Diseases That Look Like Lipedema: Understanding Misdiagnosis and Getting Accurate Care
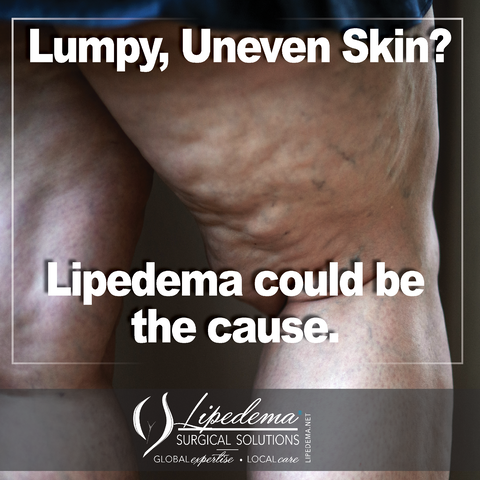
When you’re struggling with painful leg swelling, easy bruising, and fat deposits that refuse to budge despite your best efforts with diet and exercise, you might suspect lipedema. But here’s something important to know: not every case of large legs with ankle cuffs is actually lipedema. Several other conditions can mimic the appearance of this complex disorder, making an accurate diagnosis essential for effective treatment.
At Dr. Wright’s practice in St. Louis and O’Fallon, Missouri, we understand that awareness and recognition of lipedema is poor among both the public and medical professionals. This leads to two significant problems. Some women who truly have lipedema go undiagnosed, while others receive a lipedema diagnosis when they’re actually dealing with a different condition entirely. Both situations lead to frustration, ineffective treatments, and delayed access to proper care.
What Is Lipedema?
Before we explore the conditions that can be confused with lipedema, let’s establish what lipedema actually is.
Lipedema is a chronic condition characterized by the abnormal and symmetrical accumulation of subcutaneous adipose tissue (fat) in the legs, arms, and sometimes other body parts. Unlike ordinary obesity, the fat deposits in lipedema are painful or tender and do not respond well to conventional diet and exercise, often remaining unchanged even as other body fat decreases.
The condition typically progresses through stages, from mild limb enlargement to more severe cases where mobility is significantly impaired. Lipedema is also characterized by a tendency to bruise easily and may include symptoms such as fibrosis, a condition that involves the thickening and hardening of tissue.
While it is believed to have a genetic component, lipedema almost exclusively affects women and is often linked to hormonal changes associated with puberty, pregnancy, or menopause. Coexisting conditions such as lymphedema, which involves swelling due to lymph fluid buildup, and venous insufficiency are common.
The Challenge of Diagnosing Lipedema
Diagnosing lipedema is not straightforward. It cannot be determined solely by examining photos or observing symptoms, as several other conditions appear similar. Accurate diagnosis requires a comprehensive medical history, thorough physical examination, and often, diagnostic testing. Unlike other medical conditions, no blood or objective laboratory test can definitively diagnose lipedema.
This diagnostic challenge is why seeking care from a lipedema specialist in Missouri is so important. Dr. Wright has extensive experience differentiating lipedema from similar conditions and uses a comprehensive approach to ensure accurate diagnosis.
