Lipedema is a condition that affects the distribution of fat in the body, primarily in the lower extremities. Lipedema is a progressive disorder, and a significant portion of women with Lipedema progress to secondary Lymphedema. Understanding the relationship between lymphatics and Lipedema is crucial in understanding how lipedema develops and progresses.
It’s characterized as a “progressive disorder,” meaning the tissues enlarge and that over time, there is a progressive deterioration of lymphatics. When looking at extracellular water content, which is a marker of lymphatic function, the higher of the stage of lipedema, the greater the proportion of women with lipedema who also had increased amounts of extracellular water consistent with lymphatic impairment. To put it simply, research is finding that lipedema and lymphatic impairment are related.
The lymphatic system is responsible for maintaining the balance of fluids in the body and helps remove waste products and toxins through a network of vessels and lymph nodes. When the lymphatics are not functioning properly, fluid can build up, leading to swelling and inflammation. In the case of lipedema, there is often impaired lymphatic drainage. This means that the excess fat cells can put pressure on the lymphatic vessels, causing them to become compressed and less effective at removing fluid.
Lymphatic impairment changes the whole biology of the affected tissues. In the legs and arms affected by lymphatic impairment, the biology of the fat cells and other connective tissues are changed. The cells and tissues are always creating proteins, and storing and releasing fats as part of a normal, healthy bodily function. As part of this system, lymphatics are responsible for removing fatty acids, cellular debris, and large protein as they work to clean up, remodel, and maintain the structure and function of the tissues.
