

Lipedema and cellulitis are two conditions that often coexist, causing discomfort and distress to those affected. Understanding the relationship between these two conditions and implementing prevention strategies is crucial for optimal management. Lipedema is a chronic disorder characterized by an abnormal accumulation of fat in the legs and sometimes the arms, causing pain, swelling, and tenderness.
On the other hand, cellulitis is a bacterial skin infection that can occur as a complication of lipedema due to impaired lymphatic drainage and weakened immune response. It presents with redness, swelling, and warmth in the affected area. By addressing both lipedema and cellulitis simultaneously, individuals can experience relief from symptoms and prevent recurrent infections.
Prevention strategies for lipedema-related cellulitis may include maintaining good hygiene practices, promptly treating skin abrasions or wounds, wearing compression garments, and seeking early medical intervention to address lipedema symptoms. In this article, we will explore the relationship between lipedema and cellulitis, exploring effective prevention strategies and highlighting treatment options available in St. Louis. By understanding and managing these conditions, individuals can enhance their quality of life and overall well-being.
Lipedema is a fat tissue disease, mainly affecting women, that causes an enlargement of both legs due to fat deposits under the skin. It’s characterized as a “progressive disorder,” meaning it worsens over time. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back, and it’s often misdiagnosed and incorrectly treated as general obesity.
Lipedema is a disease that leads to the excessive buildup of fat cells, primarily in the arms and legs. Going far beyond the appearance of extra pounds, those who suffer from Lipedema often have large pockets of fat on their limbs that appear disproportionate compared to the rest of the body. Medical professionals often misdiagnose and dismiss lipedema as simple obesity, leaving affected women with an endless cycle of disappointment, frustration, and pain. Lipedema does not respond to a diet and exercise routine, yo-yo dieting, or juice cleanses.
Women suffering from Lipedema often report the disease a sociated with painful symptoms that trigger difficulties in dealing with everyday activities. Excessive swelling often comes with pain, numbness, and bruising. In its advanced stages, Lipedema can impact mobility and provoke vascular and lymphatic swelling, leading to further medical complications.
Early detection of lipedema is crucial for timely intervention and management. Several signs and symptoms can indicate the presence of lipedema. Initially, these symptoms may be subtle, but they become more evident as the condition progresses. Common indicators of lipedema include symmetrical swelling in the legs, unexplained bruising, heaviness and tenderness in the affected limbs, and a lower body size disproportionate to the upper body. In advanced stages, the skin may develop pearl-sized lumps, which can grow larger and resemble walnuts or plums.
Diagnosing lipedema can be challenging due to a lack of awareness among healthcare professionals. Many patients are misdiagnosed with obesity, leading to delayed treatment and unnecessary fat-shaming. To ensure accurate diagnosis and appropriate treatment, it is crucial to seek the expertise of a specialist familiar with lipedema. Early diagnosis allows for timely intervention and improves the chances of successful treatment outcomes.
Effective treatment strategies are available for individuals with lipedema. Lymphatic support, such as complete decongestive therapy, can help manage the symptoms of lipedema. Additionally, specialized suction lipectomy, a surgical procedure, can remove diseased lipedema fat while preserving lymphatic channels. This surgical intervention not only enhances the patient’s quality of life but also improves their self-confidence by restoring a more proportionate appearance to the lower body.
