

June is a significant month for the Lipedema community as it marks Lipedema Awareness Month, with World Lipedema Day celebrated on June 11. This month is dedicated to increasing awareness about lipedema, a chronic condition that affects millions of women worldwide. Despite its prevalence, lipedema remains underdiagnosed and misunderstood. At Lipedema Surgical Solutions, we are committed to spreading awareness, educating the public, and supporting those affected by lipedema.
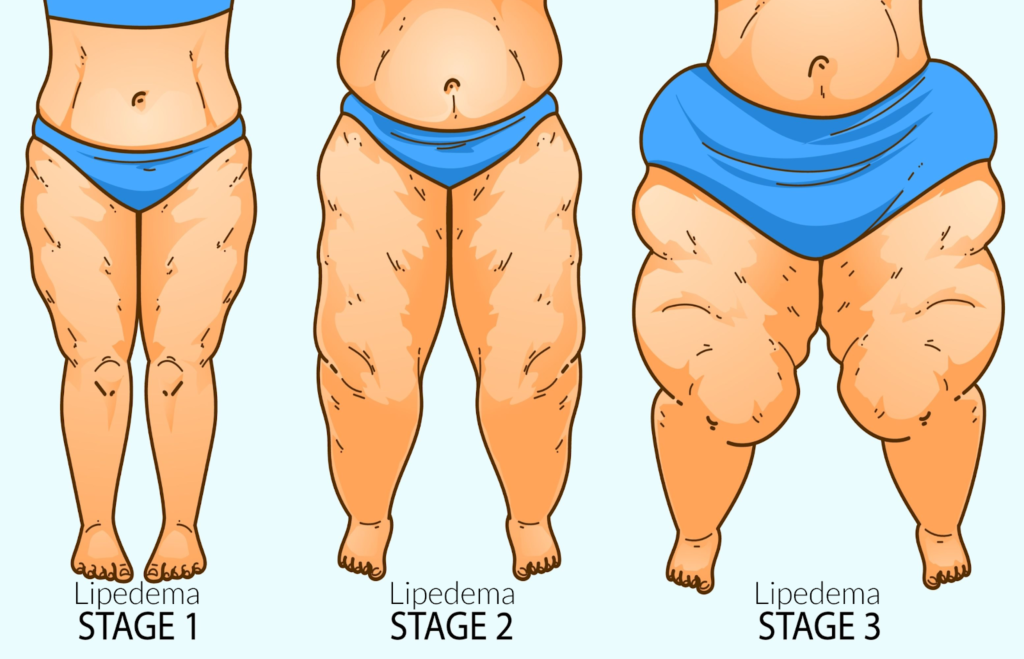
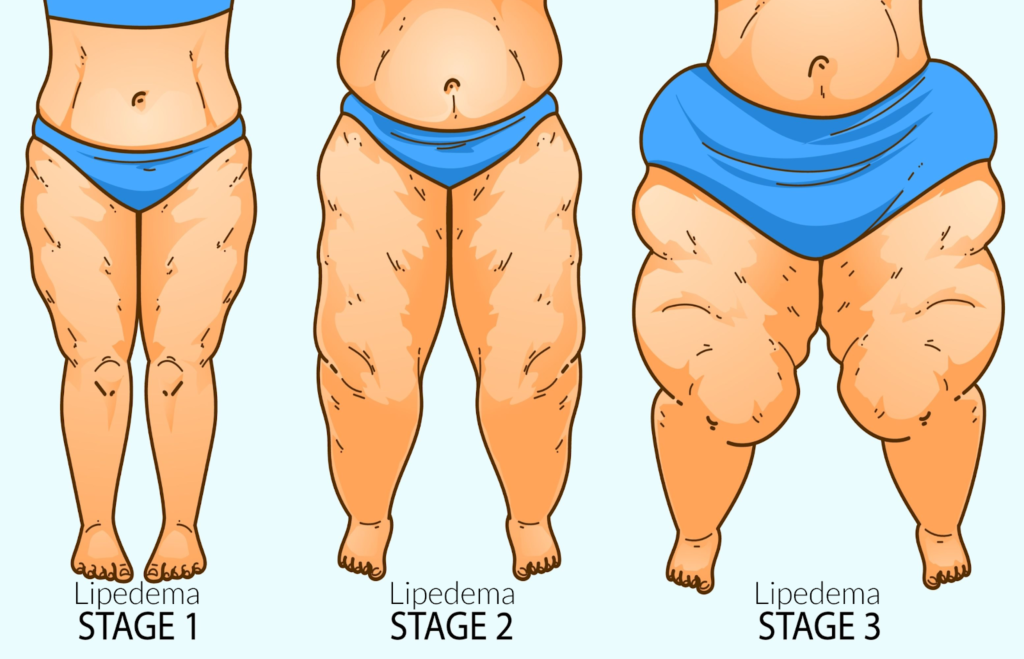
Lipedema is a chronic condition characterized by the abnormal and symmetrical accumulation of subcutaneous adipose tissue [fat] in the legs, arms, and sometimes other body parts. Unlike ordinary obesity, the fat deposits in lipedema are painful or tender and do not respond well to conventional diet and exercise, often remaining unchanged even as other body fat decreases. The condition typically progresses through stages, from mild enlargement of the limbs to more severe cases where mobility is significantly affected. Lipedema is also marked by a tendency to bruise easily and may include symptoms such as fibrosis, which is a thickening and hardening of tissue. While it is believed to have a genetic component, lipedema almost exclusively affects women and is often linked to hormonal changes associated with puberty, pregnancy, or menopause. Coexisting conditions such as lymphedema, swelling due to lymph fluid buildup, and venous insufficiency are common.


