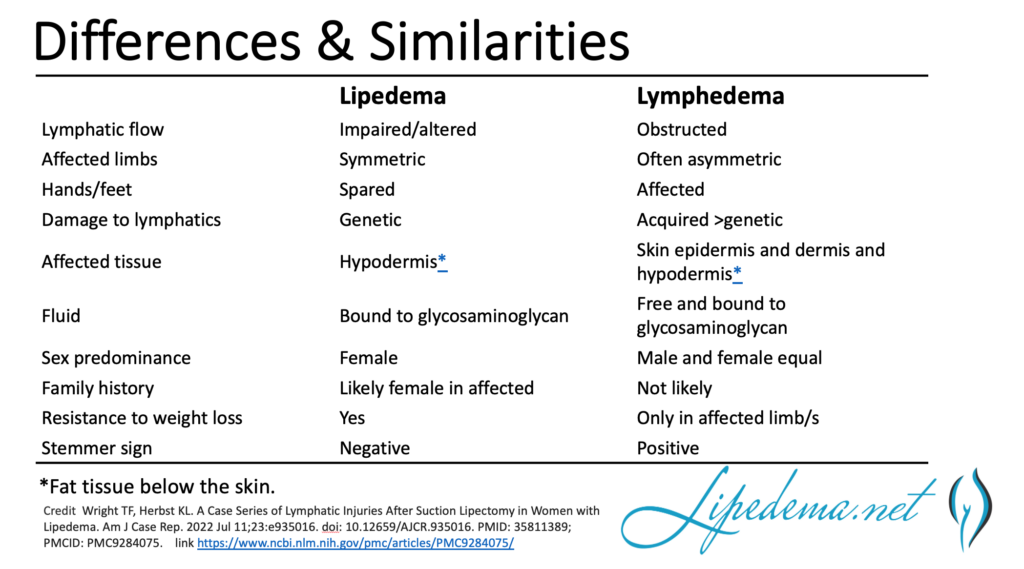
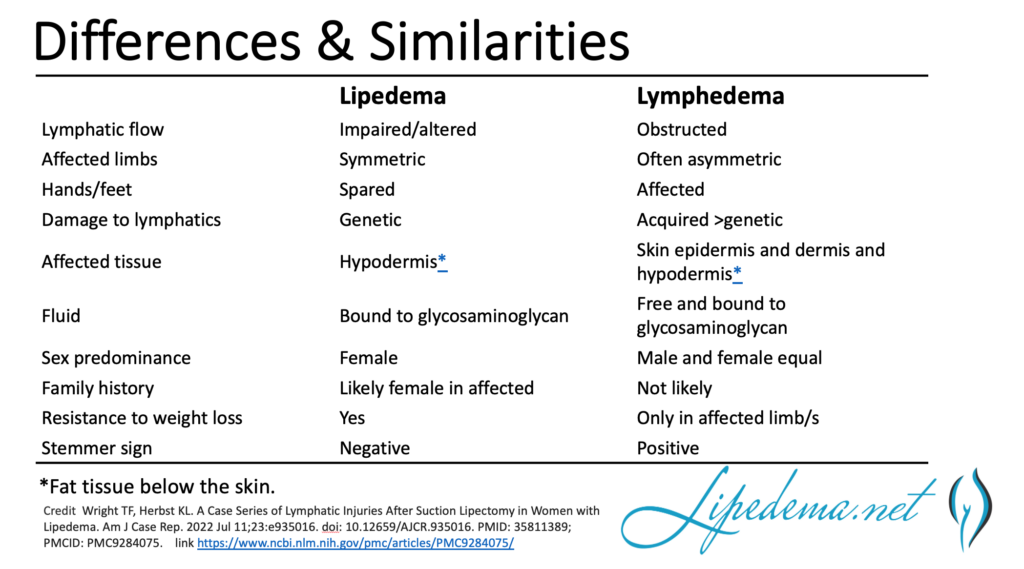
Lymphedema is asymmetric. Usually, one limb is affected, or one limb is more affected than the other. Lipedema is symmetric leg and arms are affected equally. Lipedema always spares the hands and feet initially. Lipedema almost exclusively affects women. Lymphedema affects men and women but still affects women a bit more.