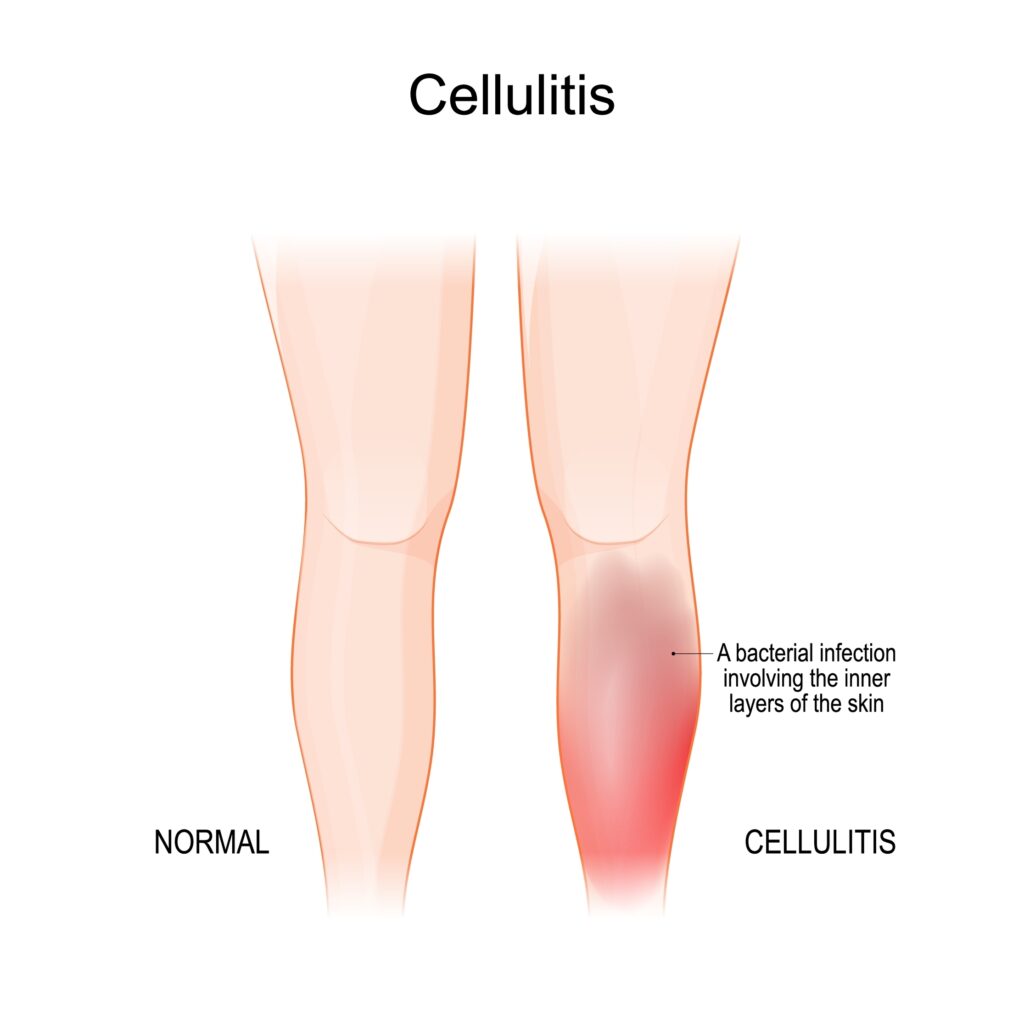
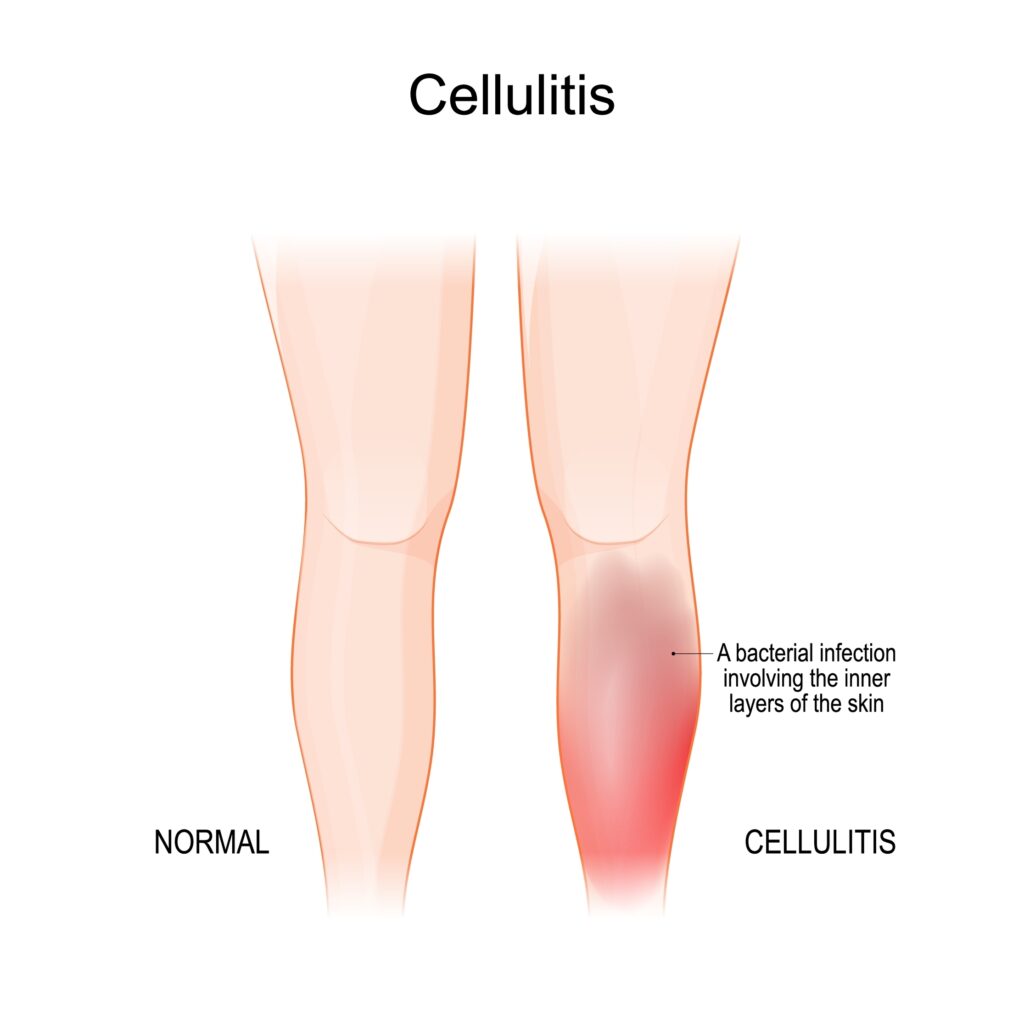
Cellulitis is a skin infection caused by bacteria that infiltrate the deep layers of the skin through breaks such as cuts or scratches. Common symptoms of cellulitis include redness, swelling, pain, tenderness, and the development of blisters. It is essential to note that cellulitis is not a direct symptom of lipedema but can arise due to the underlying condition.
While cellulitis is not a direct symptom of lipedema, individuals with lipedema are more susceptible to developing cellulitis due to factors such as poor circulation, lymphatic dysfunction, and chronic edema. Lipedema can compromise the lymphatic system’s ability to fight infections, increasing the risk of cellulitis. Therefore, it is essential to understand the relationship between lipedema and cellulitis and take preventive measures to mitigate the risk.
Preventing cellulitis in individuals with lipedema involves a multifaceted approach. It is crucial to manage the underlying risk factors that contribute to the development of cellulitis, such as chronic edema, venous disease, dermatomycosis, and obesity. By actively addressing these risk factors, the likelihood of recurrent cellulitis episodes can be significantly reduced. Additionally, non-antibiotic preventive measures, such as daily wound care, the use of protective creams and bandages, regular inspection of the feet, and maintaining good skincare practices, play a crucial role in preventing cellulitis.


Compression therapy has emerged as a beneficial approach for managing lipedema symptoms and reducing the risk of cellulitis. Compression garments, such as stockings or bandages, can help alleviate pain, reduce swelling, and improve lymphatic circulation in individuals with lipedema. These garments apply pressure to the skin and veins, promoting the clearance of lymph fluid and reducing chronic edema. Additionally, pneumatic compression pumps, which mimic manual lymphatic drainage techniques, can be used as an at-home treatment option to improve lymphatic flow and prevent fluid buildup in the affected limbs.