Lipedema is often misdiagnosed as obesity or lymphedema due to its similar appearance. This misdiagnosis can delay proper treatment and exacerbate symptoms. The lack of awareness among healthcare professionals and the general public contributes to the underdiagnosis of lipedema. Many women struggle for years without receiving a correct diagnosis, leading to frustration and worsening health outcomes.
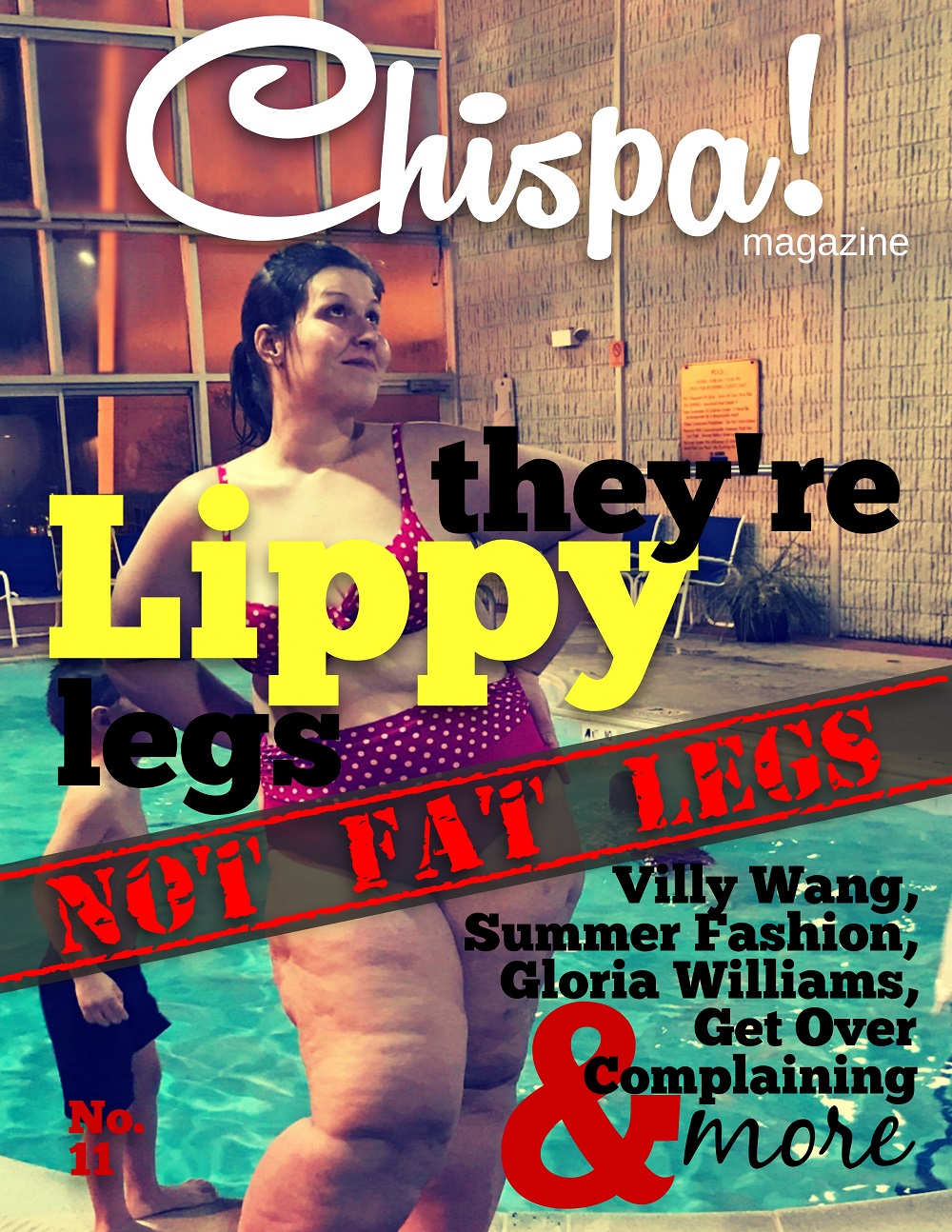
Awareness and recognition of lipedema is poor in the public and among medical professionals, which leads to some women who have lipedema not being diagnosed with lipedema. The opposite can occur. Not everyone with large legs and ankle cuffs and who appears to have lipedema disease suffers from it. Several other conditions and diseases can mimic the appearance of lipedema, making accurate diagnosis essential for effective treatment. Misdiagnosis of lipedema leads to improper treatment, so it is important to be careful and thorough.