When we have lymphatic impairment in our tissues, the biology of these cells completely change. There is an increased deposit of fibrous tissues, and the fat cells increase in number and size. These cells are no longer doing their job properly, and we don’t have equilibrium; the balance shifts towards tissue growth and fibrosis, leading to swelling and limb enlargement that is typical of lipedema and oftentimes, secondary lymphedema.
As the tissue enlarges in women with lipedema, we start to see more telltale signs of the disease, such as lobules and cuffs at the ankles and wrists. As these lobules and cuffs enlarge, the skin droops and hangs off the body. This, in turn, causes localized swelling and further disrupts the lymphatic flow, leading to a vicious cycle. The tissue enlargement caused by impaired lymphatics further disrupts lymphatic function. Read more about Lipedema Lobules and Nodules here.
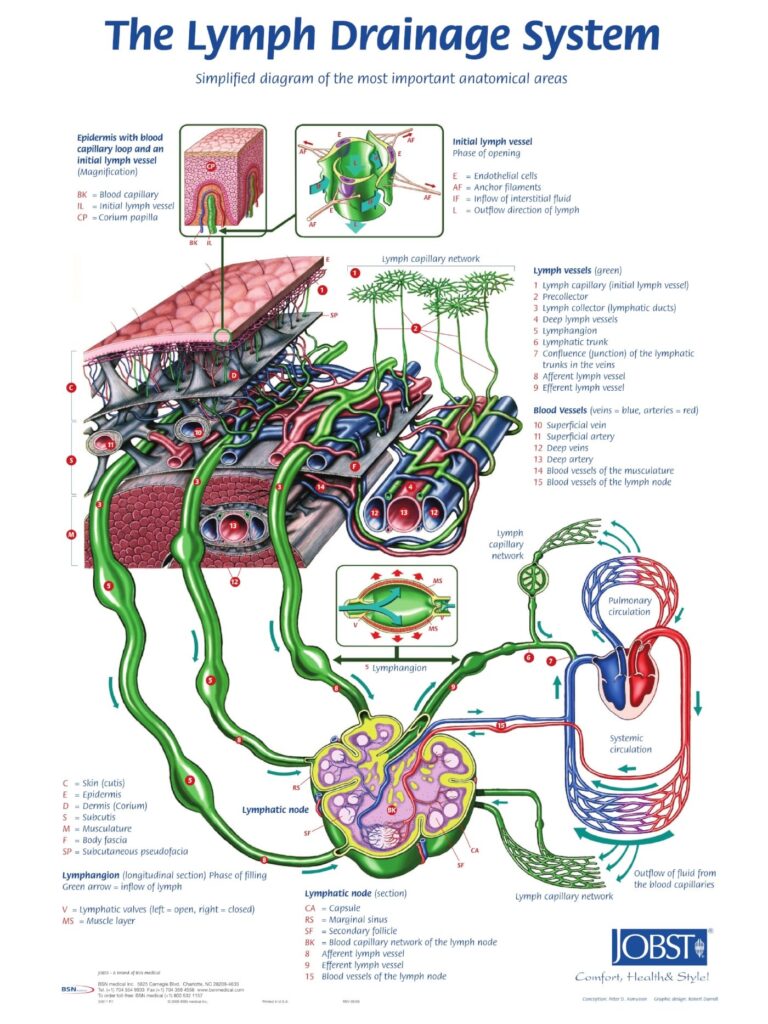
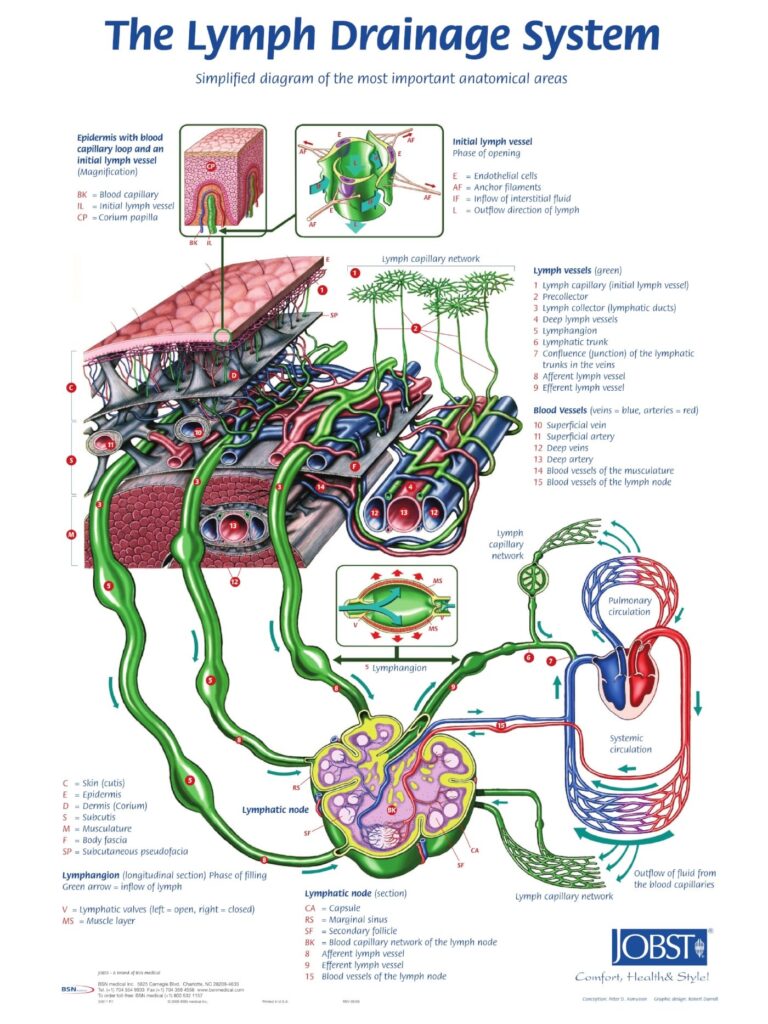
Let’s break down in greater detail the lymphatic system and its role in maintaining healthy tissue. The lymphatic system is a network of vessels and organs that help remove waste, toxins, and excess fluid from our tissues. It plays a vital role in maintaining a healthy immune system and fluid balance. The lymphatics and veins are closely interconnected. Lymphatic vessels are responsible for carrying lymphatic fluid, which contains immune cells and waste products, while veins are responsible for carrying blood back to the heart. Both systems work together to ensure proper circulation throughout the body. For those struggling with vein health and lipedema, we’ve outlined the causes and treatments.
Dr. Wright and Jen discuss Lymphatics and Lipedema.