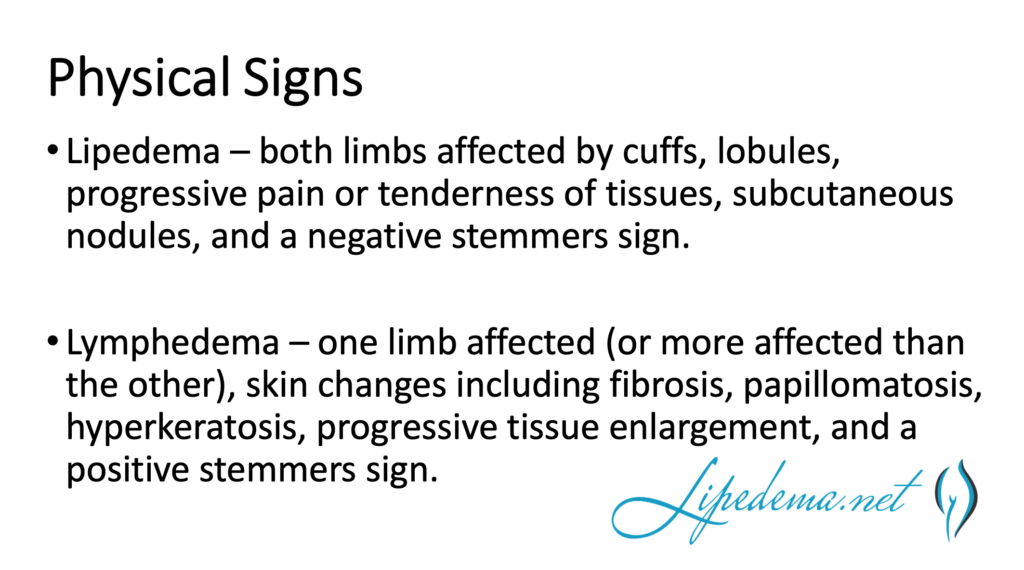
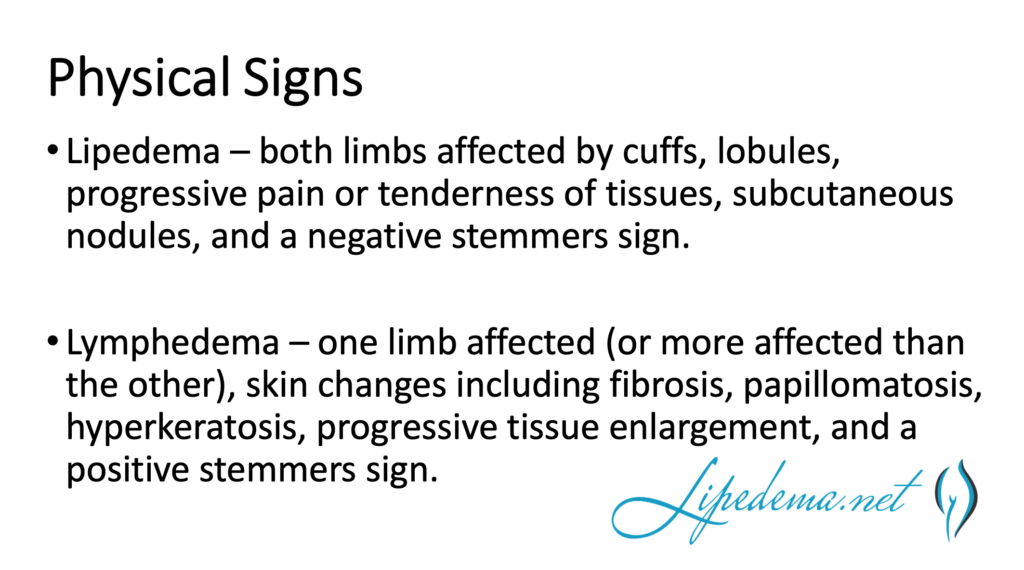
The symptoms of lymphedema include swelling in the affected area, a feeling of heaviness or tightness in the limb, and aching or discomfort. In severe cases, the skin may become thickened and hard. Conversely, lipedema typically causes symmetrical swelling in the legs, thighs, and buttocks. The skin may be tender or painful to the touch, but it is usually not thickened or stiff.
Symptoms of Lymphedema and Lipedema
The symptoms of lymphedema and lipedema can be similar, but there are some differences. Lymphedema typically causes swelling in the affected area, a feeling of heaviness or tightness in the limb, and aching or discomfort. The skin may become thickened and hard in severe cases. Conversely, lipedema typically causes symmetrical swelling in the legs, thighs, and buttocks. The skin may be tender or painful to the touch, but it is usually not thickened or hard.