Women with lipedema can take several steps to spread awareness and advocate for themselves:
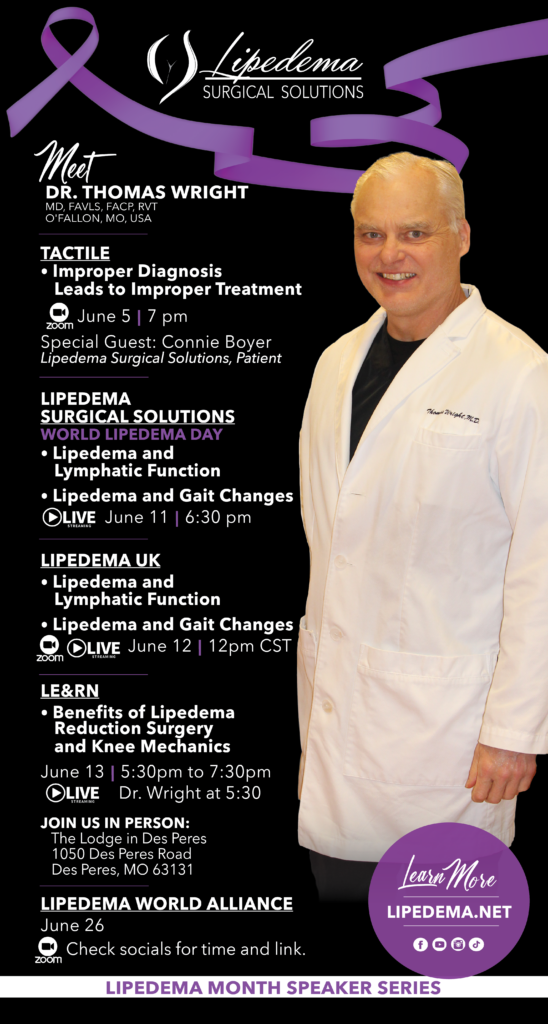
Join Dr. Wright this June for informative events to foster a greater understanding of lipedema and its treatment. These events are an excellent opportunity to learn from experts and connect with community members.
Lipedema.net is a comprehensive resource for anyone seeking detailed information about lipedema. The website features:
Dr. Wright’s YouTube channel, Lipedema Info, offers:
The Lipedema Group – Lipedema.net on Facebook is a supportive community offering:
Dr. Wright’s Instagram page, @lipedemasurgicalsolutions, provides:
Dr. Wright’s Pinterest page, Laser Lipo Vein, offers:
Living with lipedema can be challenging, but with the right resources and support, managing the condition becomes significantly easier. From comprehensive information hubs like Lipedema.net to engaging social media platforms, numerous avenues exist for education, support, and community. Dr. Wright’s dedication to providing resources highlights the growing awareness and support for those battling lipedema.
Remember, while online resources are invaluable, they should complement, not replace, professional medical advice. Always consult with healthcare professionals for personalized medical guidance and treatment plans.
If you or someone you know is struggling with symptoms of lipedema, don’t hesitate to seek help. Contact Lipedema Surgical Solutions online for guidance on understanding lipedema, obtaining a proper diagnosis, and exploring treatment options. Our team, led by Dr. Wright, is dedicated to providing comprehensive care and support for women with lipedema.
Keywords: Lipedema, Lipedema Treatment, St. Louis MO Lipedema Specialists, Dr. Wright St. Louis, Lipedema Awareness Month, World Lipedema Day
By spreading awareness and advocating for proper diagnosis and treatment, we can improve the lives of those affected by lipedema. Let’s work together to make a difference this Lipedema Awareness Month and beyond.
Lipedema is a chronic and progressive disease that primarily affects women. It is often misdiagnosed as obesity or primary lymphedema, leading to a lack of understanding and appropriate treatment options. Lipedema’s physical and psychological consequences significantly impact the quality of life of those who suffer from it. This comprehensive guide will delve into women’s experiences with lipedema, highlighting their challenges and the importance of providing adequate care and support.
Lipedema is characterized by the abnormal deposition of subcutaneous adipose tissue, primarily in the lower body parts, such as the buttocks and legs. This adipose disease is of unknown etiology and tends to manifest during or after puberty, although it can also occur in connection with pregnancy or menopause. The accumulation of fat and fibrous tissue leads to bilateral swelling and enlargement, causing discomfort, bruising, severe pain, and limited mobility. Unfortunately, the progression of lipedema varies greatly, making it challenging to predict and control.
Conservative therapy, which focuses on patient education, weight control, manual lymphatic drainage therapy, and compression therapy, is commonly used to manage lipedema. Surgical interventions, such as liposuction, may be necessary in some cases. However, there are no easy solutions for treating lipedema, and further research is needed to develop more effective interventions.
Living with lipedema has a profound effect on the quality of life of women. The physical symptoms, including pain, fatigue, and limited mobility, significantly hinder their daily activities and overall well-being. Women with lipedema often describe their bodies as burdensome, feeling controlled and hindered by the swelling and pain they experience. The constant pain and discomfort can lead to exhaustion and a sense of helplessness.
Furthermore, the psychological impact of lipedema should not be overlooked. Women with lipedema often face fat-shaming and negative judgments from others, which affects their self-esteem and body image. They may feel unattractive and struggle with intimacy and sexual activity. The changes in their bodies, such as the appearance of loose and bumpy skin, pose additional challenges regarding hygiene and self-care. The lack of understanding and support from healthcare professionals further exacerbates their emotional distress.
Women with lipedema frequently seek medical help to address the changes in their bodies and the increasing pain they experience. However, obtaining an accurate diagnosis can be a lengthy and frustrating process. Many women have encountered healthcare professionals who lack knowledge about lipedema, leading to misdiagnosis or dismissive attitudes. Instead of receiving appropriate care, they are often advised to engage in weight loss exercises or visit physiotherapists and dietitians without addressing the underlying lipedema.