How Lymphatics Work
Like lipedema, lymphatic circulation has been neglected and largely ignored until recently. For example, the arterial-venous circulation system is nearly common knowledge. Most people learn about it in school and we have a clear understanding on how works: The heart pumps the blood through the arteries, which take the oxygenated blood to the tissues, and then the venous system returns the deoxygenated blood back to the heart. This is a closed system. On the other hand, the lymphatics are an open system that is seldom talked about in school. In this system, we aren’t focused on blood flow, but instead on lymph fluid which is a clearish and sometimes yellow-tinted proteinaceous fluid. Lymph is created in the tissues, from the fluid that leaks out at the capillary-level and contains large proteins, cells, and cellular debris.
The basic unit near the start of the lymphatic system is the lymphangion, which is a smooth muscle-lined vessel that propels the fluid toward our lymph nodes. The Lymphatic System is self-propelling. There are valves at the beginning of the lymphatic system that ensure that the fluid that enters will not be able to flow out and leave. Along the way, there are additional valves much like the venous system, which ensure one-way flow. And also like the venous system, the fluid is further aided and propelled forward by the contraction of muscles.
The lymphatics start at a lymphatic capillary-level, which combines into lymphatic collecting ducts. These collecting ducts further collect together and become lymphatic trunks and enter lymph nodes. In the lymph nodes, the lymph is filtered and lymphocytes scour and search for foreign cells and proteins that should be removed from the body. After the lymph is filtered through the lymph nodes, its sent toward the center of the body. Eventually, it ends up in the thoracic duct, where it returns to the venous circulation, just in front of the heart.
Dr. Wright and Jen discuss Lymphatics and Lipedema.
Normal vs. Impaired Lymph Flow in Lipedema
There are well-documented changes in the lymphatics of women with lipedema. Rasmusen and others have reported on dilated lymphatics in lipedema. Many other authors have reported on impairments of lymphatics in lipedema (Gould, Van De Pas). The following is a near-infrared direct lymphography image from research conducted by Dr. Wright. In it, you can see the difference between normal and Lipedema tissue found in the foot and ankle. In this image, there is normal, linear lymphatic flow in the lipedema patient’s foot, which changes to dilated, tortuous lymphatic flow as the lymph flows in the area of the ankle cuff caused by lipedema.
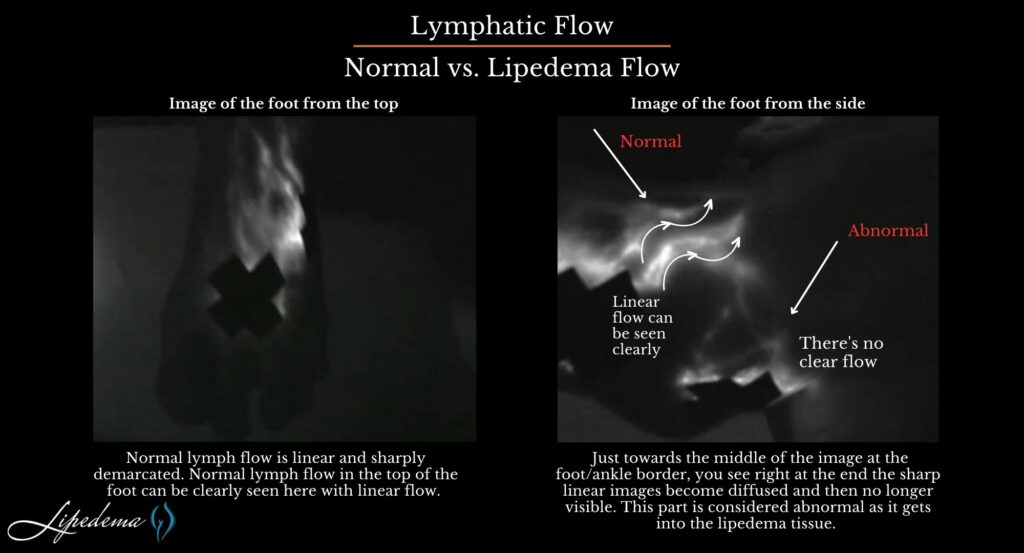
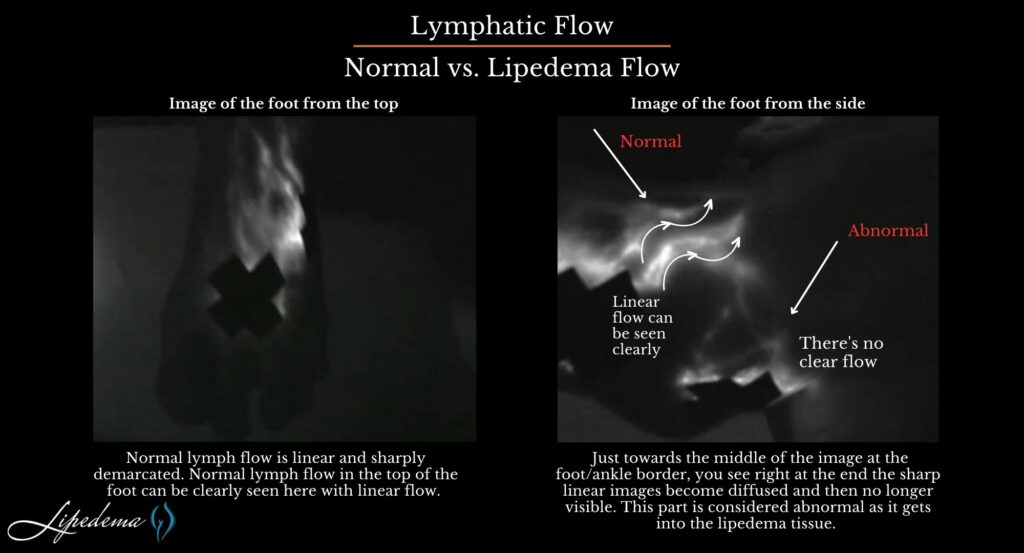