If cellulitis does occur in individuals with lipedema, prompt medical attention and appropriate antibiotic treatment are crucial. Cellulitis can cause severe complications and lead to further damage to the lymphatic drainage routes, exacerbating the swelling and long-term management of lipedema. Therefore, it is essential to seek immediate medical assistance if any symptoms of cellulitis, such as redness, warmth, pain, or fever, arise. Following the prescribed antibiotic treatment and taking necessary precautions, such as removing compression garments until the area heals, can help manage cellulitis effectively.
Raising awareness about lipedema is essential to ensure accurate diagnoses and appropriate treatment for affected individuals. Lipedema support organizations and online communities can provide valuable resources, information, and emotional support to individuals living with lipedema. By connecting with others who share similar experiences, individuals with lipedema can find solace, gain knowledge, and navigate their journey toward better health.
Lipedema is a prevalent adipose tissue disorder that affects a significant number of women worldwide. While cellulitis is not a direct symptom of lipedema, individuals with lipedema are more susceptible to developing cellulitis due to factors such as poor circulation and compromised lymphatic function. Preventive measures, such as managing underlying risk factors, utilizing compression therapy, and practicing good skincare, can significantly reduce the risk of cellulitis in individuals with lipedema. By increasing awareness, promoting early diagnosis, and providing appropriate treatment, we can improve the quality of life for individuals living with lipedema and mitigate the risk of cellulitis in this population. Dr. Wright and his team provide comprehensive treatment plans that consider a patient’s complete medical profile. If you’re looking for solutions to treat symptoms of Lipedema and/or cellulitis, contact us to set up an initial consultation.
Chronic swelling (also referred to as “edema”) in the legs is a risk factor for eventually developing cellulitis. A recent study showed that swelling of the legs from any cause leads to an increased risk for leg skin infections or cellulitis. For women suffering from Lipedema, this can add insult to injury in an already debilitating disease accompanied by sensitive and easily bruised skin. If left untreated, cellulitis can move into the lymph nodes and bloodstream and require more serious medical treatment. Symptoms of cellulitis may include the following:
Today, most doctors recommend conservative and preventative measures, such as daily washing of wounds or cuts that could be infiltrated by bacteria, and the application of protective creams, ointments, and bandages when necessary to surface wounds or extremely dry, flaky skin. Preventative medications, such as antibiotics, may be recommended in some instances where patients experience several recurrences of cellulitis.
For people with poor circulation – such as diabetics or women with Lipedema or Lymphedema, additional precautions for avoiding skin injury are recommended, but overall are still conservative and focus on healthy and consistent skincare. For example, the health providers at the Mayo Clinic recommend you inspect your feet daily, to check for signs of injury or infection early on, moisturizing skin regularly to avoid dryness or cracks, trimming finger and toenails with great care to avoid injuring the skin and wearing clean and protective footwear and gloves often.
Like Lipedema, there’s a lot we still don’t know about cellulitis; we know it can be caused by several types of bacteria infecting deeper layers of the skin, we know that it causes swollen, red, painful areas in the skin, and we know it commonly affects the feet and lower legs. But we don’t know how the bacteria gets into the body for many people affected. And new studies suggest something else we did not know previously – compression therapy may help prevent this painful condition.
