As of May 28, 2021, Dr. Wright and nearly two dozen other Lipedema experts led by Dr. Karen Herbst published 85 consensus statements making up the first ever Standard of Care Guidelines for Lipedema in the United States. Prior to it’s publication, other countries such as Germany, Spain, the United Kingdom and The Netherlands have documented and published Standards of Care for women with Lipedema, but the United States continued to lag behind it’s international colleagues. Ultimately, this resulted in American women with Lipedema being underdiagnosed, misdiagnosed, dismissed, and underserved. This publication is the first of many steps in the right direction to increasing awareness and proper treatment for women with this disease.


What are “Standard of Care” guidelines, and why are they important?
A standard Lipedema care typically refers to the formal guidelines that are generally accepted in the medical community for the treatment of a specific disease, condition, or ailment of some kind. These guidelines include important information including how to properly recognize and diagnose the condition in question, followed by the treatment process a medical provider should follow for patients with symptoms of the medical issue. The standard of care provides “best practices” developed by experts in the field who have come to a consensus of what is the most appropriate way to treat the condition at hand.
The importance of having a standard of Lipedema care in place can be best understood by highlighting what happens when a standard is not in place, as we’ve seen in Lipedema prior to today. Clinical practice guidelines are compiled by the National Guideline Clearinghouse, which provides medical providers the ability to stay up-to-date on what the standard of care is in areas of treatment. When Lipedema is not included in these national guidelines, there are no resources for physicians to refer to.
Without guidelines to the disease, symptoms checklists, or treatment plans, medical providers are unlikely to understand the disease or recognize it when they see it in their patients. Most women with Lipedema discover the disease on their own and bring it to their doctor to discuss a report being dismissed by their providers, who are unaware of the disease and have no medical expert guides as resources to refer to. This publication is a very important and exciting step to ending this cycle.
A Background on Lipedema
An estimated 11% of the world’s female population, and 16 million women in the United States alone, are affected by Lipedema, a chronic, progressive, and disruptive fat disorder. Also referred to as Lipoedema in European countries, this disorder has a variety of symptoms, ranging from generally irritating to aggressively painful. Patients suffer from swollen, sensitive areas, unsightly, bulging and indented skin, and a disproportionately larger lower body. Without answers or solutions, patients often also suffer from secondary obesity. By the time they make it to a Lipedema specialist, they report similar stories; their primary doctors had not heard of Lipedema or dismissed it as unfounded. These medical professionals’ lack of knowledge leads to improper diagnoses such as general obesity, prescribing diet and exercise as a cure, and sometimes extraordinarily invasive and dangerous weight-loss surgeries. The journey towards diagnosis and treatment takes both a mental and physical toll of those it touches, a problem that the Standard of Lipedema Care guidelines seek to alleviate.


11 Highlights from Lipedema’s Standard of Care Lipedema Guidelines
The Standard of Care for Lipedema guideline explains the following in far greater depth and should be the go-to resource for everyone in the Lipedema community, from providers to patients and their families. Below are only a few examples of action items provided, and the full standard should be consulted here for a comprehensive guide to understanding Lipedema, diagnosing it, and treating it across patients.
- Knowing the barriers to treatment for women with Lipedema. It will be no surprise to women with this disease that patients have difficulty in self-care, limited mobility, experience a social stigma attached to their increased body size, experience anxiety and/or depression, and face a lack of knowledge in their healthcare providers. Plus, there are little to no affordable treatment options, and limited non-surgical options that offer any meaningful solutions.
- There are no known medications that specifically treat Lipedema. Any use of medications or supplements should focus on reducing inflammation in the tissue, fibrosis, swelling, and pain. Medications that increase edema (swelling) or weight gain should be avoided and/or replaced with medications that are weight neutral or promote weight loss.
- Lipedema tissue is resistant to diet, exercise, or bariatric surgery. This is likely due to the fibrotic component of loose connective tissues. While weight reduction of non-lipedema obesity is beneficial to reduce metabolic complications, the difference between Lipedema and non-Lipedema weight is imperative to successful treatment.
- People with lipedema should be assessed for lipedema, lymphedema, posture, balance, muscle strength, gait and joint hypermobility. People with lipedema may benefit from postural and core exercises, muscle strengthening exercises, gait training, neuromuscular re-education, and deep abdominal breathing to increase lymphatic flow and stimulate the parasympathetic system.
- Conservative (non-surgical) therapies or lipedema may help slow progression and possibly relieve symptoms, but at present there is little evidence on their effectiveness. Standard conservative therapy for lipedema includes nutritional guidance, manual therapy, compression garments, recommendations for a pneumatic compression device (external pump) and a home exercise plan.
- Lipedema reduction surgery is currently the only available technique for removing abnormal lipedema tissue. Adipocytes, nodules, fibrotic extracellular matrix, and other non-adipocyte components cannot be removed without lipedema reduction surgery, which utilizes suction lipectomy (liposuction), excision and manual extraction that spares blood and lymphatic vessels. Lipedema reduction surgery significantly improves symptoms,mobility, stance, gait, valgus rotation/deformity of the knee and ankle, quality of life, and redistributes and restores the plantar arch. It also improves lymphatic symptoms, reducing the need for compression and manual therapy and can improve lymphatic function as shown by radionucleotide lymphangioscintigraphy.
