3 independent studies find lipedema is an inherited condition.
As reported by The Cleveland Clinic [#} on its website, the exact cause of lipedema is unknown, but the condition runs in families and may be inherited. This statement is supported by three independent studies conducted by leading research teams in Europe who validated lipedema is a genetic condition. Lipedema appears to primarily affect females, presumably driven by estrogen as it usually manifests at puberty. Lipedema disease is different from obesity and is often misdiagnosed as primary obesity because these conditions commonly overlap.
Researchers hope to continue to study as many families as possible with multiple cases of lipedema to create a stronger genetic linkage and determine the biochemical makeup of this disorder. Having this data may help researchers identify the gene that causes lipedema to increase understanding and improve treatment for this painful condition.
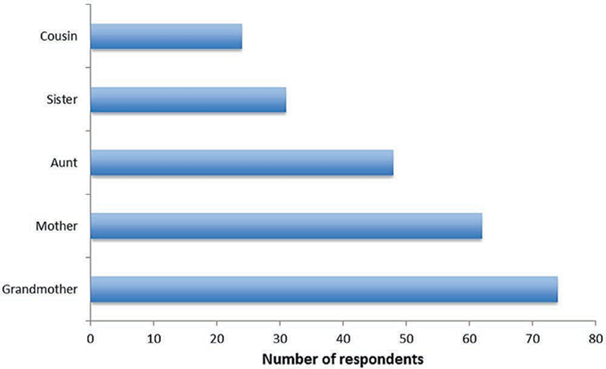
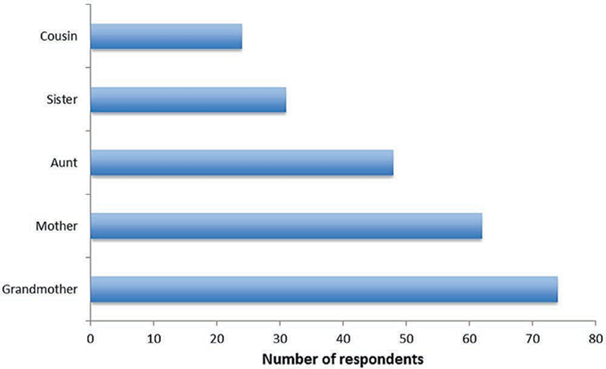
Fig 1. Bauer and etal. study reaffirms relatives of lipedema patients also suffer with lipedema. In most cases, grandmothers and mothers were affected the most, followed by aunts, sisters, and cousins.
The familial nature of the condition suggests that lipedema can demonstrate heritability[1]. The exact nature of the form of inheritance is difficult to determine.
Of lipedema patients who participated in a study, 73% reported they had one or suspected multiple family members also had lipedema. Most frequently affected was the mother (38%), followed by grandmother (17%), aunt (8%), sister (6%) and cousin (5%).


A study from 2010 showed that within six families of more than three generations with lipedema disease, a genetic autosomal-dominant hereditary pattern [2]was found.
Frequent studies of mother-to-daughter mode of inheritance led researchers to theorize lipedema is a genetic disorder.


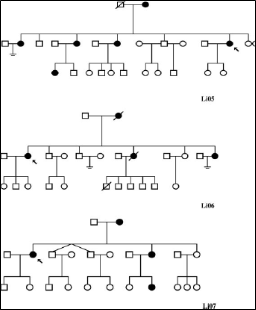
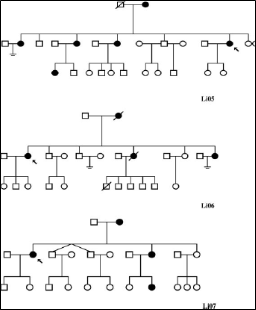
Fig 2. The largest family pedigrees (with a minimum of three living affected members in at least two generations) are demonstrated in Figure 2.
Family clusters of lipedema where more than one family member has the condition indicates a genetic component with a possibly X-chromosome[3] dominance inheritance pattern.
All affected family members were female first- or second-degree relatives of female patients.
One family had six living affected members in three generations, two families had five affected members, two had four affected members, and one further family had three living affected members.
As lipedema appears to be most common at puberty, it is reasonable to assume that hormonal influence underlies the marked female limitation shown in studies to date.
Estrogen is also considered to play a key role in regulating the manner of development of the condition.