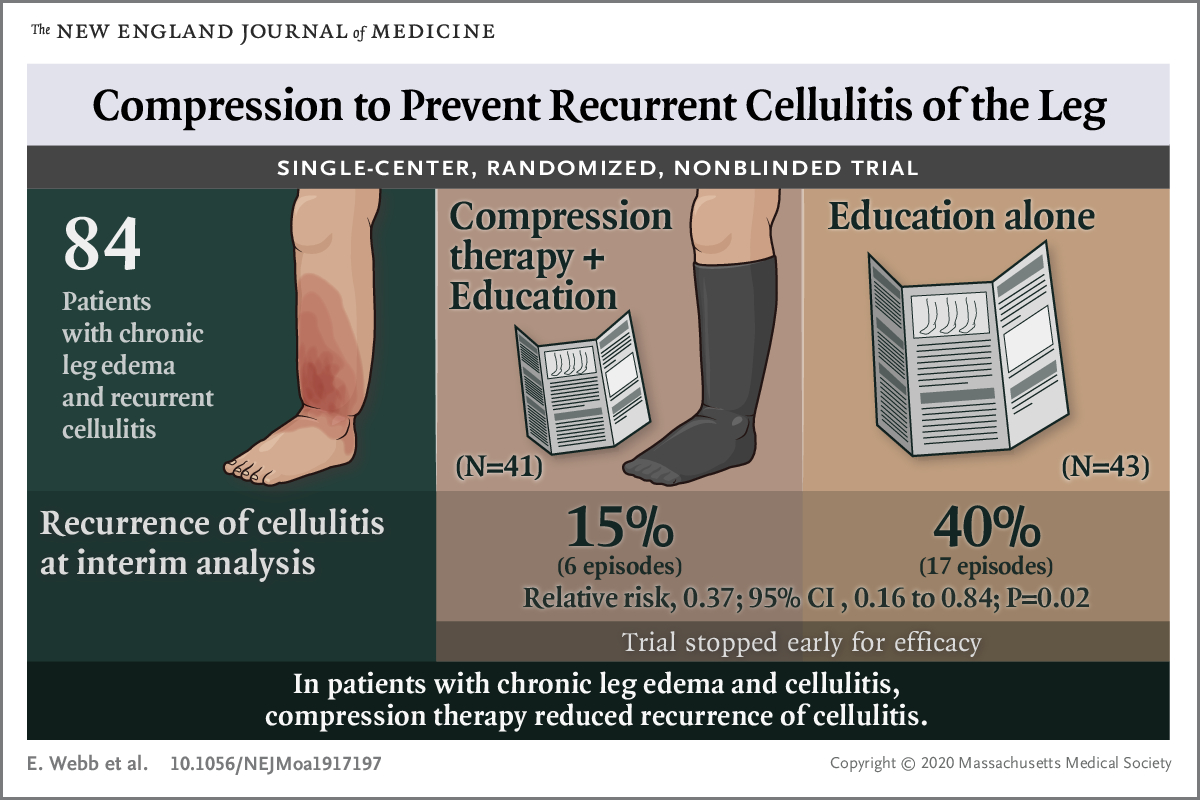
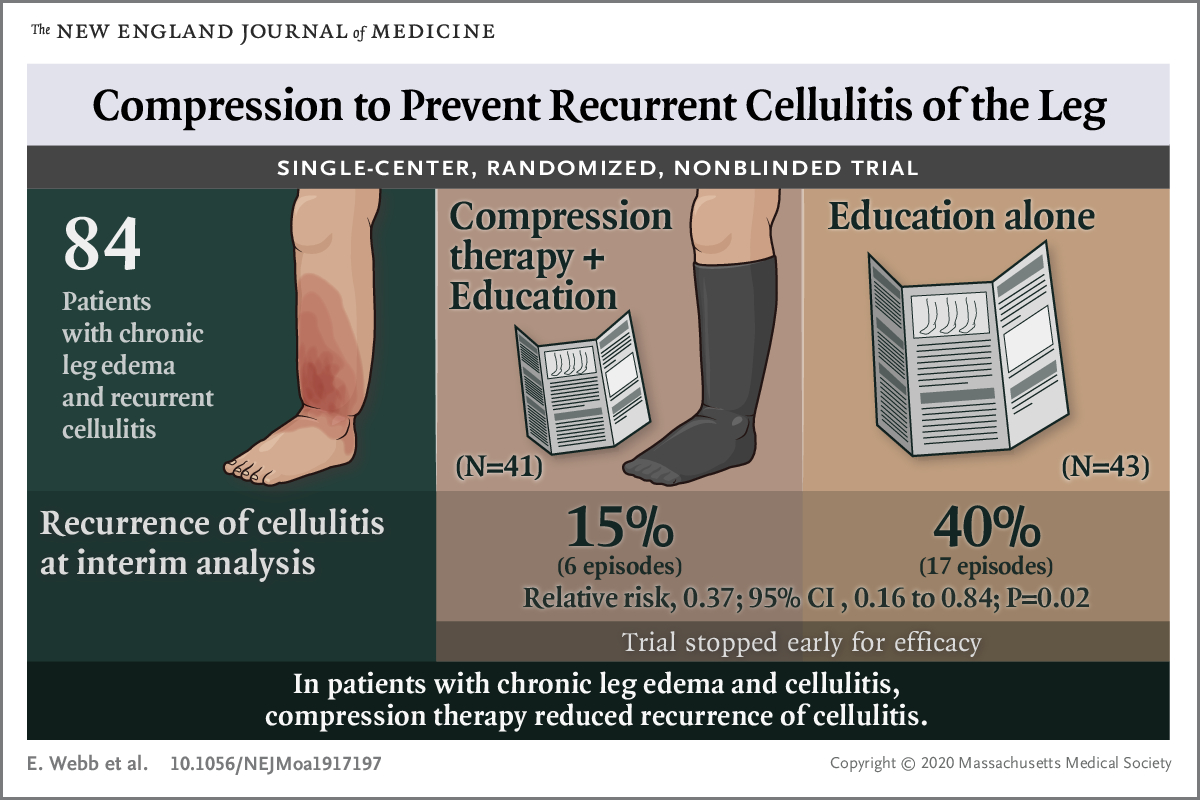
Overall, the quality of life in both groups was the same, and there weren’t drastically different experiences between group one and group two. However, the group who received both therapy and cellulitis prevention education experienced only 6 new cases of cellulitis, while the second group experienced 17 cases. While the study was small, and additional studies are needed, early indications suggest compression therapy will result in lower recurrence of cellulitis than education and conservative treatments alone. We have known for years that people with lymphedema have an increased risk for cellulitis and they benefit from compression. However, this study showed leg swelling from any cause puts affected individuals at risk for infections, and that compression helps reduce this risk.
For patients with Lipedema, there are many reasons to consider using compression garments or compression pumps. For individuals who have lipedema, lymphedema, or lipo-lymphedema, compression garments are often used to assist the lymph circulation by increasing the pressure in the tissue to propel lymph fluid through the body. Lymphedema causes excess fluid to become trapped in the extremities, especially the legs, and compression garments put pressure on the skin and veins, helping them clear lymph and decongest. If we can utilize the garments to decrease the levels of chronic edema, we may also decrease the chances of developing cellulitis.