Women with lipedema often take matters into their own hands, researching and gathering information to understand their condition better. Some find the diagnosis themselves and present it to their doctors, only to face skepticism and hurtful comments. The lack of awareness and understanding among healthcare professionals contributes to feelings of isolation and a lack of support for women with lipedema.
Receiving a diagnosis of lipedema should be a turning point towards appropriate care and treatment. However, many women find themselves at a dead end. Despite having a confirmed diagnosis, they struggle to access the care they need. The limited knowledge about lipedema among healthcare professionals hinders the development of effective treatment strategies. Women with lipedema often have to fight for liposuction surgery, which can be crucial in managing the disease. They may also seek treatment abroad, incurring additional financial burdens.
The lack of guidance and support in medical decision-making further compounds the challenges faced by women with lipedema. They often feel alone, left to navigate their treatment options without sufficient professional advice. Some women have found supportive doctors who listen to their concerns and collaborate with them to develop appropriate treatment plans. However, these rare instances highlight the urgent need for increased awareness and knowledge among healthcare professionals.
Pain and fatigue are two significant symptoms that women with lipedema experience daily. The pain associated with lipedema is often described as aching, heavy, and unpredictable. It can worsen with movement and become stabbing in nature. Women with lipedema express feelings of exhaustion and describe the constant pain as debilitating. The invisible nature of their symptoms makes it challenging for others to understand and empathize with their experiences.
Fatigue, another common symptom of lipedema, further adds to the physical and emotional burden. Women with lipedema describe feeling constantly tired, which affects their ability to engage in daily activities. The lack of understanding and validation of their pain and fatigue by others, including healthcare professionals, leads to feelings of neglect and frustration.
Encounters with healthcare professionals play a crucial role in the lives of women with lipedema. Unfortunately, many women feel that their experiences are not taken seriously, resulting in a lack of dignity and respect. Healthcare professionals’ skepticism and dismissive attitudes toward their pain and symptoms contribute to feelings of violation and humiliation. Women with lipedema emphasize the need for healthcare professionals to listen, understand, and acknowledge their experiences.
Creating a supportive healthcare environment requires healthcare professionals to educate themselves about lipedema and its impact on patients’ lives. By validating women’s experiences and providing appropriate care, healthcare professionals can alleviate the emotional distress associated with lipedema. Collaborative decision-making and the involvement of specialists can also contribute to better treatment outcomes and improved quality of life.
Living with lipedema often leads to negative body image and decreased self-esteem. Women with lipedema may feel unattractive and struggle with self-acceptance. The changes in their bodies, such as the irregular distribution of fat and the appearance of cellulite, contribute to dissatisfaction and insecurity. The societal pressure to conform to narrow beauty standards exacerbates these negative feelings.
However, some women find solace in supportive relationships, particularly with their partners. Feeling desired and loved by their partners is essential for their overall well-being. The challenges of intimacy and sexual activity due to lipedema can strain relationships, but open communication and understanding can help foster intimacy and emotional connection.
Education and support play a vital role in empowering women with lipedema. Access to accurate information about the condition, treatment options, and self-care strategies can help women make informed decisions about their health. Support networks, both online and offline, provide a sense of community and understanding. Connecting with other women with similar experiences can offer emotional support and practical advice.
Additionally, psychological support is crucial for women with lipedema. Counseling or therapy can help address body image concerns, manage emotional distress, and enhance overall well-being. By addressing lipedema’s physical and emotional aspects, women can regain control over their lives and improve their quality of life.
The experiences of women with lipedema highlight the urgent need for change in healthcare systems and increased research on the condition. Healthcare professionals must be educated about lipedema to provide appropriate care and support. Developing evidence-based treatment guidelines and exploring novel interventions are essential to improve outcomes for women with lipedema.
In conclusion, lipedema has a significant impact on the quality of life of women who live with this chronic and progressive disease. Their physical and psychological burdens require healthcare professionals to approach lipedema with empathy, understanding, and respect. By providing adequate care and support, we can empower women with lipedema to navigate their journey towards better health and well-being.
Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. Sufferers living with lipedema experience easy bruising and tenderness, pain in the affected areas, and significant disability in daily life. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back. Little is known about the disorder, and it’s often misdiagnosed and incorrectly treated as general obesity.
For anyone affected, diet and exercise alone aren’t effective ways to get rid of Lipedema fat; Lipedema fat has proved relatively immune to these lifestyle changes and won’t budge. While women are likely to experience some weight loss with a healthy diet and regular exercise routines, weight loss is usually mostly loss of non-Lipedema fat. In these instances, the painful, stubborn fat remains. This cycle becomes a difficult one to break for those with the disorder: Yo-yo dieting leads to more weight gain. More weight gain leads to increased pain and disability. Increased pain and disability make it more challenging to manage mobility and secondary obesity increases. Lipedema fat also appears to be relatively resistant to bariatric surgery, meaning many women are undergoing dangerous surgeries without experiencing the intended benefit of significant loss of lipedema fat.
Unlike common obesity, Lipedema is comprised of fat deposits and swelling that typically does not affect the feet or hands; it’s as if patients are wearing a tight bracelet or rope at their wrists or ankles that causes every above to swell and everything below to remain unaffected. At more progressive stages, the swelling increases and leads to a diagnosis of lymphedema, which makes it even less likely Lipedema is diagnosed and treated promptly and adequately.
