June is Lipedema Awareness month, one in which the Lipedema community focuses (even more than usual) on how to reach women who have lived with this painful and distressing disease. While we’ve seen great strides in awareness, insurance coverage, and slightly greater recognition of this disease in the medical community, we continue to fight an uphill battle as women are underdiagnosed or completely dismissed when discussing their struggles and side effects with their providers. As a result, our team has put together some of the most important and impactful information for all of you, and we’re kicking off the month with a webinar from a team of lipedema experts.
Join us on Tuesday, June 7th, 2022 at 8 pm ET to listen to our panel discuss Recognizing Lipedema and Treatment Options. This is a FREE event!
Register here, or listen to the recording following the webinar at tactilemedical.com/education.
Drs. Steve Dean, Thomas Wright, and Tony Gasparis with Julie Green, OTR/L CLT-LANA, WCC, CLWT discuss lipedema – the pathophysiology, association with vein disease, conservative treatments, and surgical options available for patients.


What Is Lipedema Reduction Surgery?
Lipedema reduction surgery is different from cosmetic liposuction. Studies have shown that women with Lipedema have impaired lymphatic function. Lymphatic fluid promotes the collection of fat cells, which can cause the obstruction of lymphatic capillaries (branch-like blood vessels). Extra care must be taken to avoid injuring the lymphatic system and making an already stressed system worse. Using blunt cannulas generous and special surgical techniques, studies have shown that lymphatic function can actually improve after this type of liposuction in women with Lipedema. The goal of lipedema reduction surgery is to remove the fibrous tissue and maximally reduce the lipedema tissue. It is a debulking surgery, not a cosmetic surgery.
There are two specialized liposuction techniques that have been shown in studies to benefit individuals with lipedema: water-assisted and tumescent liposuction. In addition to the surgical equipment used, it is important to choose a surgeon with experience and one that is cautious when performing lipedema surgery. These factors can have an important influence on protecting lymphatic flow and function.
Who Is an Ideal Candidate for Lipedema Surgery?
Despite affecting an estimated 11% of women around the world, Lipedema is not yet widely known. Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, but sometimes spreading occurs in the torso, and in many cases, excessive clustering of fat cells is noticed in the arms as well. Regardless of the affected area, the symptoms are equally debilitating, and unfortunately, these fat cells are equally resistant to both diet and exercise programs.


Unlike Lymphedema or general obesity, Lipedema has a tendency to affect both limbs equally and generally becomes more apparent over the course of time. Lipedema’s progressive nature makes getting a proper Lipedema diagnosis and treatment imperative and extremely time-sensitive – as the disorder progresses so does the pain, immobility, and discomfort.
In addition to the characteristic disproportionate fat accumulation, there are specific physical signs and symptoms of Lipedema. Do any of the following Lipedema symptoms sound like something you regularly experience?
3 Stages of Lipedema
Overall, Lipedema appears in a series of three stages. Do any of these sound like you?
Stage 1: The patient’s skin is flat and stretched over pearl-sized nodules.
Stage 2: The patient’s skin is indented, covering a layer of fat cells that look like pearl to apple-sized masses.
Stage 3: Skin is indented, sometimes with much larger bulges, and skin covers pearl-sized nodules in combination with excessively large fat masses, causing lobules along the legs, hips, and thighs and frequently extending to the torso or upper arms.