—
Study participants:
Between all three studies, women ages 16-83 (average age, late 30s)
Do you suspect you or a loved one may have lipedema? We can confirm your condition and start you on your journey to feeling better. Contact us to schedule an appointment, today.
References
Bauer AT, et al. Plast Reconstr Surg. 2019 Dec;144(6):1475-1484 https://pubmed.ncbi.nlm.nih.gov/31764671/
Ghods M, Georgiou I, Schmidt J, Kruppa P. Disease progression and comorbidities in lipedema patients: A 10-year retrospective analysis. Dermatologic Therapy. 2020;e14534. https://doi.org/10.1111/dtch.14534
Child AH, Gordon KD, Sharpe P, Brice G, Ostergaard P, Jeffery S, Mortimer PS. 2010. Lipedema: An inherited condition. Am J Med Genet Part A 152A:970–976. https://pubmed.ncbi.nlm.nih.gov/20358611/ and https://www.researchgate.net/publication/346917917_Disease_progression_and_comorbidities_in_lipedema_patients_A_10-year_retrospective_analysis/figures
# Cleveland Clinic Lipedema https://my.clevelandclinic.org/health/diseases/17175-lipedema
[1] Heritability is a measure of how well differences in people’s genes account for differences in their traits
[2] Autosomal dominant inheritance is a way a genetic trait or condition can be passed down from parent to child.
[3] The X chromosome is one of two sex chromosomes. Humans have two sex chromosomes, the X and Y. Females have two X chromosomes in their cells, while males have X and Y chromosomes in their cells.
In this blog, a woman shares her very real experience finding out she has lipedema disease.
In my 30 years of life, or at least over the last ten years, my weight and chronic pain has left me at a loss. I’ve tried every crash diet that exists — Keto, HCG, Phentermine, low-fat & high-protein, intermittent fasting, and the Beyoncé detox of spicy lemon water. I’ve trained and ran half marathons, hired personal trainers, seen a nutritionist, and eventually, when my anxiety and depression took over, started therapy. I’ve really tried not to be fat, but here I am.
My ego would like me to point out that I’m not an obese person, although my doctor would disagree. I was never an overweight kid and remained active into adulthood. I played basketball, ran track, and practiced a balanced diet. When I felt pain, I contributed it to my weight. When the pain turned debilitating after starting birth control at 19 and my weight shot up, my doctor told me to “lay off the cake.” Had he spent more than ten minutes with me, I could’ve explained that I’m not a fan of cake, and he was a dick.


Eleven years later, as I ring in my 30th birthday, I wish I could say I’ve learned to love my body and embraced the “Every Body is Beautiful” campaign. But I’ve been worn down, embarrassed, and depressed. In the two minutes between a shower and getting dressed that I avoid eye contact with myself, I evaluate the painful bruising all over my legs. I take in all my weird, bulky cellulite that, for some reason, always appears extra-fatty while also extremely firm. I avoid physical touch because even a gentle tap is painful. I teeter between sadness, helplessness, and anger.
Why do I wear a small t-shirt and an XL pant? If I lose weight, why is it always in my upper body, and I remain a size 16 jeans at any weight? My god, I cannot afford to lose another cup size. I start to furiously ask Google all of these questions. I ask her why my knees have so much fat around them, why I bruise so easily, and why I can’t run anymore without incredible pain. As I start to go down the 2 AM rabbit hole, I come across a medical journal in Germany about fat disorders and start reading about something called Lipedema. From here, my journey to healing (but also a lot more pain and anger) begins.
Lipedema is a subcutaneous adipose tissue disorder, in which the blood vessels and lymphatic system do not properly move toxins out of the body through the lymph nodes. This causes easy bruising, swelling, bulky legs (and sometimes arms), chunky looking cellulite that are actually lumpy cyst-like bulges, and cuffs around the wrists and ankles. Essentially, the body doesn’t drain liquid, and the “clogging” causes fatty masses all over the body. Specialists estimate this affects approximately 10% of women across the world, yet it goes widely undiagnosed. Or, more commonly, misdiagnosed as obesity.
After reading as much as I could about lipedema disease and the handful of doctors who study it in the US, I brought this information to my doctor. He scoffed at me, requested I stop self-diagnosing, and suggested I get lap band surgery. He would prefer I get a serious surgery to remove part of my stomach, despite all my labs coming back athlete-level healthy. Upon a second request for a referral, he suggested I increase my anti-depressant dosage, and again, stop reading fake medical journals. I left in tears, half out of anger and half out of embarrassment.
