

Lipedema and cellulitis are two conditions that often coexist, causing discomfort and distress to those affected. Understanding the relationship between these two conditions and implementing prevention strategies is crucial for optimal management. Lipedema is a chronic disorder characterized by an abnormal accumulation of fat in the legs and sometimes the arms, causing pain, swelling, and tenderness.
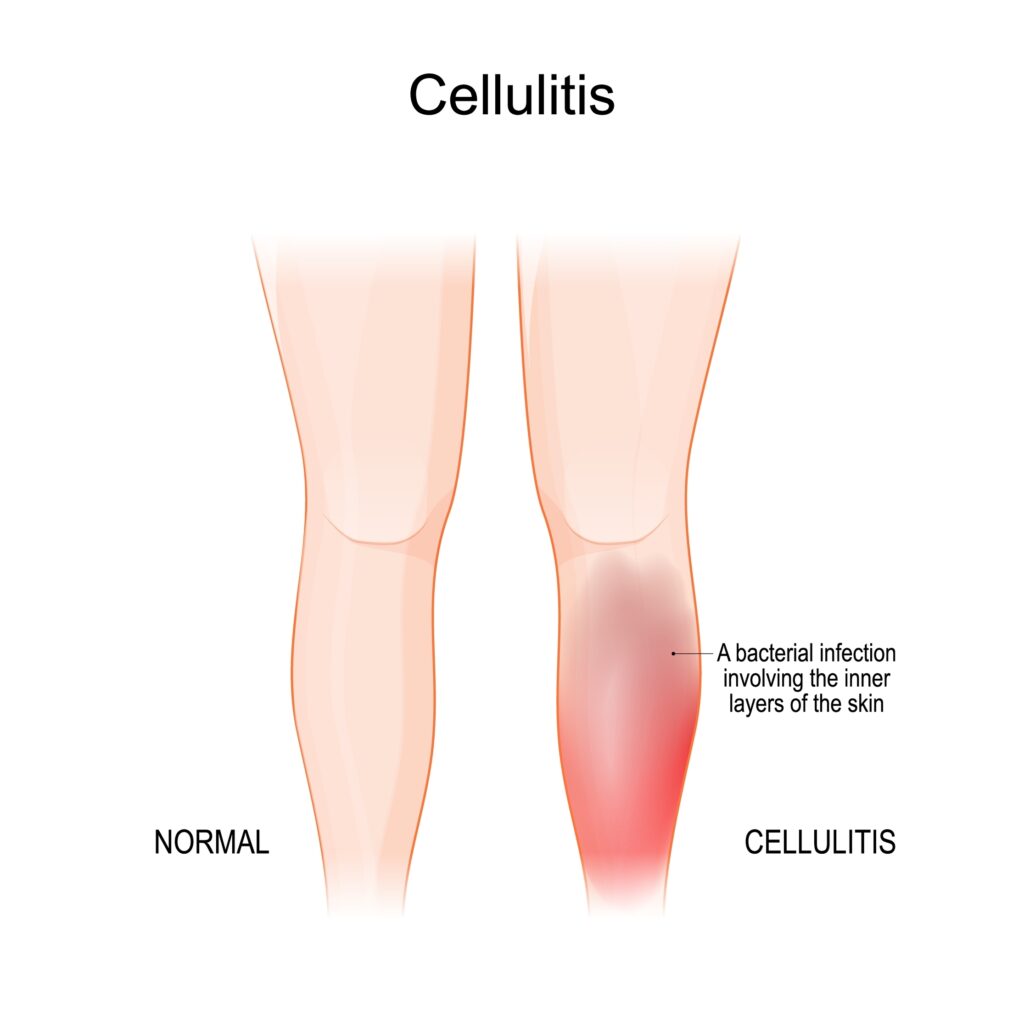
On the other hand, cellulitis is a bacterial skin infection that can occur as a complication of lipedema due to impaired lymphatic drainage and weakened immune response. It presents with redness, swelling, and warmth in the affected area. By addressing both lipedema and cellulitis simultaneously, individuals can experience relief from symptoms and prevent recurrent infections.
Prevention strategies for lipedema-related cellulitis may include maintaining good hygiene practices, promptly treating skin abrasions or wounds, wearing compression garments, and seeking early medical intervention to address lipedema symptoms. In this article, we will explore the relationship between lipedema and cellulitis, exploring effective prevention strategies and highlighting treatment options available in St. Louis. By understanding and managing these conditions, individuals can enhance their quality of life and overall well-being.
What is Lipedema?
Lipedema is a fat tissue disease, mainly affecting women, that causes an enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Medical professionals often misdiagnose and dismiss lipedema as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
Women suffering from Lipedema often report the disease a sociated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.