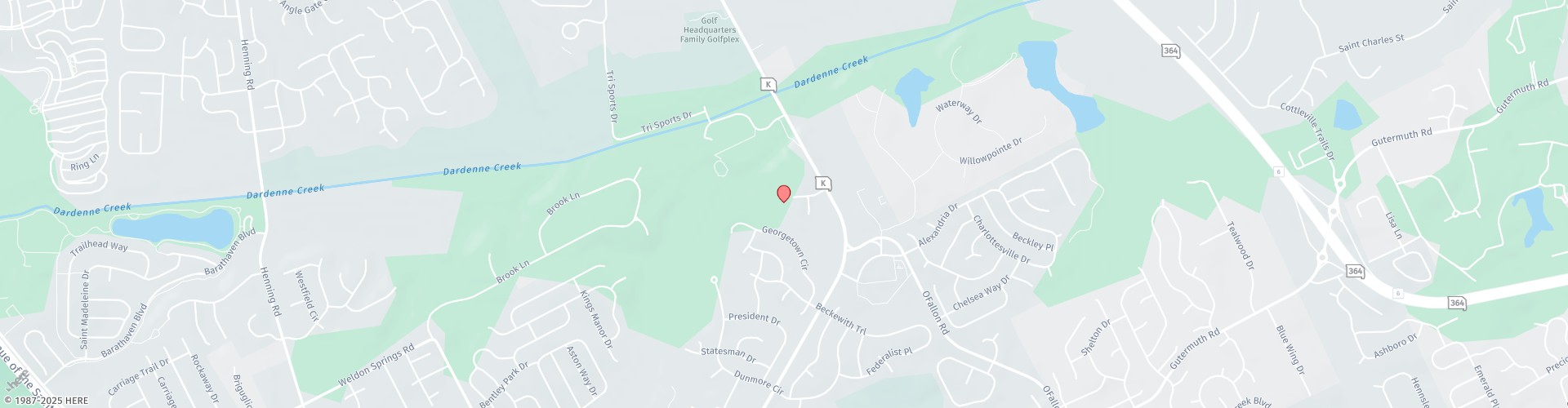
The 4-Step Process for Lipedema Diagnosis in St. Louis
Getting a diagnosis for lipedema involves several steps, primarily because it’s often misunderstood and can be confused with other conditions like obesity or lymphedema. Here’s the typical process we use for obtaining a lipedema diagnosis:
Step 1: Medical History Review
The first step is a thorough review of the patient’s medical history. This includes discussing symptoms, family history of similar issues, and any changes in the condition related to life events such as puberty, pregnancy, or menopause, since lipedema is known to be hormonally influenced.
Step 2: Physical Examination
A healthcare provider, often a specialist in lymphatic disorders, such as Dr. Wright, will perform a physical examination. They look for the typical pattern of fat accumulation (symmetrical, sparing the feet and hands), changes in skin texture such as subcutaneous nodules, and signs of pain or bruising.
Part of the exam must include a test for nonpitting and pitting edema. This assessment consists of the Bjork or Bow Tie test, which evaluates the texture of the skin using light pressure, and a Stemmer’s test on the feet and hands. These specialized techniques help differentiate lipedema from other swelling disorders.
Step 3: Symptom Assessment
The provider will assess symptoms like pain, tenderness, and easy bruising in the fatty areas, which are characteristic of lipedema. We also evaluate how your symptoms impact your daily life, work capacity, and emotional wellbeing.
Step 4: Ruling Out Other Conditions
Since no specific test can definitively diagnose lipedema, part of the diagnosis process involves ruling out other conditions. This may include tests for lymphedema (such as lymphoscintigraphy), venous insufficiency (using Doppler ultrasound), and sometimes heart or kidney conditions that can also cause limb swelling.
Additional Diagnostic Steps
Specialist Consultations: Patients might be referred to various specialists, including those skilled in vascular medicine, dermatology, or bariatric medicine, to further analyze symptoms and eliminate other potential causes.
Imaging Tests: In some cases, imaging tests such as MRI, ultrasound, or CT scans can be used to observe the distribution of fat and check for other abnormalities.
Lipedema Staging: If lipedema is diagnosed, the doctor may stage the disease based on its severity and progression. Staging helps in planning appropriate treatment and management for lipedema patients in O’Fallon and St. Louis.
Educational Resources and Support: Patients are often provided with information about the condition and directed towards support groups and resources to help manage the emotional and physical impacts of lipedema.
Getting a correct diagnosis of lipedema can be challenging due to a general lack of awareness about the condition even among medical professionals. Patients might need to consult with multiple healthcare providers before receiving an accurate diagnosis. That’s why working with an experienced lipedema specialist like Dr. Wright is so valuable.