The lymphatics are dilated and tortuous, and as lymph moves into lipedema tissue, it becomes less demarcated and linear. Normal lymph flow is linear and sharply demarcated. Just towards the middle of the image at the foot/ankle border, you see right at the end the sharp linear images become diffused and then no longer visible. This part is considered abnormal as it gets into the lipedema tissue.
The above images show that there are dilated lymphatics in lipedema and that there are reports that liposuction can injure lymphatics in lipedema. Now that we know the relationship between the two, it’s imperative that compression and other lymphatic flow-promoting treatments are included in the comprehensive treatment of lipedema. We’ll explain these practices below, and you can read more about the Lipedema Standard of Care here.
How is lymph flow different in Lipedema?


Lipedema vs. Lymphedema & Lymphatics
It is estimated that over 60% of individuals with lipedema may also experience some degree of lymphatic dysfunction. Lymphedema and lipedema are both conditions that cause swelling in the limbs. However, they have different causes and symptoms. Lymphedema is caused by damage to the lymphatic system, which is responsible for draining excess fluid from the body. Lipedema, conversely, is caused by inflammation, fibrosis, and expansion of the subcutaneous adipose tissue.
So, what does this mean for individuals with lipedema? Since impaired lymphatic drainage plays a significant role in the development and progression of lipedema, therapies that focus on improving lymphatic function can be beneficial. It’s important to note that while lymphedema is frequently associated with lipedema, not all individuals with lipedema will develop lymphedema. Read more about the differences and similarities between Lymphedema and Lipedema here.
Treating Impaired Lymphatics
Before any type of surgery can be discussed, it’s important to ensure the non-surgical treatments are followed and the lymphatic function is optimized. Examples of these practices are below, and you can also read an in-depth study about an approach to the best surgical outcomes by first addressing the inflammation in the tissues with dietary and lymphatic treatment. Read Dr. Amato’s research here.
Compression Therapy for Lymphatic Flow
Compression garments, such as compression stockings or sleeves, can also be useful in providing external support to the lymphatic vessels and promoting fluid movement. In addition to these therapies, maintaining a healthy lifestyle is key. Regular exercise, a balanced diet, and weight management can help reduce the burden on the lymphatics and improve overall lymphatic function. In conclusion, lymphatics and lipedema are closely intertwined. The impaired lymphatic drainage seen in lipedema can contribute to chronic swelling and inflammation, further complicating the condition. Understanding this relationship is vital for effective treatment and management of lipedema, with therapies aimed at improving lymphatic function playing a significant role. Read more about compression therapy here.