- Most people with lipedema have leg pain, all have leg swelling, either pitting or non-pitting, and many have underlying chronic venous disease. The physical examination should include inspection and palpation of pulses in the limbs. Pulse palpation in people with lipedema may be difficult and painful due to limb size. Common venous conditions seen in people with lipedema include increased risk for venous thromboembolism and conditions associated with chronic venous disease: varicose veins, chronic venous insufficiency, and telangiectasias (spider veins).
- Updated Definition of Lipedema: While lipedema is still considered a fat disorder, new evidence further clarifies that all of the components loose connective tissue in the subcutaneous space maybe affected by lipedema these include adipose tissue, fibrous tissue lymphatic , veins and arteries of the subcutaneous space. Therefore lipedema should be considered a loose connective tissue disorder not merely a fat disorder even though abnormal fat accumulation is a principal characteristic of lipedema.
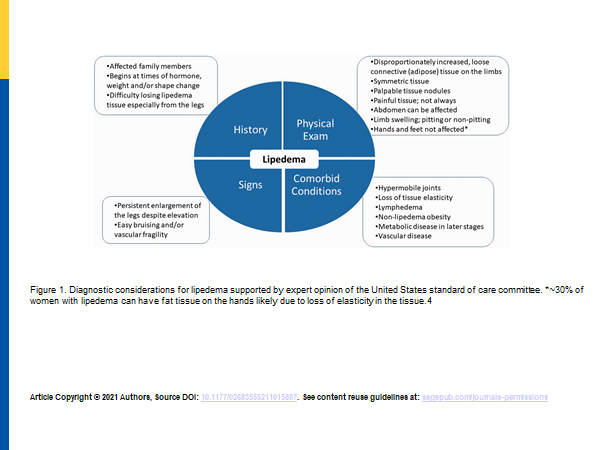
- The clinical criteria for the diagnosis of lipedema was agreed on.

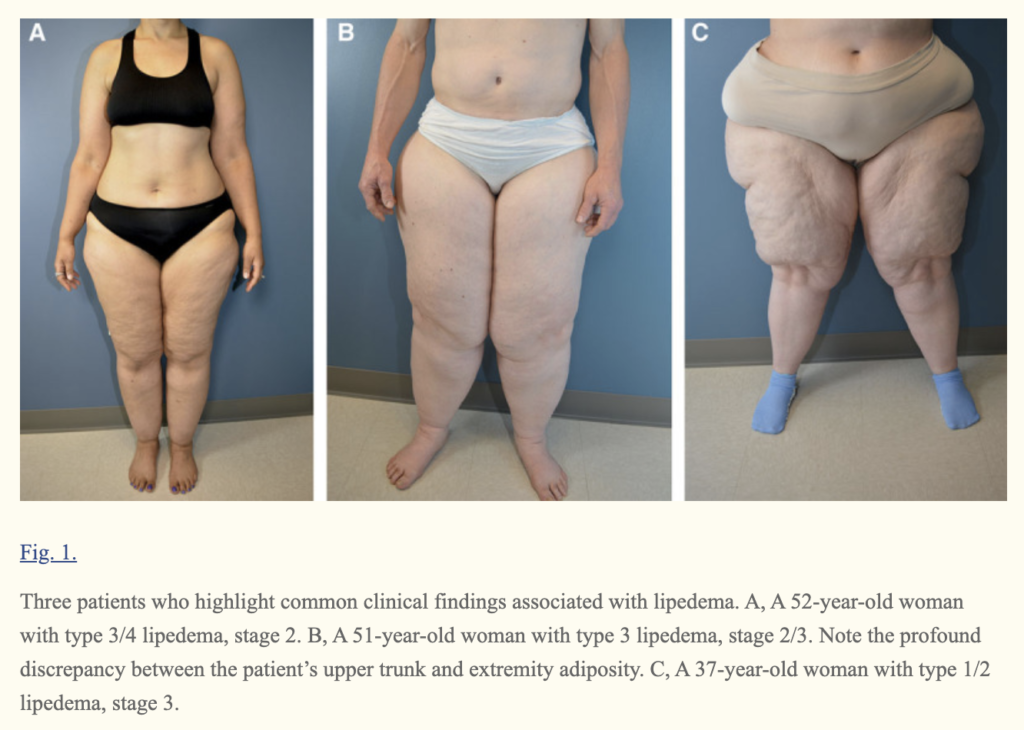
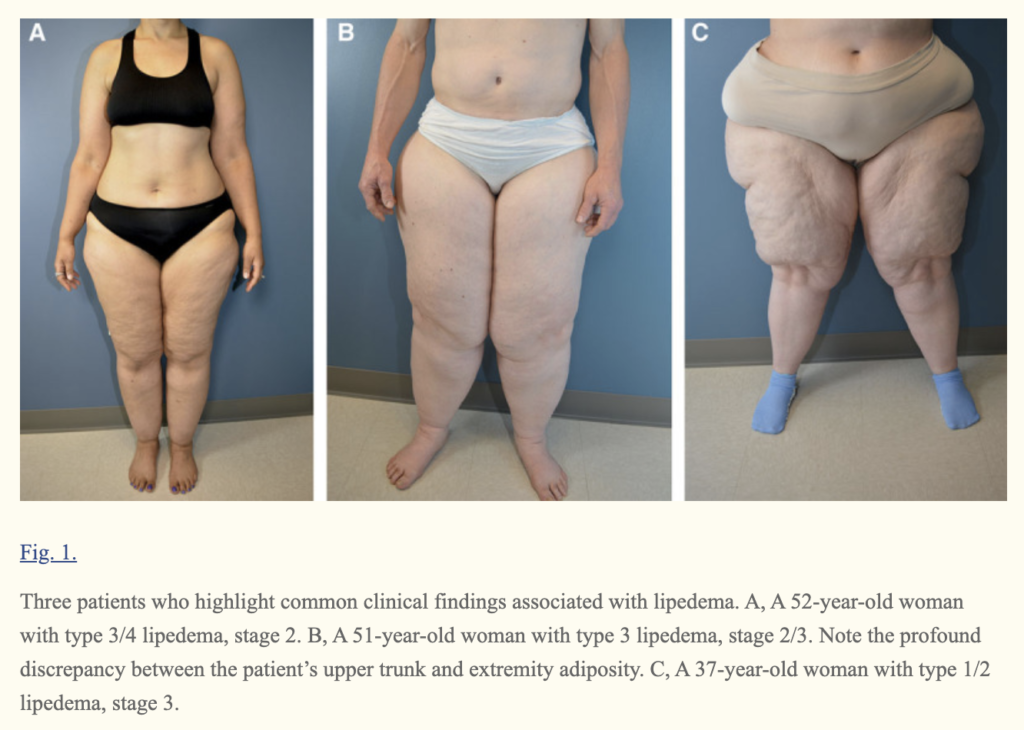
- Stages and Types of Lipedema was agreed on. Lipedema was divided into stages 1 through 3 stage 1. Stage one is typified by small nodules in the subcutaneous fat stage 2 is characterized by larger nodules and visible indents in the surface of the fat in stage 3 is characterized by lobules in the skin. Some authors have described a 4th stage for lipedema and called it lipolymphedema. The proposed 4th stage would be when lymphatics are affected and cause a secondary lymphedema from the lipedema. Our current understanding of lipedema is that lymphatics are affected at all stages of lipedema. While stage 2 and 3 more often show lymphatic impairment than stage 1 there is no clear stage of lipedema where lymphatic are affected.