Common Lipedema Lookalikes: Conditions That Mimic Lipedema
Understanding what conditions can be confused with lipedema helps both patients and healthcare providers pursue the right diagnostic path. Here are the most common lipedema lookalikes:
Other Lipomatosis and Fat Disorders
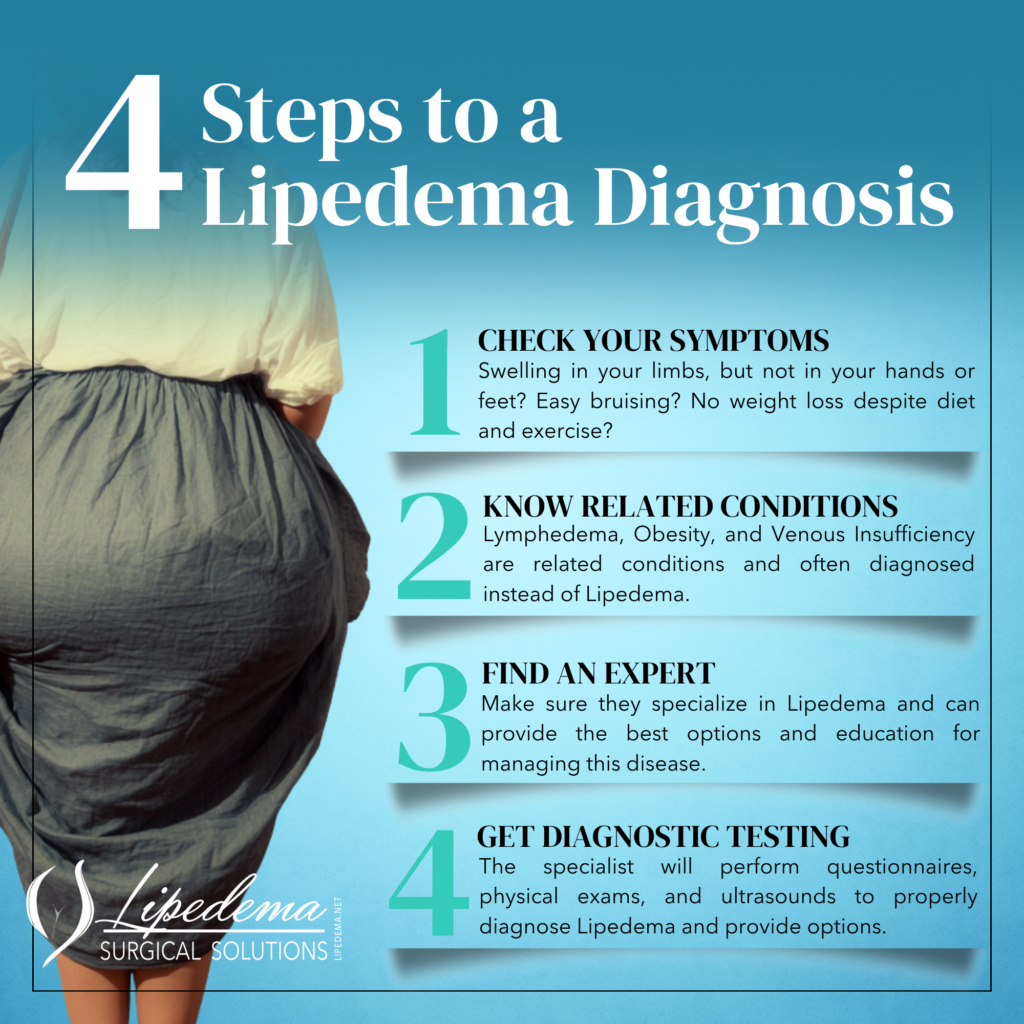
Madelung’s Disease
Madelung’s Disease is characterized by multiple painful subcutaneous tissues that can be mistaken for the fat nodules typical of lipedema. This condition typically affects the neck, shoulders, and upper trunk, though it can sometimes involve the limbs. The fat deposits in Madelung’s Disease are often more localized and asymmetrical compared to the symmetrical pattern seen in lipedema.