Despite the strong impact of Lipedema on millions of women across the world, only limited research exists to determine its cause. In many cases, the genetic background can provide some context, but enough research has yet to offer a comprehensive understanding of the disease.
Dr. Wright and his team at St. Louis Laser Lipo & Vein Center have put together a helpful list of Lipedema Do’s and Don’ts for living with this difficult disease.
Guaifenesin, best known by the brand name Mucinex©, and often prescribed as an over-the-counter expectorant to treat the common cold, may help reduce lipedema swelling and inflammation.


To our knowledge, there are no published, controlled studies showing the use of Guaifenisn to treat lipedema or lymphedema. However, there are abundant reports from clinicians and lipedema patients stating Guaifenisn helps lipedema. In our limited clinical experience, about 20 – 30 % of lipedema patients report reduced pain and/or swelling when taking this medication. Plus, there are reports of Guaifenisn being used for pain relief to treat other diseases. Guaifenesin has shown modest but significant analgesic and anti-inflammatory effects in neck and back pain and some other conditions. It is thought guaifenesin may be working as a muscle relaxant effect that occurs in these conditions. Mucinex / guaifenesin may help pain or it may work as an expectorant in lipedema tissue and thin out extracellular proteins. However, there are no studies to support these theories in lipedema.
Guaifenesin is approved for safe use at 600 mg twice a day (or 1,200 mg twice a day) for no more than 2,400 mg per day. Studies in the use of Mucinex for other medical conditions report it takes a least a week to see effects. I recommend lipedema suffers try this medication for two weeks to see if they notice any positive changes in addition to their consistent treatment plans including compression, supplements, and a healthy diet as prescribed. May not be suitable for people with a persistent cough due to asthma, bronchitis, emphysema, or smoking, or who have a cough that is producing excessive amounts of phlegm. Talk with your doctor first before using Mucinex if you are pregnant or breastfeeding.
Diosmin is a flavonoid extract made from orange peels used to treat vein disease. Diosmin helps reduce inflammation along vein walls in people with chronic venous insufficiency and it can also have very positive results for people with lipedema and lymphedema.