Exercise for Lymphatic Flow
Exercising can help to activate the lymphatic drainage system in a patient’s limbs through the foot and calf muscle pump. Workouts that aren’t too strenuous help to move the excess fluids out of affected limbs, as well as reducing additional fat buildup. Good lymph flow depends on proper joint and muscle activity. This is especially true if the lymphatic system is compromised. Individuals suffering from lipedema can receive a great benefit when engaging in diaphragmatic breathing exercises. These exercises are especially beneficial when they are combined together with other parts of a decongestive regimen.
Because fat disorders and lymphedema can often feed into one another, exercise is a great option to help combat both. With its dual purpose of clearing out excess lymph fluid and burning fat, exercise offers exactly what patients need to deal with these disorders. Learn more about the best types of exercise for lymphatic flow here.
The Rare Adipose Disorder Diet (AKA RAD Diet)
Dr. Wright recommends following a Rare Adipose Disorder (RAD) diet, a modification to a standard Mediterranean diet that helps you maintain a low glycemic index to limit the number of occurrences and levels your blood sugar spikes through the day. In order to do this, it is recommended that you avoid any refined or processed starches and sugars. These are usually found in pasta, rice, bread, corn, and potatoes. Avoiding processed food – especially processed carbohydrates – will keep your insulin levels low and provide you the best chance of limiting inflammation. Read more about healthy eating and lymphatic flow here.
Manual Lymph Drainage and Experience Lymphatic Drainage Benefits
Manual lymph drainage is just one component of complete decongestive therapy (CDC). In addition to MLD, complete decongestive therapy includes compression, exercise, and skincare. These therapeutic components, when performed together, can ultimately relieve the symptoms of lipedema, which can often be painful.
When you stimulate the lymphatic system, you will feel the effects of several lymphatic drainage benefits:
Increase the capacity of the lymphatic system, which will then let it process more fluid than normal.:
- Increase the flow through the lymph nodes, which will, in turn, allow the system to filter out waste, dead cells, excess proteins, and toxins.
- The production of lymphocytes will increase to heighten the body’s ability to fight infections.
Other lymphatic drainage massage benefits include reduction of pain and swelling and an increase of venous return and circulation. Learn more about this technique here.
Dry Brushing Technique and Benefits of Dry Brushing
In addition to several other procedures and treatments for lipedema, pump therapy, whole-body vibration, and dry brush massage can also increase the circulation of lymph fluids and relieve the sometimes painful symptoms. Learn more about whole-body vibration and dry brush massage below!
Because the lymphatic system lies just below the skin’s surface, dry brushing has been considered an effective treatment for lipedema. The benefits of dry brushing have been shown to provide :
- Help move the venous blood.
- Stimulate the lymph system.
- Strengthen the immune system.
- Improve surface circulation.
- Exfoliate the skin.
- Improve the look of the skin to produce a healthier feel.
The dry brushing technique is performed with a brush, either with a handle or a strap, that has soft bristles. As the name says, the brush is used dry and without water. You will not get the same results if the skin or brush is wet. With long, gentle, firm strokes, go over your entire body (except the face). The strokes should move the skin toward the heart and neck. Start with the feet and brush upward to the knees, groin, abdomen, and chest. Then brush the hands and arms to the armpits. Read more about dry brushing and lymphatic flow here.
What Kind of Surgery is Safe for Lymphatics in Lipedema Patients?
Lipedema reduction surgery is a spin-off of liposuction focused on the reduction of lipedema tissues, including fibrous tissue, fat, and extracellular contents. It is possible for lymphatics to be injured by a suction cannula during lipedema reduction surgery and/or cosmetic liposuction. Some argue whether this is possible, but studies show it can, and unfortunately, may happen for some. In a recent study published in the American Journal of Case Reports, According to a study by Wright and Herbst confirms that this can occur. So, it is essential if you have lipedema, or suspect you may have lipedema that you get a proper diagnosis and work closely with skilled surgeons well-versed in lipedema, lymphatics and lymphedema for the best possible outcomes and treatment plan before you proceed with any type of liposuction.