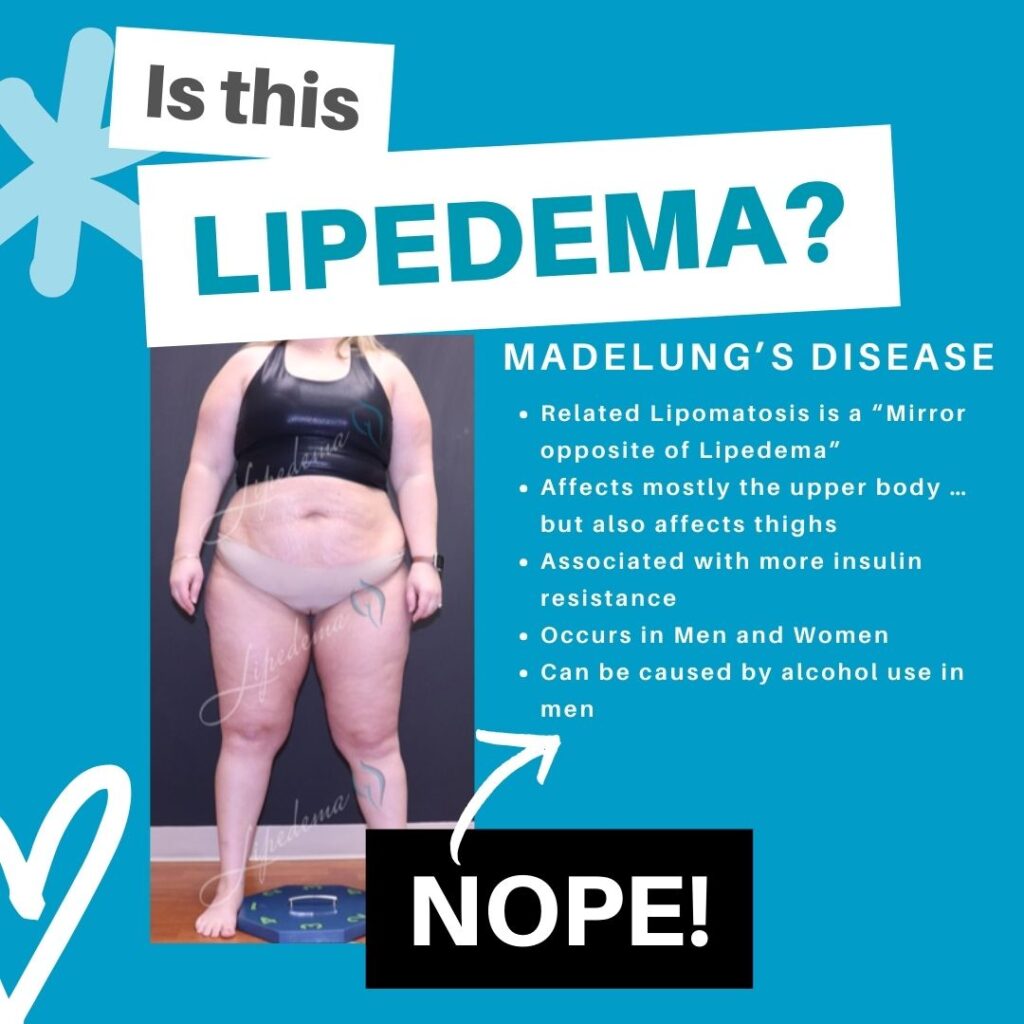
Dercum’s Disease (Adiposis Dolorosa)
Dercum’s Disease involves the growth of painful lipomas (benign fatty tumors) across the body, which are often misidentified as lipedema. Unlike lipedema, where the fat is diffusely distributed in affected areas, Dercum’s Disease presents with distinct, movable fatty lumps that can occur anywhere on the body. The pain in Dercum’s Disease is often more localized to the lipoma sites.