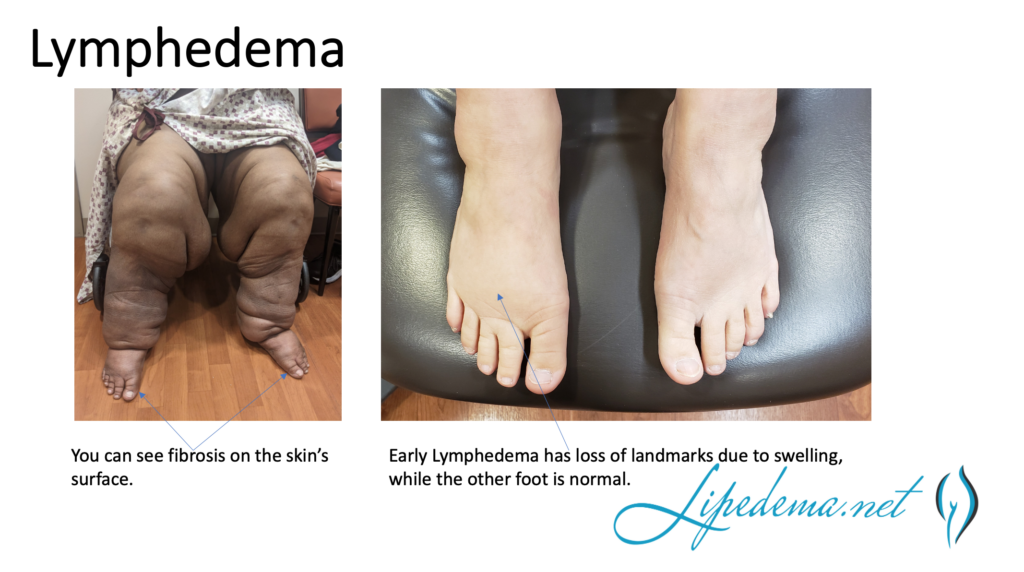
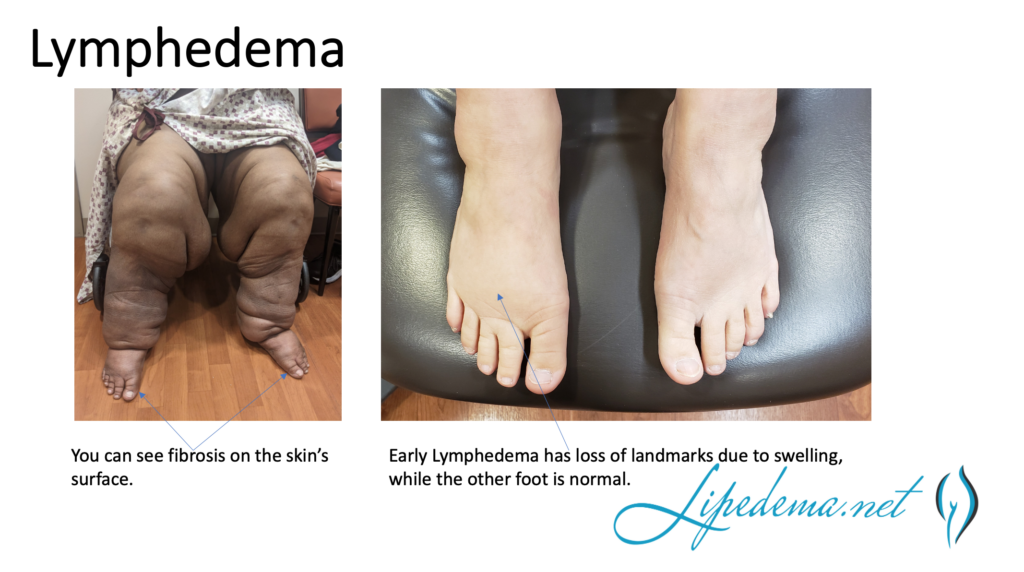
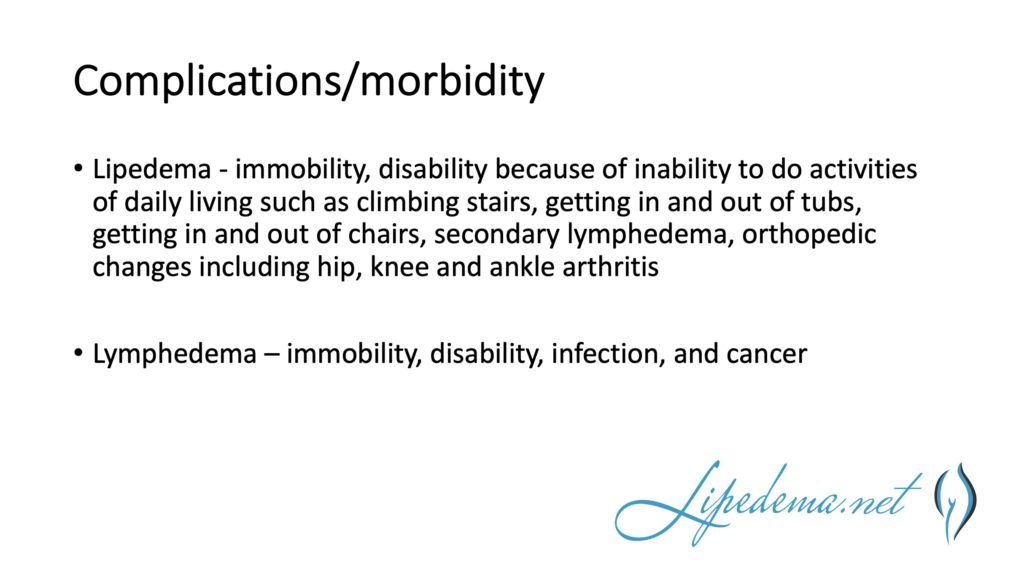
Both conditions can cause difficulty with movement and mobility. Patients with lymphedema may have trouble with activities that involve the affected limb, such as lifting or carrying objects. Patients with lipedema may have difficulty walking or standing for long periods. Lymphedema increases the risk of infection and cancer in the affected limbs. Over time, this leads to progressive enlargement and fibrosis of the stem.


Diagnosis and Treatment of Lymphedema and Lipedema
Diagnosing lymphedema and lipedema is mainly clinical. Both involve a physical examination and medical history. The diagnosis of Lymphedema may be helped through imaging tests, such as an ultrasound or MRI, to check for blockages in the lymphatic system. However, the sensitivity of the imaging tests do not easily pick up early Lymphedema. Lipedema is typically diagnosed through a physical exam; however, ultrasound and ruling out other causes are required.
Non-surgical treatment for lymphedema and lipedema typically involves lifestyle changes, compression therapy, and exercise. Lifestyle changes may include weight loss, avoiding tight clothing or jewelry, and avoiding extreme temperatures. Compression therapy involves wearing compression garments, such as socks or sleeves, to help reduce swelling. Exercises like walking or swimming can also help improve lymphatic flow and reduce swelling.
Lifestyle Changes for Managing Lymphedema and Lipedema