| Photo credit: Linda Anne Kahn at Integrative Treatment of Lipedema |
Below are conditions that can be confused with and can affect people with Lipedema. Because there can be so much overlap in appearance and symptoms, only clinicians with the training and experience to diagnose and treat these conditions can differentiate them.
When is the best time to get lipedema surgery?
There are two categories of treatment, surgical and non-surgical. Insurance providers require patients first try non-surgical treatment options before they’ll consider approving lipedema surgery, and Lipedema providers should be able to walk patients through this. While Lymph-sparing liposuction is the only treatment option that can provide permanent results by removing the lipedema fat, non-surgical options can help slow progression and are also necessary post-surgery (so it’s still important to practice them!).
Non-Surgical Treatment Options
To the dismay of patients, wearing medical-grade, tight compression garments 24-hours per day, seven days per week, is the key to improving circulation for the lymphatic system, making this a go-to prescription from Lipedema experts. Compression garments come in a variety of strengths and will be prescribed based on the stage and type of affected areas. The tighter the compression, the better.
A healthy and consistent lifestyle of clean eating and low-impact exercise to address obesity will also help with Lipedema. A diet focused on low-carb and low-sugar has proven successful. Low-impact exercise such as walking, water aerobics, yoga, or gymnastics has also reported success. Patients must avoid yo-yo dieting while also permanently losing or, at the very least, maintaining their weight. What works for one patient may not work for another. Diet and exercise recommendations and healthy practices are essential, but ultimately should be based on the individual with the understanding that weight gain is not an option.
Some patients opt-in to Manual Lymph Drainage massage (MLD), a gentle skin massage used to stimulate the circulation of the lymphatic system. While experts have yet to find significant evidence that MLD helps with Lipedema directly, some patients prefer it for its “hands-on” nature to addressing their symptoms.
Lymph-Sparing Liposuction for Lipedema
For patients in the later stages of Lipedema, the pain and disruption to daily life are not permanently addressed with compression garments, diet, and exercise alone. Traditional liposuction that uses general anesthesia, radio frequencies, ultrasound, or lasers are possibly damaging to the lymphatic vessels, and as such are not an option for Lipedema patients, either. However, Lymph-sparing liposuction is safe, using surgical techniques that avoid lymphatic injury, and the use of local tumescent anesthesia reduces the risk of complications. Generally, the most painful areas should be treated first, starting high on the legs and then moving downward in future surgeries.
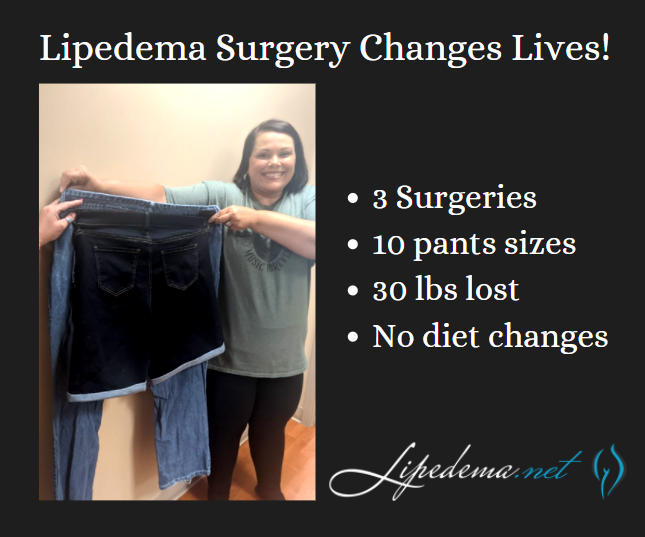
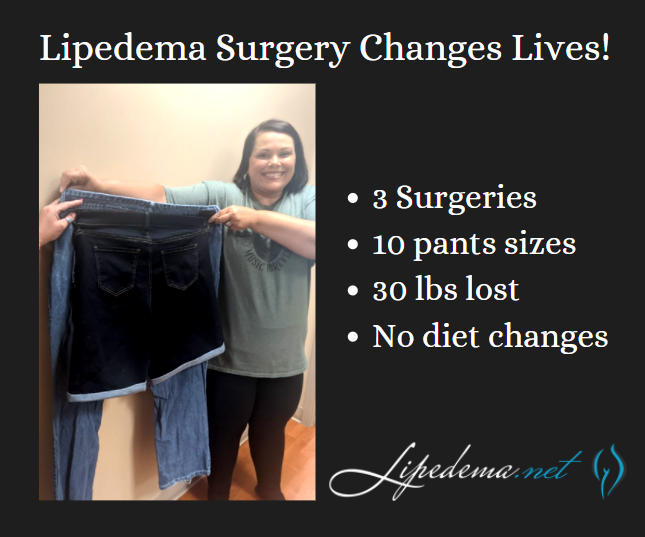
What Results Can I Expect from Lipedema Surgery?
Perhaps the most noticeable benefit of lymph-sparing liposuction is how it is able to reduce the amount of subcutaneous fat tissue in the body. Lipedema reduction surgery not only significantly reduces fat tissue, but also removes fibrous tissue, making the limbs lighter, smaller, less tender, and smoother. It is critical to follow your physician’s guidelines to reduce any swelling and inflammation before the treatment. This is done by wearing compression garments and wraps along with receiving manual lymph drainage for several weeks following lipedema surgery and beyond. Patients wear medical-grade compression clothing for at least 8 weeks, and manual lymph drainage and massage are typically recommended as an ongoing and regular treatment.
Your tissue will be decongested, allowing your liposuction treatment to be as successful as possible. Some slight swelling and bruising may return immediately following the procedure, but this is expected and should subside over time. Some patients also report numbness as their nerves in the treated areas respond to treatment. Numbness may last for several months and up to one year, but when compared with the reduction in fat tissue, patients still see this as a huge improvement. Compression is critical to be maintained after the lipedema surgery as well, as the lymphatics are reestablished. The lymphatic function is often improved.
Lipedema Reduction Surgery Risks
One of the most beneficial aspects of lymph-sparing liposuction is that the treatment does not rely on general anesthesia. While general anesthesia is used for a variety of treatments, it can cause complications for individuals with lipedema. In fact, it can cause complications in as high as 0.3% of liposuction treatments when used. Instead, lymph-sparing liposuction uses tumescent anesthesia to avoid these unwanted complications. In fact, general anesthesia can cause serious complications and even death in up to 0.3% of liposuction treatments when used. Patients are conscious for the duration of treatment, while the tumescent liquid acts as a local anesthetic in the treatment area. Patients take pain kills ahead of time to help with discomfort, and through the process feel little pain, and if anything, pressure in the area being treated.
Lipedema reduction surgery also makes sure to avoid any additional risks for the treatment. This type of liposuction procedure limits the amount of fat tissue that will be removed at once, and a follow-up appointment is scheduled for the day following the procedure to ensure the treatment and recovery are going as planned. While that may not seem like a benefit at first, it will actually make sure your body does not take any additional trauma than what is needed. The general amount of fat tissue that can be safely removed is around 5.0 liters. Smaller cannulas are also used to also keep down the risk of trauma to the body and an already compromised lymphatic system.
Start Your Life-Changing Journey
Even with all the challenges presented by lipedema, there are those who you can trust. Dr. Wright continues to strive for better education, research, and coverage for the lipedema community. Do not let these challenges bring you down even further; let Dr. Wright and his expert team help you to reduce the symptoms of lipedema and live your life fully! Dr. Wright can help find the right procedure to help manage your lipedema symptoms. Don’t let lipedema take over your life; contact us today!