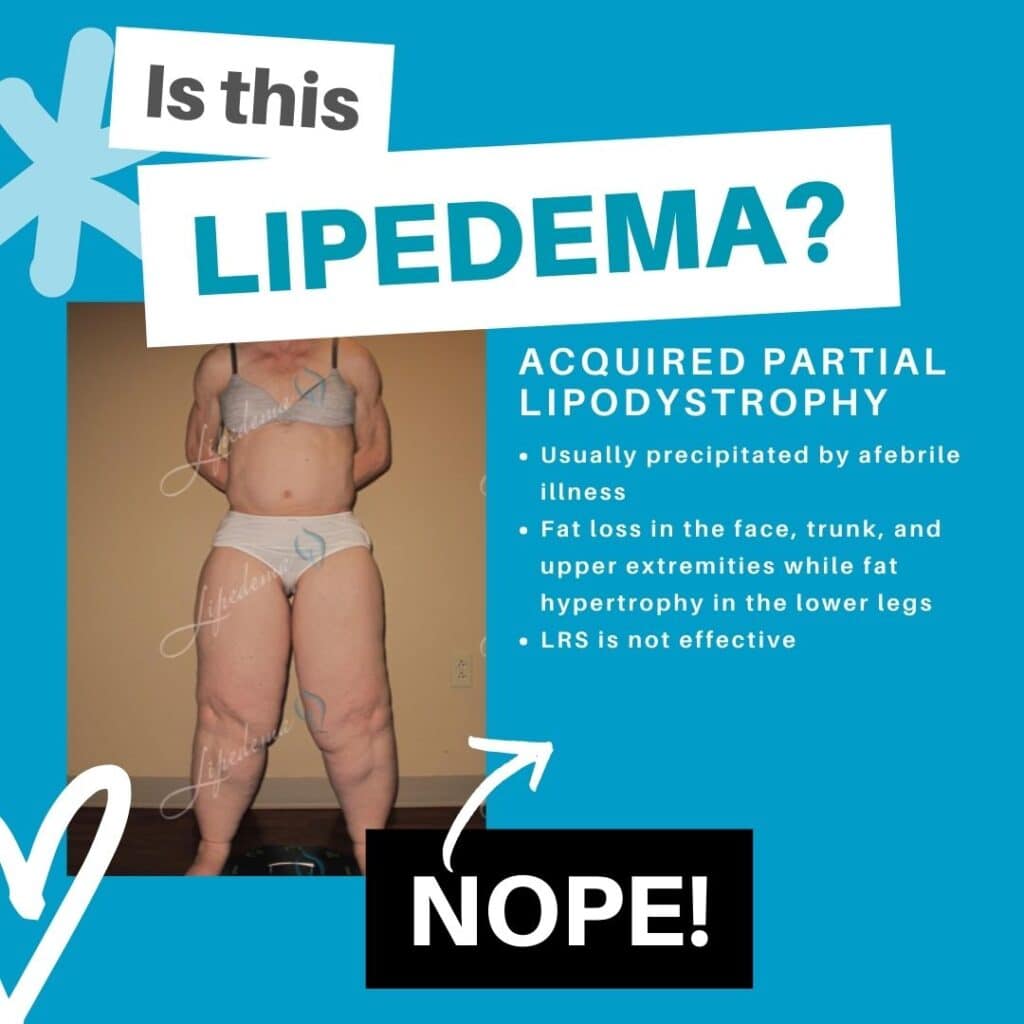
Acquired Lipodystrophy
Acquired Lipodystrophy is a condition in which fat tissue is lost or redistributed, and it can sometimes present similarly to lipedema. However, lipodystrophy typically involves fat loss in some areas and abnormal accumulation in others, creating a distinct pattern that differs from the symmetrical accumulation seen in lipedema.