Lifestyle changes can help manage lymphedema and lipedema. Patients with lymphedema should avoid tight clothing or jewelry that may restrict lymphatic flow. They should also avoid extreme temperatures, such as hot tubs or saunas, which can cause swelling. Weight loss can also help reduce the severity of lymphedema symptoms.
Patients with lipedema should maintain a healthy weight and avoid diets high in processed carbohydrates and sugar. They should try to be as active as possible and avoid standing or sitting for long periods, as this can worsen swelling. Wearing compression garments can also help reduce swelling and improve lymphatic flow.
Lipedema Reduction Surgery Overview
To be clear, lipedema reduction surgery cannot cure lipedema – it can only provide fat reduction and symptom relief and slow the progression of this disease. Liposuction is not an appropriate option for everyone with lipedema, and like any surgical procedure, there are risks. Lipedema reduction surgery is more than liposuction; it involves maximum debulking of the tissue – not just fat cells and tissue but also fibrous tissue. Due to already having a delicate lymphatic system, Lipedema reduction surgery requires additional prep and care to ensure no additional impairment to an already fragile lymphatic system. Ultimately, it’s important to understand that lipedema reduction surgery is not a silver bullet for curing lipedema. Post-surgery, lifestyle changes are required to maintain the results seen from surgery.
Examples of post-liposuction lifestyle changes:
- Strict adherence to a low refined-carbohydrate diet.
- Wearing medical-grade compression garments.
- Weight management through a health diet and active lifestyle.
- Regular physical activity through low-impact weight training, swimming and yoga.