After a few days of additional research, I started making calls. I found the best doctor specializing in subcutaneous adipose tissue (SATs) disorders, flew to Arizona from Texas, and was immediately diagnosed. I was put on a strict diet, prescribed a compression machine and compression garments, and am scheduled to get out-patient surgery to drain my excess fluid by the end of the year. It is generally an inconvenience, but I’m psyched for what comes next.


I’ve just completed a DNA test for a research study related to these disorders and will participate to evaluate the affect this surgery has on the disease. While I plan to journal my own experience through the process, I’m particularly interested in spreading the word about Lipedema, given my experience with gas lighting from my many male doctors. While in AZ, each team member had story after story about women being told they were crazy, that they were lying about their diets, exaggerating their pain, and simply not working hard enough.
The thought of one person going through a serious surgery like the lap band procedure recommended to me — when it won’t actually help — terrifies me. Stay tuned for my many updates, but in the meantime, feel free to reach out to me if you think any of the following apply to you:
I’m happy to direct to you those who have helped me. Stand up for yourselves, girlies. Be your own advocates, and down with the patriarchy.
We are very grateful to Ms. Karwick to allowing us to share her experience.
Cat Karwick
Follow
Content Creative. Women’s Health Advocate. Experience calling out mansplainers and finding carb substitutes.
Following
Sep 23, 2019 · 4 min read
This article is from Medium.com and was posted on Sept 2019. https://medium.com/@karwickca/lipedema-ruined-and-saved-this-fat-girls-life-26ce65ec9185
The arrival of COVID-19 on the global health scene has put the vast majority of the population in a position where there seem to simply be more questions than answers. As this new strain has made its way across the planet, experts have been working hard to identify trends, put protective orders in place, and ultimately, look for a cure for something that’s undeniably difficult to contain. It’s generally assumed that a little can go a long way in preventing the spread of COVID-19, but one of the most daunting aspects of the virus seems to be how it puts those with underlying health conditions at heightened risk. So what does that mean for those individuals that suffer from Lipedema disease? Many are asking if this condition is a gateway to contracting COVID-19.
While COVID-19 is new and there is much left to be learned, medical experts have been able to pinpoint a few categories of individuals that are at an increased risk of contracting the disease. To date, those are considered to be individuals over the age of 65, those that are currently taking medications that ultimately suppress the immune system and those with underlying health conditions such as diabetes, hypertension, lung disease or cancer. COVID-19 has shown a trend of quickly being able to infiltrate the lungs of those that experience any or a combination of these conditions.
The chronic nature of Lipedema makes it easy for some to assume that those that suffer from the condition are more susceptible to contracting COVID-19. Lipedema is widely recognized as a condition where fat cells accumulate disproportionately throughout the lower extremities with the possibility of the condition extending into the torso and upper arms as well. Lipedema is associated with painful swelling in these same extremities and those individuals suffering from the condition are often prone to excessive bruising.
Lipedema presents in three distinct stages with varying sizes and severity of fat cells and masses developing. Histology of tissue sampled from patients that suffer from Lipedema often shows increased macrophage inflammation numbers—a scenario very common in areas of infection throughout the body. Patients presenting with Lipedema are often noted to have dilated blood and lymphatic micro-vessels in the affected areas as well as fat cells with increased dimensions. It’s not uncommon to see the increased development of new blood vessels in Lipedema thigh skin and fat tissue.
While Lipedema directly affects fat cells and causes significant inflammation in the tissue of the extremities, patients who suffer from Lipedema are not presumed to be at an increased risk of contracting COVID-19 at this point in time. This chronic condition is assumed to exclusively affect tissue and unless an individual with Lipedema ends up with a severe infection or the condition transitions into Lymphedema, they do not appear to be at increased risk. That being said, the chronic nature of this condition does mean that an individual with Lipedema who contracts COVID-19 could be more susceptible to presenting with more serious symptoms overall.
Steps should be taken by those with Lipedema to prevent the transmission and contraction of COVID -19 in line with those regulations put in place by the CDC for the general population at this time. It’s essential to perform regular handwashing of at least 20-second at a time using warm water and soap with hand sanitizer working as an alternative option. Staying indoors and distancing from others is imperative to preventing the spread of the infection and if a trip outdoors is necessary, a mask should be worn to prevent transmission by air. Those that develop symptoms including a cough, fever or shortness of breath are encouraged to contact their physician by phone immediately.