Vascular and Lymphatic Conditions
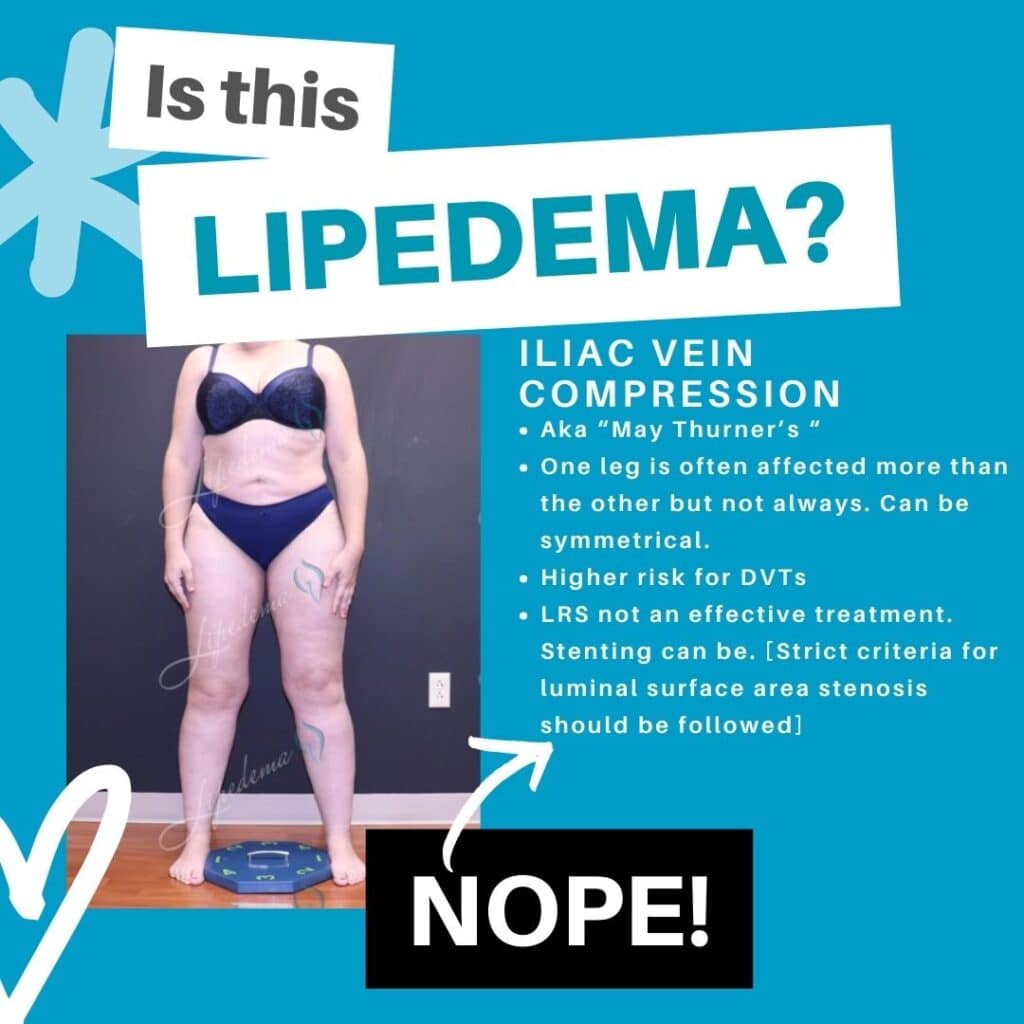
Iliac Vein Compression
Iliac Vein Compression can cause leg swelling and pain, similar to symptoms seen in lipedema. This vascular condition occurs when the iliac vein (a major vein in the pelvis) becomes compressed, leading to venous insufficiency in the legs. Unlike lipedema, this condition typically causes pitting edema (swelling that leaves an indentation when pressed) and may be asymmetrical.
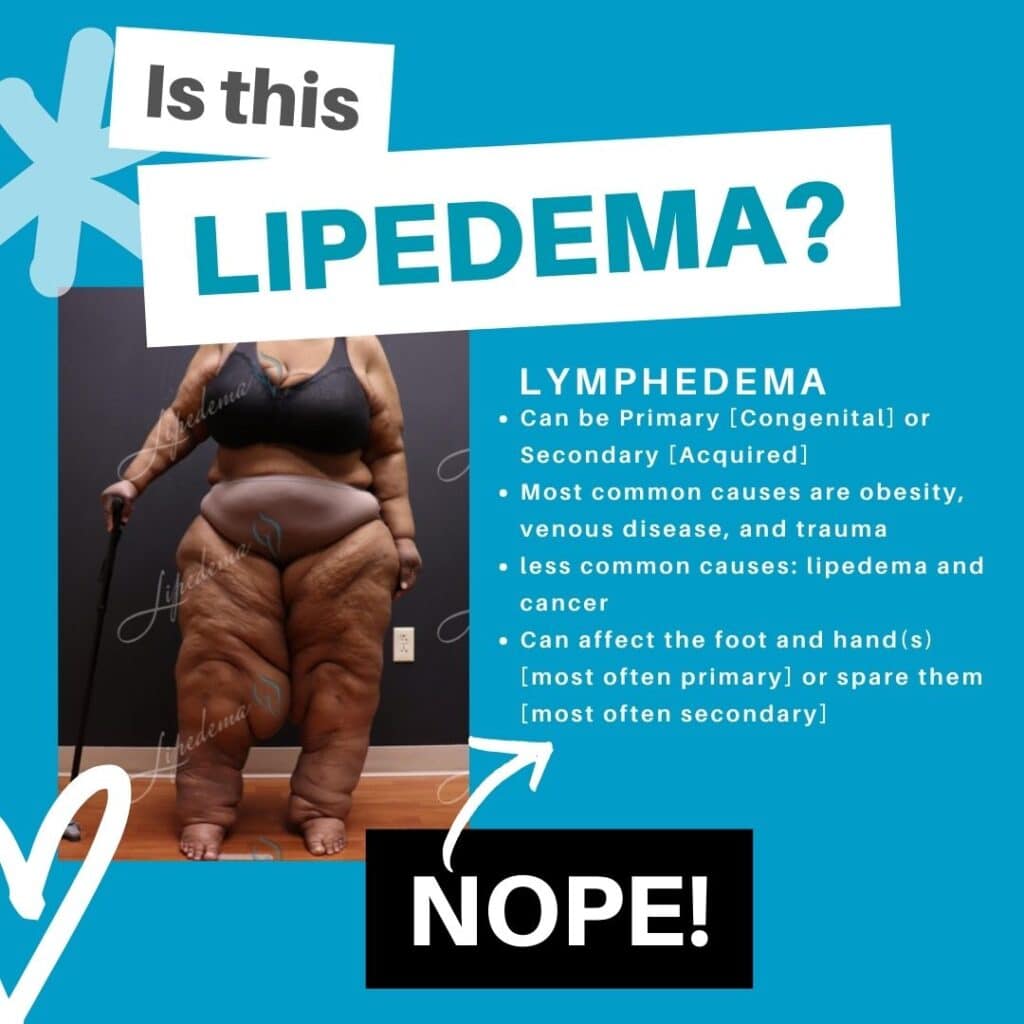
Lymphedema
Lymphedema often coexists with or is mistaken for lipedema. It involves swelling due to lymphatic fluid accumulation rather than fat accumulation. Lymphedema typically includes pitting edema, affects the feet and hands (which lipedema usually spares), and has a different texture when examined. However, the two conditions can occur together, creating a condition called lipo-lymphedema.
Endocrine and Metabolic Diseases
Obesity
Generalized obesity can be confused with lipedema, but the fat distribution and other symptoms usually differ. In standard obesity, fat distribution is more generalized throughout the body, responds to diet and exercise, and typically doesn’t cause the same degree of pain and tenderness seen in lipedema. Additionally, obesity affects the feet and hands proportionally, while lipedema characteristically spares these areas.
Prader-Willi Syndrome
Prader-Willi Syndrome is a genetic disorder that causes insatiable hunger, developmental delays, and obesity. While it can lead to significant fat accumulation in the lower body, it presents with additional symptoms not seen in lipedema, including intellectual disability, behavioral challenges, and other distinctive features.
The Importance of Differential Diagnosis
Differentiating lipedema from these lookalikes is crucial. Misdiagnosis can lead to inappropriate treatments, which may not only fail to help but could potentially cause harm. For instance, treatments beneficial for lipedema, such as certain types of massage or compression, may not be suitable for conditions like Dercum’s Disease.
When you receive the wrong diagnosis, you may undergo treatments that are ineffective or even counterproductive. This leads to wasted time, financial burden, and increasing frustration as your condition continues to progress without proper management. Accurate lipedema diagnosis in Missouri ensures you receive the right treatment from the start.
Diagnostic Steps and Testing for Lipedema Treatment Near Me
To rule out other conditions and confirm a lipedema diagnosis, healthcare providers might recommend various tests, such as:
Ultrasound and MRI: These imaging studies can check for venous insufficiency, deep vein issues, or other structural abnormalities that might explain your symptoms. They can also help visualize the pattern and distribution of fat deposits.
Lymphoscintigraphy: This specialized imaging test is specifically useful in diagnosing lymphedema. It involves injecting a small amount of radioactive material to track how lymph fluid moves through your lymphatic system. This helps differentiate lymphedema from lipedema.