Although lipedema reduction surgery is generally safe in healthy individuals, risks such as infection, bleeding, and trauma to the area may occur. Post-operative swelling in the limbs after surgery, which occurs with any lipedema lipo procedure, is more prolonged in individuals with lipedema. The swelling typically worsens for a few months before it gets better, and the full benefit may not be realized for six months to a year. However, overall, most patients with lipedema experience significant improvement in many or all of their symptoms, with varying individual results.
Numerous care guidelines, including the ones published in the US, Germany, the UK, and Canada, recommend lipedema reduction surgery for women with lipedema who have symptoms that are not relieved with conservative measures.
Although some people with lipedema limited to only one specific area may need one procedure, most people undergo multiple lipedema lipo procedures to address all the different areas affected by lipedema. The multiple liposuction procedures must be staged or separated to be done safely. The timing of the procedures depends on multiple factors, including the clinical stage of lipedema in the patient, the amount of fat being removed, the patient’s health and mobility, and other logistical factors.
Benefits of Lipedema Reduction Surgery
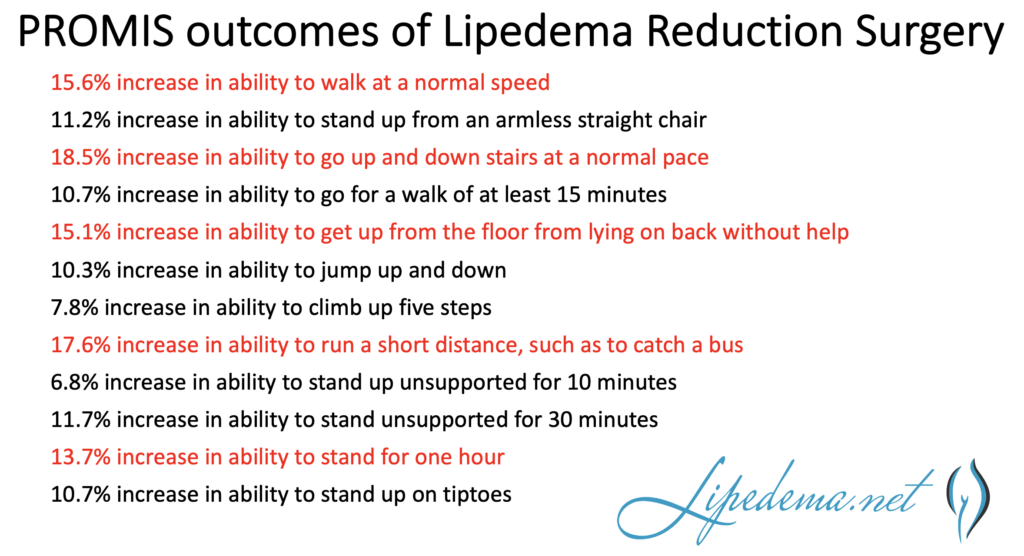
Lipedema reduction surgery has been shown to decrease pain, improve quality of life, decrease the need for compression, and slow or reverse the progression of lipedema. New research shows that it also improves mobility and knee mechanics. Using the NIH Outcomes Tool, PROMIS, these statistically significant changes were demonstrated after lipedema reduction surgery.
Preventing Lymphedema and Lipedema Complications
Complications from lymphedema and lipedema can be prevented through proper treatment and management. Patients with lymphedema should avoid injuries to the affected limb, such as cuts or burns, which can lead to infection. They should also prevent blood draws or injections on the affected limb. Patients with lipedema should maintain a healthy weight and avoid wearing tight clothing, which can worsen swelling.
Dealing with the Emotional Impact of Lymphedema and Lipedema
Lymphedema and lipedema can have a significant emotional impact on patients. Patients may experience depression, anxiety, and a decreased quality of life. Counseling and support groups can help patients cope with the emotional impact of these conditions.
Support Groups and Resources for Lymphedema and Lipedema
Many support groups and resources are available for patients with lymphedema and lipedema. The Lymphatic Education & Research Network (LE&RN) and the National Lymphedema Network (NLN) are two organizations that provide resources and support for patients with lymphedema. The Lipedema Foundation is an organization that provides resources and support for patients with lipedema.
Conclusion: Living Well with Lymphedema and Lipedema
Lymphedema and lipedestama are two conditions that can cause swelling in the limbs. While they have different causes and symptoms, both conditions can be managed through proper treatment and lifestyle changes. Patients with lymphedema and lipedema should work with their healthcare provider to develop the best treatment plan. With proper management, patients can live well with lymphedema and lipedema.