Benefits
In a recent case study, Diosmin had positive results when used in combination with other supplements, diet, compression, and other anti-inflammatory measures to non-surgically manage lipedema. Based on these studies, and my experience prescribing Diosmin to patients, I recommend Diosmin as part of an overall conservative management treatment plan for lipedema and lymphedema.
In the United States, Diosmin is sold under the brand name Vasculera, which is available in pharmacies by prescription from a physician. Vasculera is approved by the FDA as a medical food.
Diosmin is also available as a supplement without a prescription. We recommend Vein Formula, as we trust its formulation. Be sure to order any supplements from a reputable website for the best safety and quality. Link https://vitasupportmd.com/products/vein-formula-1000
Fat freezing—also known as cryolipolysis (or Cool Sculpting) uses cold temperature to reduce fat deposits in certain areas of the body. The procedure is designed to reduce localized fat deposits that do not respond to diet and exercise. It is not intended for people who are obese or significantly overweight. Currently, there is no published research on cryolipolysis for lipedema. Most lipedema fat is not the type of localized fat deposit for which this procedure is intended. Cryolipolysis can cause Paradoxical Adipose Hyperplasia (PAH). This condition can aggravate symptoms, and lead to worsening of lipedema.
Researchers from Stanford University found both diets improved blood glucose and led to comparable weight loss. However, this study shows keto may elevate LDL cholesterol, lacks essential nutrients, and is more difficult to maintain over time.
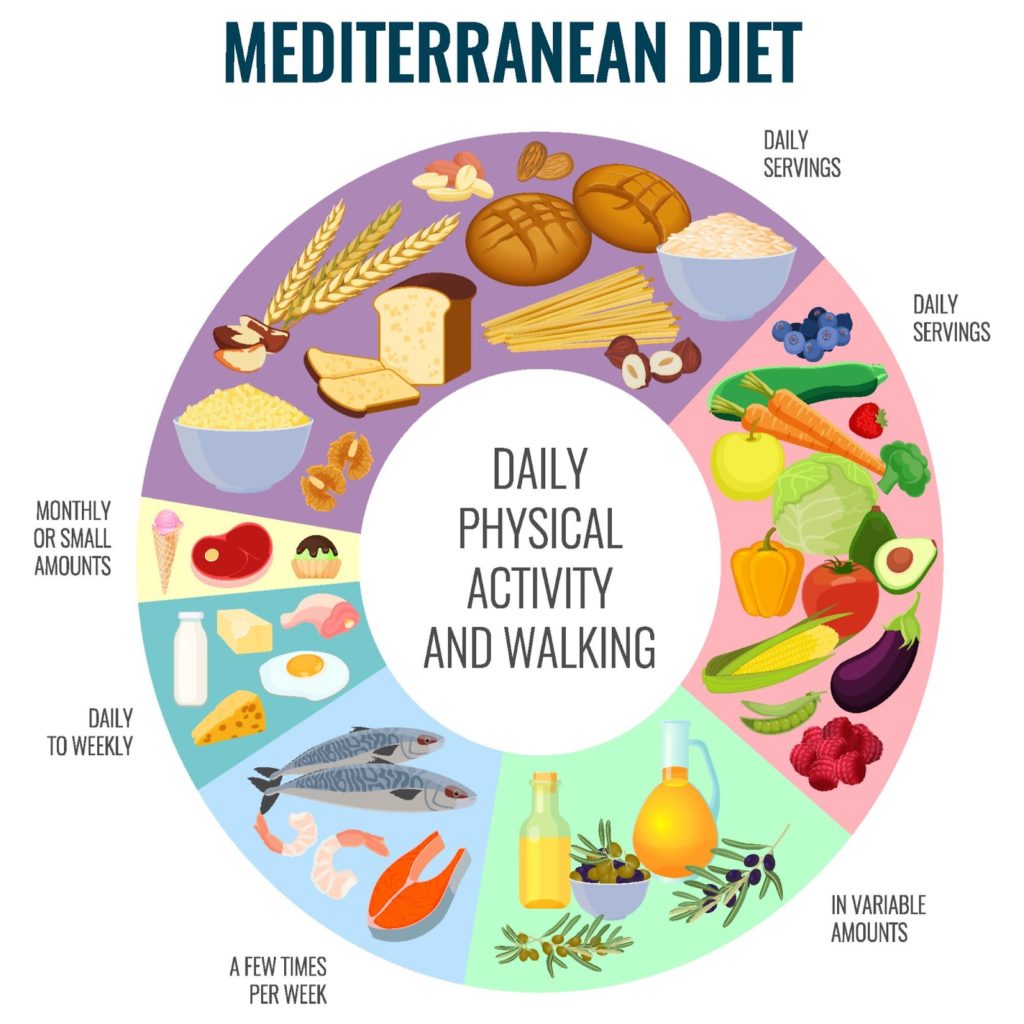
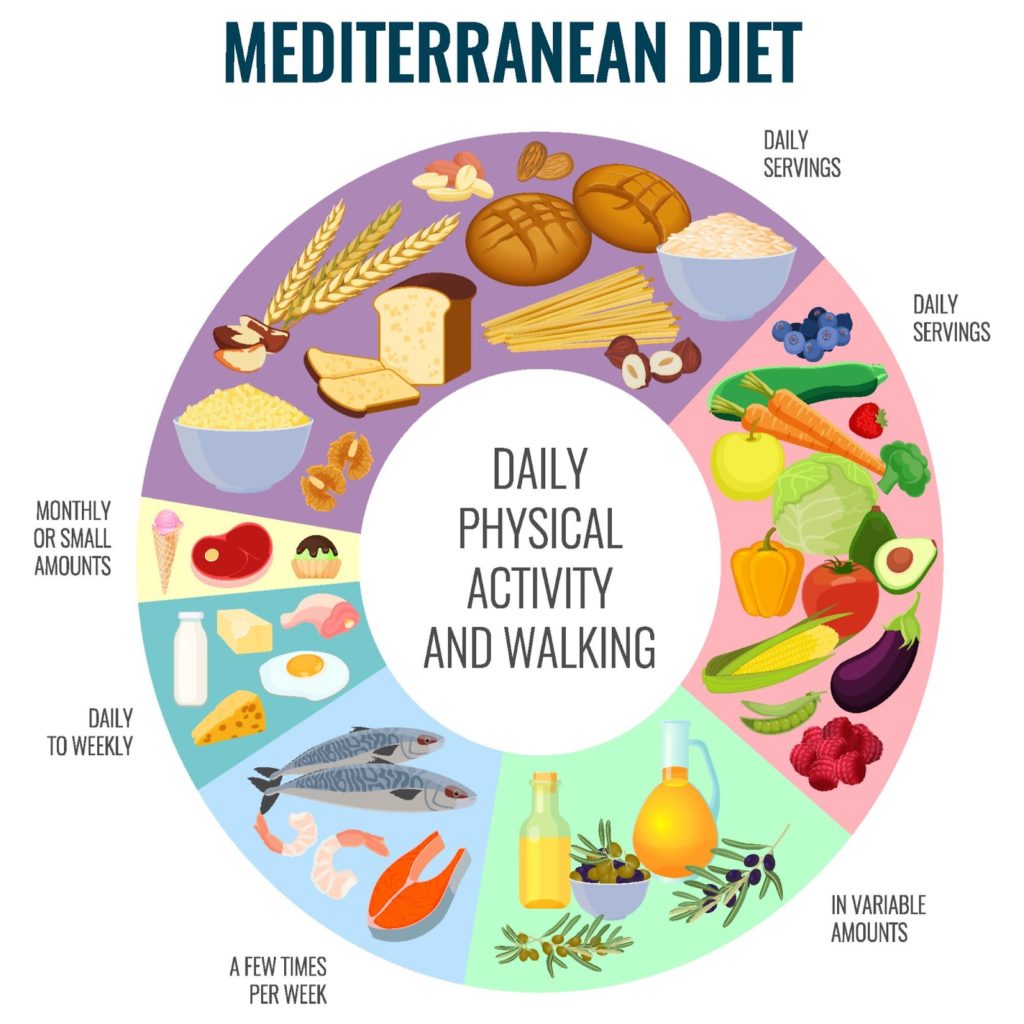
Study: During the study, 30 adults with prediabetes or type 2 diabetes followed the Mediterranean diet and the keto diet for 12 weeks each. Both diets served non-starchy vegetables and avoid added sugars and refined grains, but there are three key differences between them: the Mediterranean diet incorporates legumes, fruits, and whole grains – keto does not.
Note: Please work with a doctor or nutritionist to choose a dietary pattern that fits your needs and preferences. The potential harms of higher LDL associated with keto cannot be dismissed.