Doppler Ultrasound: This test evaluates blood flow through your veins and can identify venous insufficiency or iliac vein compression that might be causing or contributing to leg swelling.
Biopsy: Rarely, but sometimes necessary to rule out other fat disorders. A tissue sample can help identify conditions like Dercum’s Disease or other lipomatous conditions.
Patients and healthcare providers must be thorough in the diagnostic process to ensure that the treatment plan is appropriate for the actual condition. At Dr. Wright’s practice in St. Louis and O’Fallon, we use a comprehensive diagnostic approach that combines clinical expertise with appropriate testing to achieve accurate diagnoses.
Why Accurate Diagnosis Matters for Treatment
Recognizing that not every case of apparent lipedema is indeed lipedema is a critical step in getting correct care. Patients who are misdiagnosed often experience frustration due to ineffective treatments and poor outcomes.
Consider what happens with different diagnoses:
- If you have lipedema but are told you simply have obesity, you might spend years trying diet and exercise programs that cannot address your actual condition. This leads to feelings of failure and worsening psychological distress.
- If you have venous insufficiency but are treated for lipedema, you won’t receive the vascular interventions that could actually resolve your swelling.
- If you have lymphedema misdiagnosed as lipedema, you might undergo liposuction that doesn’t address the underlying lymphatic dysfunction and could potentially worsen your condition.
- By understanding and identifying lipedema lookalikes, patients can be directed toward the proper care and management they truly need. Through careful examination and consideration of all possible conditions, healthcare providers can ensure accurate diagnoses and effective treatment plans, ultimately leading to better patient health outcomes.
Dr. Wright’s Expertise in Lipedema Diagnosis and Treatment
Dr. Wright is recognized as a pioneer in treating lipedema and vein disorders throughout Missouri and the Midwest. His comprehensive approach to diagnosis ensures that patients receive accurate identification of their condition before beginning any treatment protocol.
With extensive training in lymphatic disorders and years of experience specifically treating lipedema, Dr. Wright can identify the subtle differences between lipedema and its lookalikes. His diagnostic process includes:
- Detailed medical history review with attention to hormonal influences
- Comprehensive physical examination using specialized techniques
- Appropriate diagnostic testing to rule out other conditions
- Collaboration with other specialists when needed
- Clear communication about findings and treatment options
Once an accurate diagnosis is established, Dr. Wright offers cutting-edge treatment options including:
- Lymph-sparing lipedema reduction surgery
- Power-assisted liposuction (PAL) and water-jet-assisted liposuction (WAL)
- Conservative management strategies including compression therapy
- Medical weight loss programs with semaglutide and tirzepatide, when appropriate
- Treatment for coexisting conditions like venous insufficiency
His involvement with organizations like the National Lymphedema Network and AVLS Congress demonstrates his commitment to staying current with the latest advances in lipedema diagnosis and treatment.
Take the Next Step: Get an Accurate Diagnosis
If you’ve been told you have lipedema but haven’t seen improvement with treatment, or if you’re experiencing symptoms that suggest lipedema but haven’t received a clear diagnosis, it’s time to seek specialized care.
Dr. Wright’s practice in O’Fallon and St. Louis serves patients throughout Missouri who are searching for lipedema treatment and need expert evaluation. During your consultation, Dr. Wright will conduct a thorough assessment to determine whether you truly have lipedema or one of the conditions that mimics it.
You deserve an accurate diagnosis and a treatment plan designed for your specific condition. Don’t continue struggling with ineffective treatments based on an incorrect diagnosis. Contact our office today to schedule your comprehensive lipedema evaluation and take the first step toward proper care and lasting relief.
Through careful examination and consideration of all possible conditions, we can ensure you receive the right diagnosis and the most effective treatment plan for your individual situation. Your journey to better health starts with an accurate understanding of what you’re truly facing.
Dr. Wright’s practice serves patients seeking accurate lipedema diagnosis and treatment in St. Louis, O’Fallon, and throughout Missouri. With specialized expertise in differentiating lipedema from similar conditions and advanced training in lymph-sparing surgical techniques, Dr. Wright is committed to helping patients receive the correct diagnosis and appropriate care for their specific condition.