During liposuction some temporary interruption to the lymphatic vessels is unavoidable. In the vast majority of patients, the lymphatics return to normal in the postoperative period, especially for patients with underlying normal lymphatic function [ Read patients without lymphedema or lipedema]. Suction lipectomy with small blunt cannulas and surgical techniques that focus on avoiding lymphatic damage has been reported to halt lipedema progression. [Sandofer 1, 2] A modification of suction lipectomy can result in alleviating or at least improving the swelling, leg heaviness and fatigue, the need for limb compression, and the need for lymphatic massage in women with lipedema. In patients with an impaired lymphatic function such as chronic lymphedema (or lipedema), careful suction lipectomy using techniques to avoid lymphatic injury can result in improved lymphatic function and a decreased rate of secondary infection or cellulitis in the affected limbs. [Gould . Van de Pas 3,4,]. Once you understand that lymphatics are impaired in lipedema and you understand that lymphatic injury can occur, the natural question arises – How can we protect the lympathic system in lipedema surgery? Read more about surgical treatments for lipedema here.
What Are Measures That May Protect Lymphatics in Lipedema Liposuction?
The short answer is this issue is hard to study as it is not possible to examine on live patients. There is one study by Hoffman which showed a longitudinal cannula technique and tumescent solution caused less injury to the lymphatics post-mortem. There is some evidence that the preoperative mapping of venous and lymphatic structures can lower the risk of lymphatic injury. While there is clear evidence lymphatic injury can occur, there is no definitive proof of what surgical techniques can prevent lymphatic injury from liposuction or surgery for lipedema. Lymphatic injury complications are poorly recognized after suction lipectomy surgeries and therefore are less likely to be reported in the literature for both lymphedema and lipedema.
Protective measures to lessen the risk of lymphatic injury include:
- Map out the important vein and lymphatic structures
- Generous tumescent fluid (A mix of saline, Lidocaine, and a vasoconstrictor—epinephrine—which is injected before liposuction and facilitates fat removal, provides anesthesia, decreases swelling, bleeding, bruising, and improves post-op recovery)
- Longitudinal cannula technique near lymphatic structures to avoid injury
- Multiple positions to allow optimal orientation of the cannulas
- Small blunt cannulas versus large incisions
Possible Side Effects From Lymphatic Injury After Liposuction
Skin Lymphostatic Fibrosis:
This is a widespread side effect in patients with lymphedema, where the skin hardens over time. In the early stages of lymphedema, swelling is soft to the touch. However, over time, the swelling hardens the skin due to the development of connective tissue fibers underneath the skin of the affected areas.
-
Papillomatosis:
The growth of numerous papillomas, more commonly referred to as warts.
-
Dermal Sclerosis:
Hardening and tightening of the skin and connective tissues.
-
Leg Swelling:
Ironically, leg swelling is one of the most common symptoms of lipedema and prompts patients to seek treatment. Post-lymph-sparing liposuction for lipedema, lymphatic injury after liposuction can lead back to leg swelling.