TABLE 1: Classification of lipedema severity according to Stößenreuther (2001).
| STAGE | SKIN SURFACE | SUBCUTANEOUS ADIPOSE TISSUE |
| STAGE 1 | NORMAL | SMALL NODULES |
| STAGE 2 | UNEVEN | BIGGER NODULES |
| STAGE 3 | LOBULAR DEFORMATION | LARGE NODULES & DEFORMITIES |
TABLE 2: Types of lipedema, used to describe the location of lipedema fat
| TYPE | LOCATION |
| TYPE I | BUTTOCKS, HIPS (“SADDLEBAGS”) |
| TYPE II | BUTTOCKS TO KNEES, WITH FOLDS OF FAT AROUND THE INNER KNEE |
| TYPE III | BUTTOCKS TO ANKLES |
| TYPE IV | ARMS |
| TYPE V | LOWER LEGS |
- Common Diseases Associated with Lipedema Diagnosis.
Common complications of lipedema including lymphedema non lipedema obesity venous disease and hypermobile joints were described.
Put Criteria for EDS hs . Beighton Criteria.
Table 2: Beighton’s joint hypermobility score.
| The ability to | Right | Left | |
| (1) Passively dorsiflex the fifth metacarpophalangeal joint to ≥90◦ | 1 | 1 | |
| (2) Oppose the thumb to the volar aspect of the ipsilateral forearm | 1 | 1 | |
| (3) Hyperextend the elbow to ≥10◦ | 1 | 1 | |
| (4) Hyperextend the knee to ≥10◦ | 1 | 1 | |
| (5) Place hands flat on the floor without bending the knees | 1 | ||
| Total possible score | 9 |
One point can be gained for each side for maneuvers 1–4 so that the hypermobility score will have a maximum of 9 points if all are positive. (12) 12. Vounotrypidis P, Efremidou E, Zezos P, et al. Prevalence of joint hypermobility and patterns of articular manifestations in patients with inflammatory bowel disease. Gastroenterol Res Pract. 2009;2009:924138. doi:10.1155/2009/92413
References:
Standard of care for lipedema in the United States
https://pubmed.ncbi.nlm.nih.gov/