Recognizing the Symptoms of Lipedema
Early detection of lipedema is crucial for timely intervention and management. Several signs and symptoms can indicate the presence of lipedema. Initially, these symptoms may be subtle, but they become more evident as the condition progresses. Common indicators of lipedema include symmetrical swelling in the legs, unexplained bruising, heaviness and tenderness in the affected limbs, and a lower body size disproportionate to the upper body. In advanced stages, the skin may develop pearl-sized lumps, which can grow larger and resemble walnuts or plums.
The Challenge of Diagnosis and Treatment
Diagnosing lipedema can be challenging due to a lack of awareness among healthcare professionals. Many patients are misdiagnosed with obesity, leading to delayed treatment and unnecessary fat-shaming. To ensure accurate diagnosis and appropriate treatment, it is crucial to seek the expertise of a specialist familiar with lipedema. Early diagnosis allows for timely intervention and improves the chances of successful treatment outcomes.
Treatment Options for Lipedema
Effective treatment strategies are available for individuals with lipedema. Lymphatic support, such as complete decongestive therapy, can help manage the symptoms of lipedema. Additionally, specialized suction lipectomy, a surgical procedure, can remove diseased lipedema fat while preserving lymphatic channels. This surgical intervention not only enhances the patient’s quality of life but also improves their self-confidence by restoring a more proportionate appearance to the lower body.
Understanding Cellulitis: Causes and Symptoms
Cellulitis is a skin infection caused by bacteria that infiltrate the deep layers of the skin through breaks such as cuts or scratches. Common symptoms of cellulitis include redness, swelling, pain, tenderness, and the development of blisters. It is essential to note that cellulitis is not a direct symptom of lipedema but can arise due to the underlying condition.
The Link Between Lipedema and Cellulitis
While cellulitis is not a direct symptom of lipedema, individuals with lipedema are more susceptible to developing cellulitis due to factors such as poor circulation, lymphatic dysfunction, and chronic edema. Lipedema can compromise the lymphatic system’s ability to fight infections, increasing the risk of cellulitis. Therefore, it is essential to understand the relationship between lipedema and cellulitis and take preventive measures to mitigate the risk.
Preventive Measures for Cellulitis in Individuals with Lipedema
Preventing cellulitis in individuals with lipedema involves a multifaceted approach. It is crucial to manage the underlying risk factors that contribute to the development of cellulitis, such as chronic edema, venous disease, dermatomycosis, and obesity. By actively addressing these risk factors, the likelihood of recurrent cellulitis episodes can be significantly reduced. Additionally, non-antibiotic preventive measures, such as daily wound care, the use of protective creams and bandages, regular inspection of the feet, and maintaining good skincare practices, play a crucial role in preventing cellulitis.


Compression Therapy for Lipedema Management and Cellulitis Prevention
Compression therapy has emerged as a beneficial approach for managing lipedema symptoms and reducing the risk of cellulitis. Compression garments, such as stockings or bandages, can help alleviate pain, reduce swelling, and improve lymphatic circulation in individuals with lipedema. These garments apply pressure to the skin and veins, promoting the clearance of lymph fluid and reducing chronic edema. Additionally, pneumatic compression pumps, which mimic manual lymphatic drainage techniques, can be used as an at-home treatment option to improve lymphatic flow and prevent fluid buildup in the affected limbs.
The Importance of Timely Treatment for Cellulitis
If cellulitis does occur in individuals with lipedema, prompt medical attention and appropriate antibiotic treatment are crucial. Cellulitis can cause severe complications and lead to further damage to the lymphatic drainage routes, exacerbating the swelling and long-term management of lipedema. Therefore, it is essential to seek immediate medical assistance if any symptoms of cellulitis, such as redness, warmth, pain, or fever, arise. Following the prescribed antibiotic treatment and taking necessary precautions, such as removing compression garments until the area heals, can help manage cellulitis effectively.
Raising Awareness and Seeking Support
Raising awareness about lipedema is essential to ensure accurate diagnoses and appropriate treatment for affected individuals. Lipedema support organizations and online communities can provide valuable resources, information, and emotional support to individuals living with lipedema. By connecting with others who share similar experiences, individuals with lipedema can find solace, gain knowledge, and navigate their journey toward better health.
Conclusion
Lipedema is a prevalent adipose tissue disorder that affects a significant number of women worldwide. While cellulitis is not a direct symptom of lipedema, individuals with lipedema are more susceptible to developing cellulitis due to factors such as poor circulation and compromised lymphatic function. Preventive measures, such as managing underlying risk factors, utilizing compression therapy, and practicing good skincare, can significantly reduce the risk of cellulitis in individuals with lipedema. By increasing awareness, promoting early diagnosis, and providing appropriate treatment, we can improve the quality of life for individuals living with lipedema and mitigate the risk of cellulitis in this population. Dr. Wright and his team provide comprehensive treatment plans that consider a patient’s complete medical profile. If you’re looking for solutions to treat symptoms of Lipedema and/or cellulitis, contact us to set up an initial consultation.