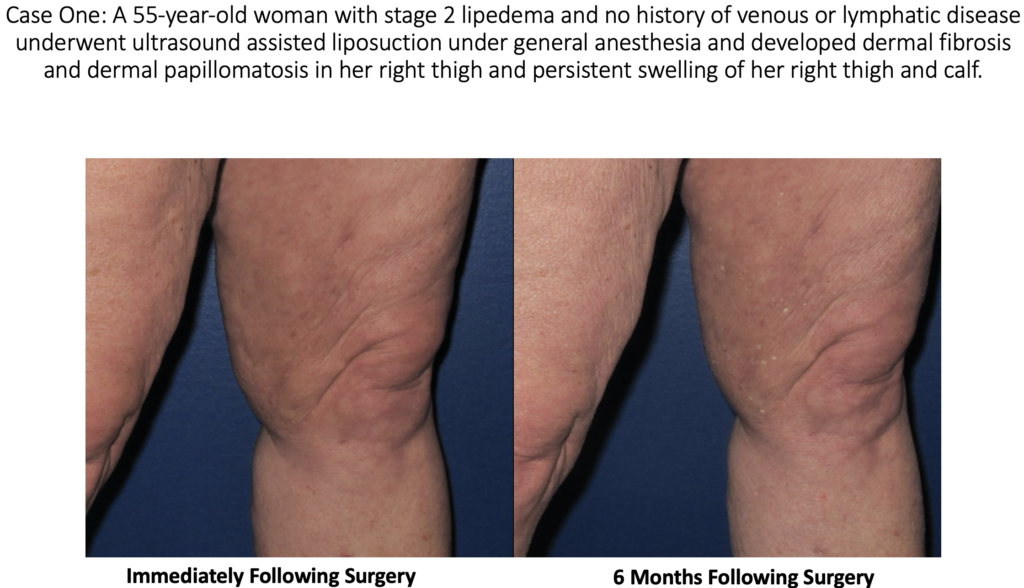
At this time, most experts believe that suction lipectomy with ultrasound, power, or water assistance techniques, in the proper hands, are safe and effective treatments for lipedema, as long as the surgeon performing the liposuction has skill and experience to perform a lymph-sparing technique. When suction lipectomy is performed properly, it improves symptoms, lymphatic flow, and skin health. Studies have shown that lipedema is often associated with lymphatic impairment. Studies have also shown that lymphatic function is not changed or improved with careful liposuction that uses surgical techniques and technologies that protect or minimize lymphatic injury after liposuction. We do know that traditional liposuction, without special care of the lymphatics or proper tumescent technique, can cause lymphatic damage and possibly worsen lipedema symptoms.
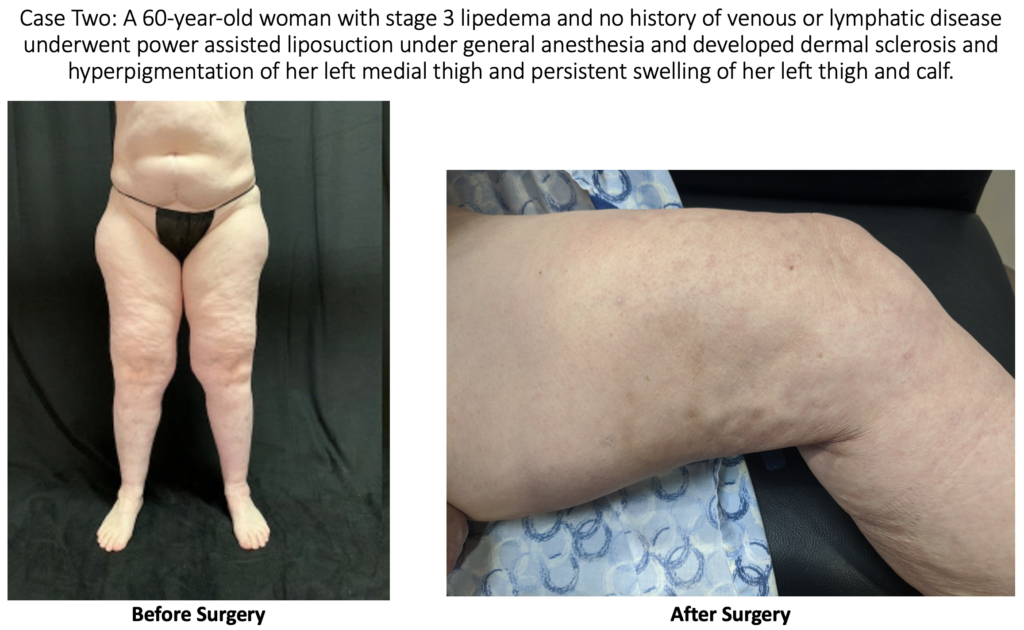
The skin changes experienced by the above patients were not present prior to the surgery. The changes seen in these patients are consistent with stage 2 or stage 3 lymphedema. We are left to conclude that the lymphedema changes in the skin were most likely the result of surgical trauma during suction lipectomy. Doctors A. Frick, C.C. Campisi, and others have shown that there are surgical techniques that can limit the risk of lymphatic injury after liposuction. [1,2] These case reports show the importance of choosing a surgeon that will take every precaution to not injure lymphatics.