Exercising can help to activate the lymphatic drainage system in a patient’s limbs through the foot and calf muscle pump. Workouts that aren’t too strenuous help to move the excess fluids out of affected limbs, as well as reduce additional fat buildup.
The lymphatic system differs from the blood circulatory system in that it does not have a muscle “pump” to move fluids into the lymphatic system and eventually return back into circulation. Because of this, good lymph flow depends on proper joint and muscle activity. This is especially true if the lymphatic system is compromised. Individuals suffering from lipedema can receive a great benefit when engaging in diaphragmatic breathing exercises. These exercises are especially beneficial when they are combined together with other parts of a decongestive regimen.
Because fat disorders and lymphedema can often feed into one another, exercise is a great option to help combat both. With its dual purpose of clearing out excess lymph fluid and burning fat, exercise offers exactly what patients need to deal with these disorders.


The types of exercise used should be focused on the individual patient’s needs and ability. Additionally, it is important to use compression garments when exercising whenever possible. Compression garments help to promote blood circulation and lymph fluid flow, which can be severely inhibited in patients who suffer from fat disorders and lymphedema.
Even with all the challenges presented by lipedema, there are those who you can trust. Dr. Wright continues to strive for better education, research, and coverage for the lipedema community. Do not let these challenges bring you down even further; let Dr. Wright and his expert team help you to reduce the symptoms of lipedema and live your life fully! Dr. Wright can help find the right procedure to help manage your lipedema symptoms. Don’t let lipedema take over your life; contact us today!
Albert-Adrien Ramelet, MD, Pharmacologic Aspects of a Phlebotropic Drug in CVI-Associated Edema
First Published January 1, 2000
Scholar.google Diosmin Effect on Lymphatic Function
A lymphatic function of Daflon 500 mg
Int Angiol. A lymphatic function of Daflon 500mg., 1995 Sep; 14(3 Suppl 1):36-8
Recommended Sources for Diosmin: Vitasupport MD
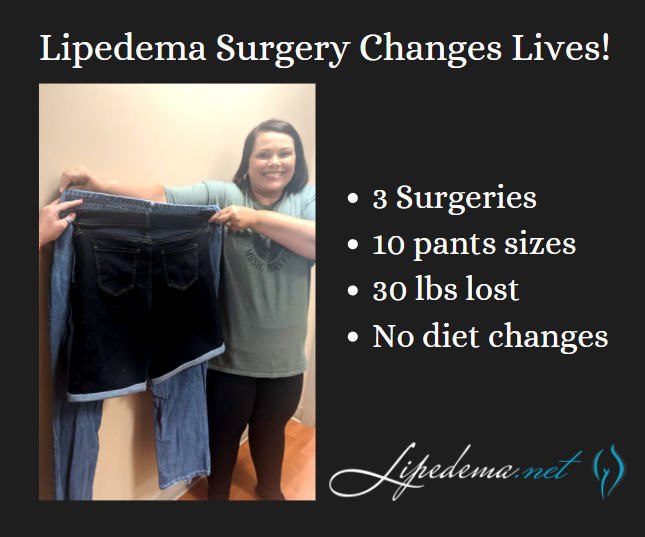
There’s nothing more satisfying and exciting for Dr. Wright and his team at Laser Lipo & Vein Center than celebrating patient wins! One of our favorite patients, Rita, spent her time in quarantine focused on getting through her lipedema surgeries, recovering safely at home, and both she and our team couldn’t be happier with her results! Rita’s experience is proof that Lipedema surgery can transform patient experiences as they walk through life (literally!) from pain and immobility to pain-free progress!
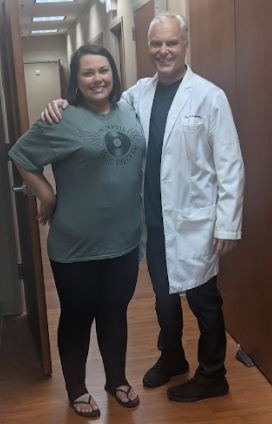
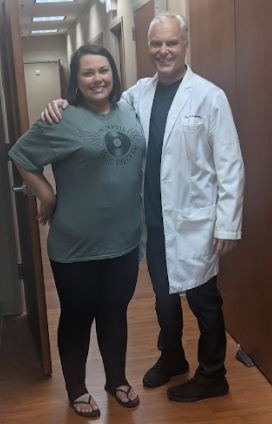
Rita has undergone three Lipedema surgeries on her legs and has seen dramatically positive results. She’s continued to follow a generally healthy diet both before and after her surgeries but did not implement any form of diet changes, so these results are primarily the outcome of her lipedema surgeries! She’s gone from a size 24 to a size 14 in jean size, lost 30 pounds, and is now more easily active and mobile day-in and day-out.
There are so many day-to-day activities that those without Lipedema wouldn’t think twice about, but patients with Lipedema struggle with and dread. Post-surgery, Rita has reported back to our office that after losing 10 pants sizes and removing the irregular lipedema fat in her lower body, she has no problems fitting into those frustrating chairs with arms on either side, she has enjoyed walking around the amusement park with her 10-year-old daughter without having to take breaks, and overall has enjoyed her active lifestyle, without the pain that used to accompany it!


Lipedema is a subcutaneous fat disease that primarily affects women. When we reference the “subcutaneous” tissue and fat, we’re referencing the layer of tissue directly under the skin.