Compression garments can help reduce pain and heaviness felt in the limbs from fat disorders (such as lipedema) by decreasing swelling in the fat and throughout the limbs. Compression may also reduce the rate at which the fat cells grow, and help to prevent fat disorders from progressing to more serious stages. In other words, compression can be one of the best treatments for lipo-lymphedema or fat caused by lymphatic diseases, in addition to cellulitis prevention.
Another option patients have to manage their own symptoms at home is pneumatic compression pumps. Pneumatic compression pumps are a great at-home solution for patients suffering from lipedema or lymphedema, and potentially for cellulitis prevention. Compression pumps are devices that mimic the massage techniques used in manual lymphatic drainage. An intermittent pneumatic compression device (IPC) is worn on the affected limb and activated to help push retained fluids back towards the core of the body. These devices let patients who may have difficulty or are unable to visit a doctor’s office often still find relief from their symptoms.
If you have compression stockings but they aren’t providing enough relief, an intermittent pneumatic compression device can help you get daily treatment. These treatments are very effective at treating extreme levels of swelling, and IPC devices help patients to continue their treatment at home and keep their lymph fluid from rebuilding in the affected limbs. As we continue to monitor the development and new studies related to how these practices may help prevent the recurrence of cellulitis, we will update the data here as well.
You can read more about compression garments and compression pumps here. The full study is below.
NEJM Compression Cellulitis Swollen Legs