Shockingly, Lipedema affects an estimated 17 million women across the globe. This disease affects a huge number of women, the majority of whom are still walking through their world in a lot of physical and mental pain. Lipedema is a disease that leads to the excessive build-up of fat cells, primarily in the arms and legs. Women suffering from it often have “pockets” of fat on their limbs that appear disproportionate in comparison to the rest of their bodies. This disease causes an enlargement of the legs due to deposits of fat under the skin, and typically gets worse over time, making diagnosis and treatment essential.
It’s common for women with Lipedema to have a small upper body, while their lower body is disproportionately larger (kind of like an extreme pear-shaped body). Pockets of fat develop in the affected areas and appear to bulge in and out of the top layer of the skin. This is often mischaracterized as cellulite, rather than painful lipomas.
These pockets of Lipedema fat are accompanied by painful symptoms, such as excessive swelling, pain to the touch, numbness, and very easy bruising. If my dog jumped up on my legs, it was excruciating. Everyday occurrences that most people don’t think twice about, like accidentally bumping into a table or chair, can cause deep, painful bruises.


As Lipedema progresses over time, these symptoms will continue to get worse as more Lipedema fat accumulates, and many women report that they are less and less mobile or active as time goes on. As a result, these women are stuck in a terrible cycle; they are less mobile, so they often gain weight, then it’s even more difficult and painful to be active, and the cycle goes on and on.
While many women also see weight gain in their arms, it’s common that the following areas are greatly affected:


We know that Lipedema is inherited in about 60% of women, and early studies show a genetic component is definitely at play (read more about that here!) and is the result of a malfunction of the Lymphatic System. The lymphatic system is a network of tissues and organs that help rid the body of toxins, waste, and other unwanted materials. This system transports lymph fluid throughout the body and is important for maintaining a healthy immune system. This disease affects the lymphatic system’s tiny vessels (microvessels) that cause a build-up of excess fluid around the body’s tissue cells. These tissue cells (located in the subcutaneous layers we discussed above) are then full of excess fluid, causing the swelling, soreness, bruising, and pain that many women with Lipedema report.
As researchers continue to gain understanding and genetic proof of Lipedema and differentiate it genetically from other diseases that they’re commonly misdiagnosed with, it will only become easier for women with Lipedema to get a proper diagnosis. Then, as the disease is more widely known and understood, treatments will become better and better, it will be more difficult for insurance providers to refuse coverage for treatments. Hopefully from there, more doctors will be trained in treating women with Lipedema properly, so treatments will become more accessible across the country! Read more about the first-ever Standard of Care Guidelines for Lipedema here!
There are two categories of treatment, surgical and non-surgical. Insurance providers require patients first try non-surgical treatment options before they’ll consider approving lipedema surgery, and Lipedema providers should be able to walk patients through this. While Lymph-sparing liposuction is the only treatment option that can provide permanent results by removing the lipedema fat, non-surgical options can help slow progression and are also necessary post-surgery (so it’s still important to practice them!).
To the dismay of patients, wearing medical-grade, tight compression garments 24-hours per day, seven days per week, is the key to improve circulation for the lymphatic system, making this a go-to prescription from Lipedema experts. Compression garments come in a variety of strengths and will be prescribed based on the stage and type of affected areas. The tighter the compression, the better.
A healthy and consistent lifestyle of clean eating and low-impact exercise to address obesity will also help with Lipedema. A diet focused on low-carb and low-sugar has proven successful. Low-impact exercise such as walking, water aerobics, yoga, or gymnastics has also reported success. Patients must avoid yo-yo dieting while also permanently losing or, at the very least, maintaining their weight. What works for one patient may not work for another. Diet and exercise recommendations and healthy practices are essential, but ultimately should be based on the individual with the understanding that weight gain is not an option.
Some patients opt-in to Manual Lymph Drainage massage (MLD), a gentle skin massage used to stimulate the circulation of the lymphatic system. While experts have yet to find significant evidence that MLD helps with Lipedema directly, some patients prefer it for its “hands-on” nature to addressing their symptoms.
For patients in the later stages of Lipedema, the pain and disruption to daily life are not permanently addressed with compression garments, diet, and exercise alone. Traditional liposuction that uses general anesthesia, radio frequencies, ultrasound, or lasers are possibly damaging to the lymphatic vessels, and as such are not an option for Lipedema patients, either. However, Lymph-sparing liposuction is safe, using surgical techniques that avoid lymphatic injury, and the use of local tumescent anesthesia reduces the risk of complications. Generally, the most painful areas should be treated first, starting high on the legs and then moving downward in future surgeries.
Even with all the challenges presented by lipedema, there are those who you can trust. Dr. Wright continues to strive for better education, research, and coverage for the lipedema community. Do not let these challenges bring you down even further; let Dr. Wright and his expert team help you to reduce the symptoms of lipedema and live your life fully! Dr. Wright can help find the right procedure to help manage your lipedema symptoms. Don’t let lipedema take over your life; contact us today!
After receiving the diagnosis of Lipedema, all heads turn to the Internet for the glory answers of what, how, and the why. And of course, who else? You view minimal reporting from doctors and remind yourself, “That’s probably why my family doctor thought I had painful cellulite.” Yes, you are shocked, and agree to never return to a doctor who believes in such falseness. By the way, we did our research and indeed, there is no such thing as painful cellulite.